>Corresponding Author : Ziad Imane
>Article Type : Case Report
>Volume : 4 | Issue : 9
>Received Date : 23 May, 2024
>Accepted Date : 06 June, 2024
>Published Date : 11 July, 2024
>DOI : https://doi.org/10.54289/JCRMH2400146
>Citation : Fadwa A, Imane Z, Ali S, Boufettal H, Mahdaoui S, et al. (2024) Synchronous Endometrial and Ovarian Cancers: One Case Report. J Case Rep Med Hist 4(9): doi https://doi.org/10.54289/JCRMH2400138
>Copyright : © 2024 Fadwa A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access
1Resident Physician, Department of Gynecology and Obstetrics, at Ibn Rochd University Hospital, Casablanca, Morocco
2Professor in the Department of Gynecology and Obstetrics at the Ibn Rochd University Hospital in Casablanca, Morocco
*Corresponding author: Ziad Imane, Resident Physician, Department of Gynecology and Obstetrics, at Ibn Rochd University Hospital, Casablanca, Morocco
Abstract
Synchronous ovarian and endometrial cancer (SEOC) is a rare instance butit accounts for 50–70% of all synchronous female genital tract tumors We report a case of a woman that was diagnosed with SEOC and underwent surgical staging. Patients with synchronous cancers have better prognosis than those with single disseminated cancer. Their detection in a relatively early stage suggests diagnosis may be facilitated by early symptoms from the endometrial carcinoma, and that these lesions are biologically of relatively low grade. The first symptoms reported by our patients and the course of the disease were concordant with data from the literature.
Keywords: Synchronous Endometrial and Ovarian Carcinoma; Endometrial Cancer; Ovarian Carcinoma
Abbreviations: SEOC: Synchronous Endometrial and Ovarian Cancers, EC: Endometrial Cancer, OC: Ovarian Cancer
Introduction
Synchronous malignancies in the female genital tract are very rare entities (0.5-1.7%). Synchronous endometrial and ovarian cancers (SEOC) are the most common, with a frequency of 5% for primary endometrial tumors and 10% for primary ovarian tumors [1]. SEOCs are characterized by the histological dissimilarity of the tumors, the absence of myometrial invasion or only superficial invasion of the endometrial cancer, the absence of invasion of the vascular space of the endometrium and the ovarian tumor, and the absence of other signs of spread, unilateral ovarian tumor, ovarian tumor in the parenchyma and without involvement of the ovarian surface, dissimilarity of molecular or karyotypic genetic abnormalities in the tumors, and different ploidy of the tumor DNA [2,3]. We report the case of a 53-year-old patient with no particular pathological history who presented with synchronous tumors of the endometrium and ovary.
Case Report
The patient was 53 years old, divorced, gravida 3, para 3, she had given birth by vaginal root, with no particular pathological history. She presented herself to the clinic with postmenopausal metrorrhagia associated with chronic pelvic pain which had been evolving for a month, with no urinary or digestive functional signs. The patient's general condition remained unchanged.
On clinical examination, the patient's general condition was good, and her conjunctivae were normo-colored. Speculum examination showed a normal cervix with no endo-uterine bleeding and clean vaginal walls. On vaginal touch and abdominal palpation, the uterus was of normal size with no latero-uterine mass.
A pelvic ultrasound was ordered, which revealed an ultrasound appearance associated with a tissue-like cervical-isthmic uterine formation (Figure 1).

Figure 1. Ultrasound appearance of the mass
A pelvic MRI was subsequently performed and showed a suspicious-looking endometrial thickening classified as FIGO stage Ib and a suspicious-looking left ovarian solid cystic mass (Figure 2).

Figure 2. Pelvic MRI findings
The CA 125 came back negative at 77 IU/ml and the cervical smear showed no sign of malignancy.
The patient subsequently underwent an enlarged total hysterectomy without adnexal preservation, pelvic lymph node dissection, omentectomy and peritoneal lavage fluid sampling.
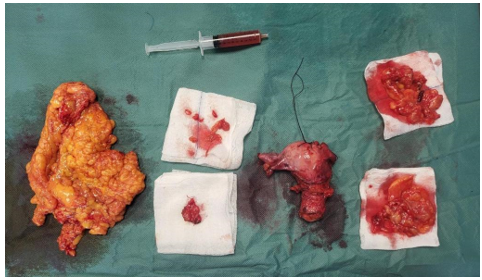
Figure 3. Appearance of surgical parts
Anatomopathological examination of the surgical specimen (Figure 3) revealed:
- Right ovary: poorly to moderately differentiated invasive adenocarcinoma.
- Uterus: clear cell carcinoma infiltrating the isthmus and uterine wall down to the myometrium < 50%.
- Right pelvic resection: 0N+/10N
- Left pelvic resection: 0N+/13N
- Omentectomy: no signs of malignancy, reactive adenitis
- Ascites sampling: absence of malignant cells
- IHC: tumor cells expressed napsin.
Post-operative management was straightforward, and the patient was discharged on the third post-operative day with a discharge order and follow-up appointment.
Discussion
According to various studies, 10% of women with ovarian cancer have SEOC and approximately 5% of women with endometrial cancer are diagnosed with SEOC [4]. The majority of women with SEOC are aged between 41 and 54, 40% are nulliparous, 2/3 are premenopausal and 1/3 are obese [5].
The pathophysiology of SEOC is explained by the theories of oestrogenic environment, microenvironment restriction and hormonal field effect [6,7]. Studies suggest that patients with endometrioid or clear cell ovarian cancer under the age of 53 are at higher risk of loss of MMR expression (MLH1, MSH2 and MSH6) and Lynch syndrome.
The simultaneous detection of a malignant tumor in the endometrium and ovary is often a challenge for clinicians and pathologists in order to achieve a correct diagnosis and appropriate management. The distinction between independent primary tumors and metastatic tumors is clinically significant and also complicated. These tumors can only be distinguished after histopathological examination of the surgical specimen, using the criteria established by Ulbright and Roth, subsequently modified by Scully et al, and immunohistochemical studies [8].
The most common symptom of SEOC is abnormal uterine bleeding, but some patients present to gynecological clinics because of pelvic pain or a palpable pelvic mass, in our case the patient presented with abnormal uterine bleeding and pelvic pain [9].
The histological subtype of both primary tumors is endometrioid in 50-70% of SEOC cases and independent primary tumors are often grade 1 or 2 [10].
The endometrioid type, low grade and early stage of SEOC are associated with a better prognosis and overall survival of 80-90%, in contrast to the poor prognosis seen in metastatic disease (9,10).
SEOCs tend to have the same prognosis as patients with a single Endometrial cancer (EC) or Ovarian cancer (OC), after taking into account age, FIGO stage, histology, year of diagnosis and Eastern Cooperative Oncology Group performance status [11].
Pre-treatment CA-125 concentration and ovarian tumor stage are independent factors in SEOCs [12].
With regard to the pathogenesis of SEOC, the "restricted microenvironment" hypothesis reflects the low metastasis potential of SEOC. It is also thought that embryologically similar tissues, such as those of the female genital tract, are affected by hormonal stimulation and other carcinogenic factors [13].
In addition, mitochondrial DNA analysis and sequencing of various genes have confirmed the clonality of SEOCs [14].
Conclusion
Although SEOC is a rare phenomenon, it is necessary to distinguish this type of malignancy from metastatic disease. Molecular biomarkers are needed to identify the characteristics and underlying pathogenesis of SEOC.
References
- Kelemen LE, Rambau PF, Koziak JM, Steed H, Köbel M. (2017) Synchronous endometrial and ovarian carcinomas: predictors of risk and associations with survival and tumor expression profiles. Cancer Causes Control. 28: 447-457. [PubMed.]
- Scully R, Young R, Clement P. (1998) Tumors of the Ovary, Maldeveloped Gonads, Fallopian Tube and Broad Ligament: Atlas of Tumor Pathology. Bethesda, Armed Forces Institute of Pathology. [Ref.]
- Al Hilli MM, Dowdy SC, Weaver AL, et al. (2012) Incidence and factors associated with synchronous ovarian and endometrial cancer: a population-based case-control study. Gynecol Oncol. 125: 109-113. [PubMed.]
- Soliman PT, Slomovitz BM, Broaddus RR, et al. (2004) Synchronous primary cancers of the endometrium and ovary: a single institution review of 84 cases. Gynecol Oncol. 94: 456-462. [PubMed.]
- Makris GM, Manousopoulou G, Battista MJ, Salloum I, Chrelias G, et al. (2017) Synchronous Endometrial and Ovarian Carcinoma: A Case Series. Case Rep Oncol. 10(2): 732‑736. [Ref.]
- FOGSI Oncology Committee. (2020) Synchronous VS Metastatic Endometrial and Ovarian Cancer - A Diagnostic and Management Dilemma. 1(1). [Ref.]
- Vierkoetter KR, Ayabe AR, VanDrunen M, Ahn HJ, Shimizu DM. (2014) Lynch syndrome in patients with clear cell and endometrioid cancers of the ovary. J Gynaecol Oncol. 135(1): 81-84. [PubMed.]
- Metgud, Mrityunjay, Srivani, Tella, Patil, et al. (2022) A Case Report - Synchronous Endometrial and Ovarian Cancer. Journal of the Scientific Society. 49(2): p 213-216. [Ref.]
- Soliman PT, Slomovitz BM, Broaddus RR, et al. (2004) Synchronous primary cancers of the endometrium and ovary: a single institution review of 84 cases. Gynecol Oncol. 94: 456-462. [PubMed.]
- Zaino R, Whitney C, Brady MF, et al. (2001) Simultaneously detected endometrial and ovarian carcinomas - a prospective clinicopathologic study of 74 cases: a gynecologic oncology group study. Gynecol Oncol. 83(2): 355-362. [PubMed.]
- Heitz F, Amant F, Fotopoulou C, et al. (2014) Synchronous ovarian and endometrial cancer - an international multicenter case-control study. Int J Gynecol Cancer. 24(1): 54-60. [PubMed.]
- Eisner RF, Nieberg RK, Berek JS. (1989) Synchronous primary neoplasms of the female reproductive tract. Gynecol Oncol. 33(3): 335‑339. [PubMed.]
- Schultheis AM, Ng CK, De Filippo MR, et al. (2016) Massively parallel sequencing-based clonality analysis of synchronous endometrioid endometrial and ovarian carcinomas. J Natl Cancer Inst. 108(6): djv427. [PubMed.]
- Guerra F, Girolimetti G, Perrone AM, Procaccini M, Kurelac I, et al. (2014) Mitochondrial DNA genotyping efficiently reveals clonality of synchronous endometrial and ovarian cancers. Mod Pathol. 27(10): 1412-1420. [Ref.]