>Corresponding Author : Elomri Hajar
>Article Type : Case Report
>Volume : 4 | Issue : 10
>Received Date : 19 June, 2024
>Accepted Date : 04 July, 2024
>Published Date : 17 July, 2024
>DOI : https://doi.org/10.54289/JCRMH2400147
>Citation : Younes B, Hajar E, Imane Z, Leila E, Fadwa B, et al. (2024) Bilateral Male Breast Cancer: A Report Case. J Case Rep Med Hist 4(10): doi https://doi.org/10.54289/JCRMH2400147
>Copyright : © 2024 Younes B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access
1Resident Physician, Department of Gynecology and Obstetrics, at Ibn Rochd University Hospital, Casablanca, Morocco
2Professor in the Department of Gynecology and Obstetrics at the Ibn Rochd University Hospital in Casablanca, Morocco
*Corresponding author: Elomri Hajar, Resident Physician, Department of Gynecology and Obstetrics, Ibn Rochd University Hospital, Casablanca, Morocco
Abstract
Breast cancer occurs in men, and its rate of incidence has increased recently. The main particularity of men's breast cancer is that its prognosis is usually worse than that of women, because it is diagnosed late and hence at advanced stage. Bilateral involvement has been reported only in rare cases. We report a case of a bilateral breast cancer, in a 47 year old patient , with no family history of breast cancer , who presented with a bilateral breast mass.
Histopathological biopsy showed a bilateral invasive carcinoma, Luminal B, HER 2 negative . The extension PET scan showed no distant metastases. Bilateral mastectomy and bilateral sentinel lymph node were performed. The final histopathological exam confirmed the previous biopsy diagnostic, the tumors were mutually classified T2N0M0 of the TNM breast cancer classification. The surgical treatment was followed by tamoxifen hormonotherapy and an oncological semestriel follow-up. No recurrences or relapses were reported. The aim of our current work is to draw attention to this pathology in men, in order to contribute to its early diagnosis and therefore to improve its prognosis.
Keywords: Breast cancer, Bilateral, tumor, Male.
Introduction
Breast cancer in men is rare and accounts for about 1 % of all cases of breast cancer, the presentation of bilateral synchronous breast cancer is extremely rare, with an incidence of 2% of all breast cancers in men [1,2]. Its etiopathogenesis remains somewhat obscure, but certain risk factors, including a direct family history and hormonal imbalance, have been incriminated [3]. The male breast cancer prognosis is guarded, because it's a pathology unknown by the general public, and the discovery of a breast nodule in a man doesn't arouse the same concern as in a woman, which leads to a delayed approach to treatment [4]. We report a case of a 47 years old patient with a of a bilateral breast cancer, bilateral mastectomy and bilateral sentinel lymph node were performed, the tumors were mutually classified T2N0M0 of the TNM breast cancer classification. The surgical treatment was followed by tamoxifen hormonotherapy and an oncological semestriel follow-up. No recurrences or relapses were reported.
Case Report
Mr M.A, 47 years old patient, was referred by a general doctor to the gynecological oncology department of the Casablanca University hospital center, for the management of an autopalpation of two bilateral breast masses that have been progressively evolving over the past year. No familial breast cancer history neoplasia has been reported. The clinical examination revealed a patient in good general condition, with the following findings on breast examination (Figure 1) : on the right breast, a mass straddling the internal quadrants measuring 3 x 2 cm and mobile in relation to the two planes, with no signs of inflammation or nipple discharge; on the left breast a mass straddling the internal quadrants measuring 4 x 3 cm and mobile in relation to the two planes was found, with no signs of inflammation or nipple discharge. The general lymph node examination revealed no palpable adenopathy.

Figure 1. clinical examination of the patient
Given the difficulty of performing a mammogram, the radiological examination consisted exclusively of an ultrasound scan of the breasts and the lymph nodes areas.
Mammary ultrasound revealed: on the right breast, nine homogeneous, partially necrotic, locally confluent breast lesions on the right breast, predominantly in the inner quadrants, the largest of which measured 10 x 6.5 mm above the internal nipple (Figure 2), on the left breast thickened and irregular galactophoric duct in the upper inner quadrant, continuing into a hypoechoic, heterogeneous mass with spiculated contours, measuring 32 x 13mm (Figure 3), no axillary adenopathy was detected. The radiological examination was classified Birads 5 for both breasts.
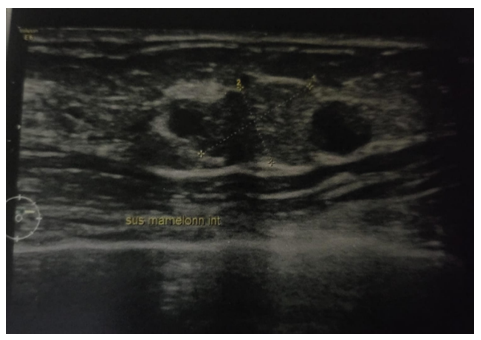
Figure 2. The largest lesion in the inner quadrants on the right breast, measuring 10 x 6.5 mm above the internal nipple.
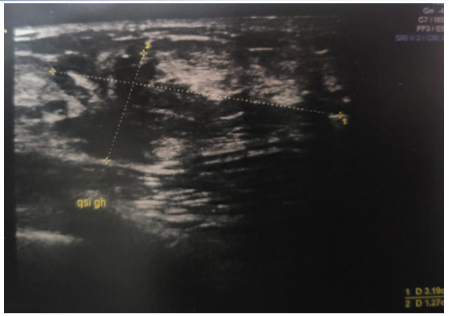
Figure 3. A hypoechoic, heterogeneous mass with spiculated contours, in the upper inner quadrant on the left breast measuring 32 x 13mm.
A tru-cut biopsy was performed, revealing in both breasts an infiltrating breast carcinoma proliferation, NOS type, SBR 2, with immunohistochemical Luminal B profile, HER 2 negative.
A pet scan showed no distant metastases. The patient file has been discussed in a multidisciplinary consultation meeting and the final decision was to perform a bilateral mastectomy with a bilateral sentinel lymph node exam.
Bilateral mastectomy and bilateral sentinel lymph node (0 N + / 3 N) were performed. The final histopathological exam confirmed the previous biopsy diagnostic, the tumors were mutually classified T2N0M0 of the TNM breast cancer classification, with an immunohistochemical Luminal B profile, HER 2 negative.
The surgical treatment was followed by tamoxifen hormonotherapy and an oncological semestriel follow-up showed no recurrences or relapses.
Discussion
Breast cancer is the most prevalent malignant disease among women worldwide. According to data published in 2019, breast cancer accounted for 30% of newly diagnosed malignant tumors in women, and led to 15% of female cancer deaths [5]. Male breast cancer represents about 1% of all cancers that develop in men and about 1% of all breast cancers worldwide [1]. The average age of discovery of a male breast cancer is around sixty-six years old, and 10% of patients are under fifty [1]. Although it is a rare masculin cancer, the incidence of this male pathology has been rising steadily over the past three decades, from 0.86/100,000 to 1.06/100,000 [6]. Bilateral breast cancer is extremely rare, with an incidence of 1.5%-2% of all male breast cancers [2].
The risk factors for breast cancer in men are basically the age, family neoplasic history, diseases associated with hyperoestrogenism , Klinefelter's syndrome, radiation exposure, estrogen treatment, black race and obesity but The most critical risk factor is a positive family history of breast cancer therefore the risk is multiplied by two if the history is positive for first-degree relatives, and by five if there are other affected first-degree relatives [7]. The familial factor is linked to mutations in several genes such as BRCA1 and BRCA2, the TP-53 (Li-Fraumani) gene, the MLH1, MLH2, PMS2 (Lynch syndrome) and PALB2 genes [7].
The presence of a man with breast cancer in a family is therefore a risk factor for mutation and is in itself a possible indication for oncogenetic consultation , the Current National Comprehensive Network recommends breast surveillance of men carrying a mutation of these genes, with training in self-palpation, bi-annual clinical surveillance, and considers an initial mammogram, followed by annual mammographic surveillance in case of presence of gynecomastia or breast density on this first mammogram [8].
Clinical symptoms generally appear later in men than in women, the diagnosis is often made at advanced stages, men have more localized tumors, but more lymph node involvement and risk of metastases at the time of diagnosis [8]. The most common symptom in male breast cancer is pain that occurs over a mass that appears gradually [9].
The radiological image of a male breast cancer is not specific it can appear as an irregular opacity with spiculated margins and is frequently associated with gynecomastia [10]. Calcifications are not frequent in male breast cancer, yet any calcifications besides, should be considered suspicious irrespective of their morphology or distribution, on mammogram of male breasts [11]. Breast MRI is being used in females for breast cancer staging and treatment planning. Similarly, MRI can be used in males in certain cases of breast cancers, to evaluate for disease extent and for detection of contralateral cancers [11].
The most common histological type of male breast cancer is the infiltrating carcinoma in 90% of the cases, carcinoma in situ corresponds to 10% of lesions, of which 75% are of the papillary type and the lobular carcinomas are exceptional due to the absence of the terminal lobules in the normal male breast, but it can occur in 1% of patients with Klinefleter syndrome (XXY) [1]. More than 90% of tumors have positive hormone receptors [2].
The treatment is multidisciplinary using surgery, radiotherapy and chemotherapy as well as innovative therapies improving the overall survival of patients [12].
The prognosis between men and women are similar when comparing patients with the same tumor characteristics (hormonal receptors, axillary involvement, tumor size and histology). Male survival is lower than female survival when comparing early-stage disease without lymph node involvement, suggesting that there are sex differences in the pathogenesis and biology of neoplasia [1].
References
- Male breast cancer incidence and mortality, United States- 2013-2017. U.S. Cancer Statistics Data Brief, No. 19. 2020. [Ref.]
- Rubio Hernandez MC, Diaz Prado YI, Perez SR, Diaz RR, Aleaga ZG. Synchronous bilateral breast cancer in a male. Ecancermedicalscience. 2013;7:377. [PubMed.]
- Burga AM, Fadare O, Lininger RA, Tavassoli FA. Invasive carcinomas of the male breast: a morphologic study of the distribution of histologic subtypes and metastatic patterns in 778 cases. Virchows Arch. 2006;449(5):507-12. [PubMed.]
- Darkeh MHSE, Azavedo E. Male breast cancer clinical features, risk factors, and current diagnostic and therapeutic approaches. Int J Clin Med. 2014;5:1068-86. [Ref.]
- Wang X, Wang C, Guan J, Chen B, Xu L, Chen C. Progress of Breast Cancer basic research in China. Int J Biol Sci. 2021 May 11;17(8):2069-79. [Ref.]
- Cutuli B, Le-Nir CC, Serin D, Kirova Y, Gaci Z, Lemanski C, et al. Male breast cancer. Evolution of treatment and prognostic factors. Analysis of 489 cases. Crit Rev Oncol Hematol. 2010;73(3):246-54. [PubMed.]
- Sanguinetti A, Polistena A, et al. Cancer du sein chez l’homme, présentation clinique, diagnostic et traitement. Int J Surg. 2016;8-11. [PubMed.]
- Eisinger F, Bressac B, Castaigne D, Cottu PH, Lansac J, Lefranc JP, et al. Identification et prise en charge des prédispositions héréditaires aux cancers du sein et de l'ovaire. Bull Cancer. 2004;91(3):219-37. [PubMed.]
- Korde LA, Zujewski JA, Kamin L, Giordano S, Domchek S, Anderson WF, et al. Multidisciplinary meeting on male breast cancer: summary and research recommendations. J Clin Oncol. 2010;28(12):2114-22. [PubMed.]
- Mathew J, Perkins GH, Stephens T, Middleton LP, Yang WT. Primary breast cancer in men: clinical, imaging, and pathologic findings in 57 patients. AJR Am J Roentgenol. 2008;191(6):1631-9. [PubMed.]
- Dershaw DD, Borgen PI, Deutch BM, Liberman L. Mammographic findings in men with breast cancer. AJR Am J Roentgenol. 1993;160(2):267-70. [PubMed.]
- Fitousi A, Couturaud B, Delay E, Lantieri L. Chirurgie du cancer du sein: traitement conservateur. Oncoplastie et reconstruction. 2011. p. 280. Elsevier Masson. [Ref.]