>Corresponding Author : Jadon Ashok
>Article Type : Original Research Article
>Volume : 2 | Issue : 2
>Received Date : 05 May, 2022
>Accepted Date : 15 May, 2022
>Published Date : 18 May, 2022
>DOI : https://doi.org/10.54289/JAAD2200108
>Citation : Ashok J, Prashant KS, Swastika C, Neelam S, Apoorva B, et al. (2022) Functional Outcome and Pain Relief After Pulsed Radiofrequency of Saphenous Nerve in Medial Compartment Knee Osteoarthritis: A Randomised Double-Blind Trial. J Anesth Anesth Drug 2(2): doi https://doi.org/10.54289/JAAD2200108
>Copyright : © 2022 Ashok J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Original Research Article | Open Access
1D-63, Vijaya Heritage Ph-6, Kadma, Jamshedpur, India - 831005
2Department of Anaesthesia & Pain Relief Service, Tata Motors Hospital, Telco Colony, Jamshedpur, Jharkhand, India - 831004
*Corresponding author: Jadon Ashok, D-63, Vijaya Heritage Ph-6, Kadma, Jamshedpur, India-831005
Abstract
Background and aims: Pulsed radiofrequency (PRF) of saphenous nerve (SN) has shown effective pain relief in knee pain due to knee osteoarthritis (KOA). Since adductor canal (AC) contains other sensory nerves innervating the medial part of knee joint apart from SN. We compared the PRF of SN within and outside the AC for their quality and duration of pain relief in knee osteoarthritis of medial compartment (KOA-MC).
Methods: We conducted a randomised prospective study in 60 patients with anteromedial knee pain due to KOA-MC. Patients in group A received PRF-SN and those in group B, PRF-AC. Primary objectives were, comparison of pain by visual analogue scale (VAS) score and changes in quality of daily living by Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) and OXFORD knee scores (OKS). Secondary objectives were, comparison of analgesic requirements using Medicine Quantification Scale (MQS) scale and block related complications. Intra group comparison was done by Analysis of variance (ANOVA). Inter group normally distributed data was assessed by student's t-test, non-normally distributed and ordinal data by Mann-Whitney U-test and categorical data by Chi-square test. A p value of < 0.05 was considered significant.
Results: VAS scores were significantly lower in Gr-B at 12 weeks. The WOMAC scores and OXFORD scores at 4, 8, 12 and 24 weeks were significantly lower in Gr-B compared to Gr-A.
Conclusion: The PRF-AC provides better pain relief and functional outcome than PRF-SN however, duration of pain relief was not significantly different.
Keywords: Adductor Canal; Knee Joint; Osteoarthritis Knee; Pulsed Radiofrequency Treatment; Pain Management; Saphenous Nerve
Abbreviations: PRF: Pulsed Radiofrequency, SN: Saphenous Nerve, KOA: Knee Osteoarthritis, AC: Adductor Canal, KOA-MC: Knee Osteoarthritis of Medial Compartment, VAS: Visual Analogue Scale, WOMAC: Western Ontario and Mcmaster Universities Osteoarthritis Index, OKS: OXFORD Knee Scores, MQS: Medicine Quantification Scale, ANOVA: Analysis of Variance, NVM: Nerve to Vastus Medialis, IQR: Interquartile Range
Introduction
Knee osteoarthritis (KOA) is a common degenerative disease in the older population, causing pain, stiffness and dysfunction. The involvement of medial compartment (KOA-MC) of the joint is 5–10 times higher than disease in the lateral compartment [1,2]. The saphenous nerve supplies the anterior and medial part of the joint and the interventional management of saphenous nerve and pulsed radiofrequency (PRF) of saphenous nerve (SN) have shown long lasting relief [3-5]. As PRF of SN provides effective pain relief in KOA, we hypothesized that PRF of adductor canal (AC) which contains SN and other sensory nerves (like nerve to vastus medialis (NVM), medial femoral cutaneous nerve of thigh, intermediate femoral cutaneous nerve of thigh, branches of obturator nerve and related to knee joint innervation on the anterior and medial side), may provide superior pain relief in KOAMC. As there was no comparative study available, we conducted this comparative study in patients of KOA-MC with knee pain to assess the quality and duration of pain relief after PRF of SN and PRF of AC.
Methods
After clearance from the ethical committee and registration with CTRI this prospective randomised double-blinded study was conducted at a teaching hospital during May 2019 to February 2021 (including 6 months of follow-up). A total 60 patients of both sexes aged 40-80 years having predominantly medial knee pain due to KOA-MC were included in the study. Inclusion criteria were pain and tenderness for more than 6 months on anteromedial aspect of the knee owing to KOA and matching x-ray findings of grade 2-4 radiographic changes according to the Kellgren–Lawrence classification [6]. Exclusion criteria were refusal to participate in the study, presence of other knee pathology such as fracture or rheumatic diseases, previous surgery of the knee or knee synovitis.
Patients having any contraindication to nerve blocks or radiofrequency treatment were also excluded.
After written informed consent, all the patients (n= 58) were randomly divided into two equal groups- PRF-SN (Gr-A, n= 29) and PRF-AC (Gr-B, n= 29) (Figure-1) by computer generated random numbers and group assignment was done by sequentially numbered opaque envelopes. All the blocks were performed by a single experienced anaesthesiologist who was not involved in post procedure observations. Patients were taken to the operating room and standard monitors (electrocardiogram, non-invasive blood pressure and pulse oxymeter) were attached. The blocks were performed in supine position with standard protocol and strict sterile technique.
To perform PRF-AC a high frequency US probe (6-13 MHz SonoSite-M Turbo®, Fuji India.) was placed in transverse orientation at mid-thigh level. Sonoanatomy of adductor canal was identified (Fig. 2 A). The needle entry point at skin was anaesthetized with 2 ml 1% lidocaine and a 20-gauge 10 cm long blunt-tip RF cannula with 10 mm active tip (COSMAN Cannula-RFK™) was inserted towards the nerve complex lateral to femoral artery using an in-plane view (Fig.2 B & C). Sensory stimulation at 50 Hz (0.5 mV) and motor stimulation at 2 Hz (1 mV) was done to observe the sensation along the course of saphenous nerve including on the inferior-medial side of the knee joint and contraction of vastus medialis muscle respectively. Once the needle position was confirmed, PRF was done for 8 minutes (4 cycles of 120 seconds each at 42°C and 50V). After completion of PRF, 5 ml mixture of 0.25% bupivacaine and 40 mg methyl-prednisolone acetate (Depot. preparation) was given.
To perform PRF-SN, after identifying the sonoanatomy of adductor canal (Fig. 2 A), the US probe was moved distally to follow the course of the SN. When the SN was medial and a little away from the artery, the block needle was inserted towards the SN using an in-plane view (Fig.2 D &E). Sensory stimulation at 50 Hz (0.5 mV) and motor stimulation at 2 Hz (1-2 mV) was done. We observed the tingling sensation along the course of saphenous nerve including inferior-medial side of knee joint however, there was no motor response. Once the needle position was confirmed, PRF was done for 8 minutes (4 cycles 2 minutes each at 42°C, 50V). After completion of PRF, 5 ml mixture of 0.25% bupivacaine and 40 mg methylprednisolone acetate (Depot. preparation) was injected via the cannula. Patients were discharged after observation for 1 hour. Patients were allowed to take medicines (topical analgesics, non-steroidal anti-inflammatory drugs, gabapentinoids, tricyclic antidepressants and tramadol) as before the intervention. If required, patients were advised to take tablet paracetamol 500 mg as desired up to a maximum of 3 tablets/24 hours for 2-3 days to manage procedural pain. After 48 hours, all the patients were called and a structured physiotherapy session for 10 days at the physiotherapy outpatient department was done with the help of a professional physiotherapist followed by guided home based exercises. Follow-up was done at 4, 8, 12 and 24 weeks. Primary objectives were to compare pain and changes in quality of daily living in Gr-A and Gr-B. VAS score (0-100) was used to assess the pain relief and WOMAC (Western Ontario and McMaster Universities
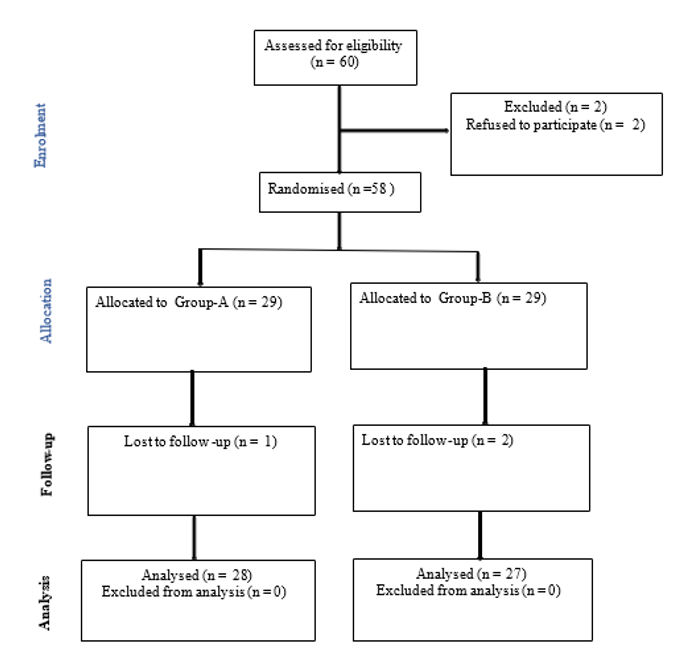
Figure 1: CONSORT flow diagram for enrolment, group allocation, follow-up and analysis
Gr-A; PRF-SN- (Pulsed radiofrequency of saphenous nerve), Gr-B; PRF-AC (Pulsed radiofrequency of adductor canal)
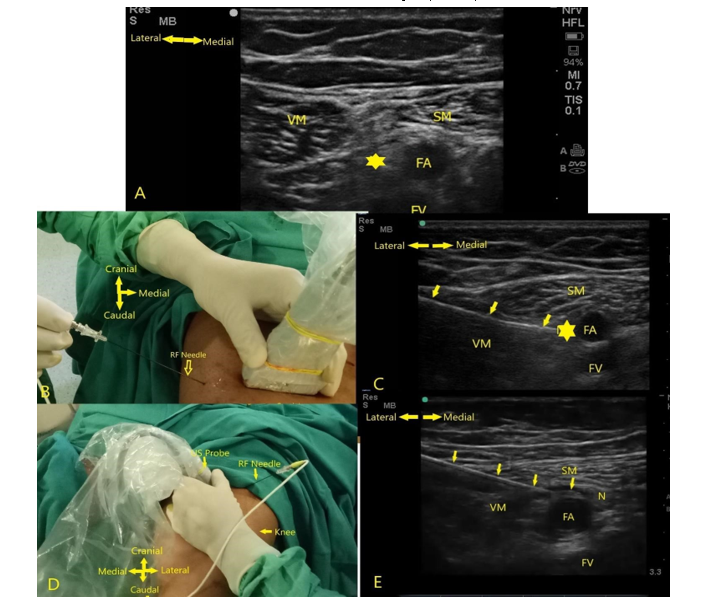
Figure 2: A-sonoanatomy of adductor canal, B-Needle entry from lateral to medial side under high frequency US probe, C-needle positioned on the nerve complex lateral to femoral artery, D- needle entry from lateral to medial direction at the distal part of thigh towards SN using in-plane view E-radiofrequency needle in contact with SN. FA-femoral artery, FV-femoral vein, VM-vastus medialis, SM-sartorius muscle, * nerve complex (SN+VM)
Osteoarthritis Index) and OXFORD knee scores (OKS) were used to assess the functional outcome (quality and activity of daily living). The WOMAC used in this study was the Likert version 3.1 consisting of 24 self-administrated questions that were answered for each item on a 5-point Likert scale (none-0, mild-1, moderate-2, severe-3 and extreme-4). It was reported as three separate subscales: pain, physical function and stiffness. The WOMAC pain subscale had five questions with scores 0 to 4 and was considered invalid if more than one item was missing; hence, it had a range of 0 (no pain) to 20 (maximal pain) and the total score range was between 0-96. In the event of a missing item, the remaining four items were averaged and then multiplied by five [7]. In OKS, original scoring system was used where the symptoms score ranges from 1-5; where score 1 represented the best outcome (lesser score is better) [8]. In OKS reporting, if there were one or two missing answers, a mean answer from the patient's other answer was entered. If a question had more than one answer, the smallest number was used for calculations [8]. The secondary objectives were to compare the analgesic requirements using Medicine Quantification Scale (MQS) and block related complications. Assessments of WOMAC, VAS and MQS were done by a resident of anaesthesia/ pain management who was unaware about the group allocation. The OKS assessment was done by an observer of orthopaedic department who was also unaware about the protocol and the group allocation. The data was entered in an excel sheet. The results were analysed using the statistical software (MedCalc version 20.0). Within each group, comparison of various scores (pre-intervention or base line values up to 24 weeks) was done using one-way ANOVA. To compare Gr-A & Gr-B, the continuous data was assessed for normality using the Kolmogorov-Smirnov test of normality. Normally distributed data (represented as Mean ± SD) was assessed using the student’s t-test (two-tailed, unequal variances). Non-normally distributed data and ordinal data [represented as median and interquartile range (IQR)] was assessed using the Mann-Whitney U-test. Chi-square statistic was used for categorical data. A p-value < 0.05 was considered significant.
Sample size was based on our pilot study of 20 patients where VAS at 6 months was 42 ± 10.49.
Considering 20% change as significant and using the formula (N= 2σ2 (z1−β +z 1−α /2)2 ÷ (μ0−μ1)2 , N= 2(10.492 +10.492) (0.84+1.96)2 ÷ (8)2 , N=54), 27 patients in each group were required with 95% confidence, 80% power and p < 0.05 where, μ0 = population mean, μ1 = mean of study population, N = sample size of study population, σ = variance of study population, α = probability of type I error (0.05), β = probability of type II error (0.2), z = critical Z value for a given α or β. We enrolled 60 patients to take care of attrition.
Results:
A total of 60 patients were enrolled and 58 randomised and 55 were finally analysed (2 patients were excluded before randomisation and 3 patients opted out before final follow up at 24 weeks) (Figure-1). The demographic profile of patients including mean age, weight, BMI, male/ female ratio, radiological severity of KOA and number of cases with bilateral affection were comparable in both the groups (Table-1). The WOMAC scores at 4, 8, 12 and 24 weeks were significantly lower in Gr-B compared to Gr-A; p= 0.004, 0.008, 0.034 and 0.013 respectively. The OXFORD scores were significantly lower in Gr-B at 4, 8, 12 and 24 weeks p < 0.0001, < 0.0001, < 0.0001 and p= 0.02 respectively. VAS scores were comparable in Gr-A and Gr-B at 4, 8 and 24 weeks p= 0.827, 0.852, and 0.754 respectively. However, significantly lower in Gr-B at 12 weeks p= 0.010 (Table-2). In both the groups, there was significant reduction in pain and improvement in the functional outcome when compared within the group (One-way ANOVA) at all the follow-up periods (p< 0.0001). In both the groups, there was significant reduction in WOMAC, OKS at 24 weeks compared to pre-intervention levels p< 0.0001 (Figure-3). The MQS scores were comparable in Gr-A and Gr-B at 24 weeks p= 0.123 (Table-3). No patient in any group had any complication related to PRF intervention.
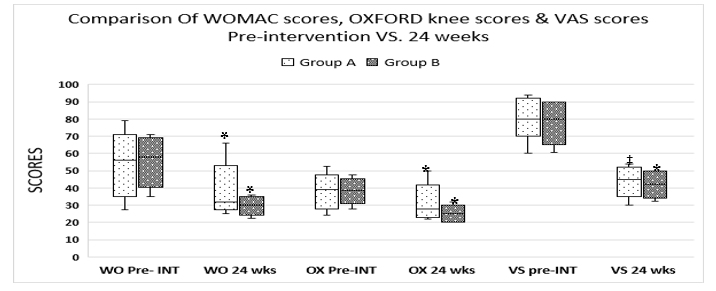
Figure 3:Comparison of various scores at pre-intervention (Baseline level) and at 24 weeks
Gr-A; Pulsed radiofrequency of saphenous nerve, Gr-B; Pulsed radiofrequency of adductor canal,
WO- (WOMAC; Western Ontario and McMaster Universities Osteoarthritis Index), OX- (OXFORD knee scores), VS-(VAS; visual analogue scale), pre-int; pre-intervention, SD; standard deviation, p <
0.0001 (*Paired Student t-test, ‡Mann Whitney U-test)
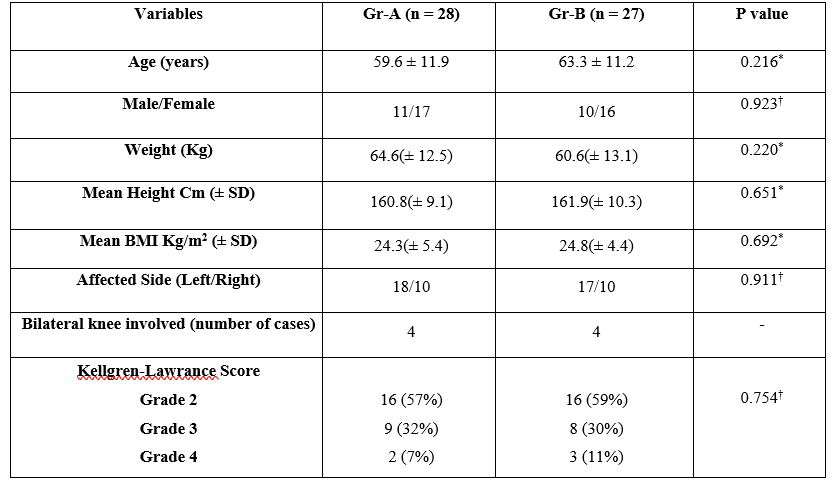
Table-1:Demographic variables, Kellgren-Lawrence Score (KJ grades of arthritis) and side of Knee involved in patients of Gr-A and Gr-B
†Chi-square test, *Student t-test, SD-standard deviation, BMI-Body mass index, Gr-A; Pulsed radiofrequency of Saphenous nerve, Gr-B; Pulsed radiofrequency of Adductor canal.
Discussion
We conducted a double blinded randomised study to compare the efficacy of PRF-SN with PRF-AC to treat pain in KOA-MC. There was significant pain relief and improvement in the functional scores from pre-intervention values at all the follow-up periods (4-24 weeks) in both the groups. This reduction in functional improvement was significantly better in Gr-B (PRF-AC) compared to Gr-A (PRF-SN).
Saphenous nerve is a terminal sensory branch of femoral nerve and supplies anterior and medial part of joint capsule. It plays an important role in the pain management of the knee joint. Akbas et al. [4] investigated 115 patients with chronic knee pain after 8 minutes of PRF-SN. All patients showed remarkable improvement in their VAS and WOMAC scores (p = 0.001). Vas et al. [9] used PRF of multiple nerves to manage pain of KOA and PRF-SN was one of the components of the management strategy. Recently, Baysal et al. [5] has concluded that PRF-SN is a safe and function sparing technique for knee osteoarthritis. However, there was a lacuna in the literature as, only few studies are available where PRF-SN has been used to treat the chronic pain in KOA and comparative studies with PRF-AC were lacking.
SN is consistently present in adductor canal and to achieve motor sparing in SN block, it is advised to block it in the distal part of AC where it is away from the branches of the nerve to vastus medialis (NVM). Therefore, we performed PRF-SN at the distal part of AC after confirming the absence of motor stimulation to achieve selective sensory block of SN.
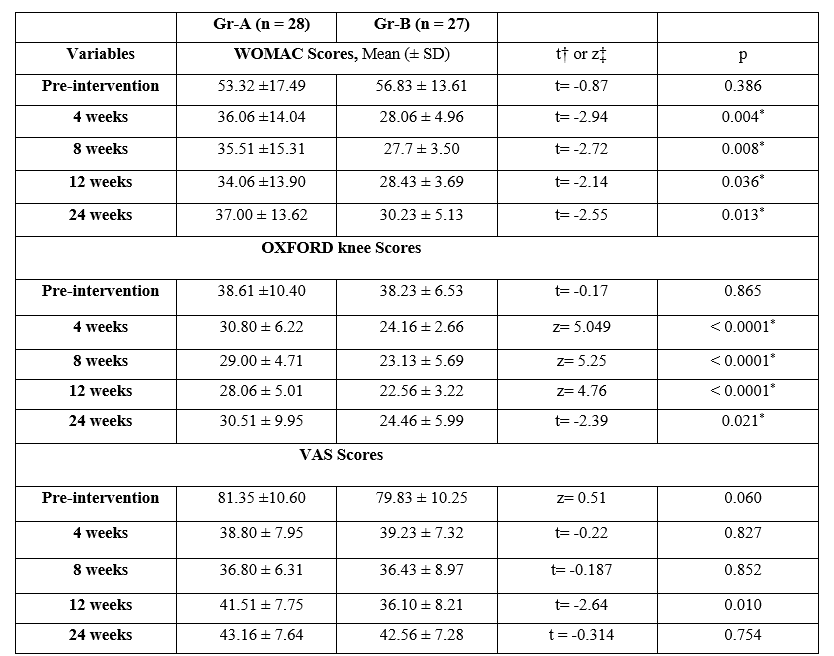
Table-2:Comparison of WOMAC, OXFORD and VAS scores at various follow-up periods in Gr-A and Gr-B.
Gr-A; Pulsed radiofrequency of saphenous nerve, Gr-B; Pulsed radiofrequency of adductor canal, WOMAC; Western Ontario and McMaster Universities Osteoarthritis Index, VAS; visual analogue scale, SD; standard deviation, * p < .05 (significant), †Student t-test, ‡Mann Whitney U-test
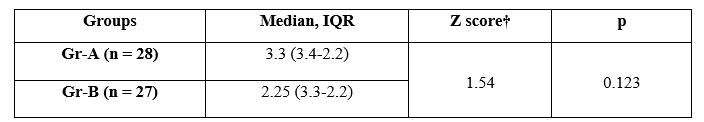
Table-3:Comparative MQS scores at 24 weeks in Gr-A and Gr-B.
† Mann-Whitney U test, MQS; Medicine Quantification Scale. Gr-A; Pulsed radiofrequency of saphenous nerve, Gr-B; Pulsed radiofrequency of adductor canal.
Over the years the adductor canal (AC) block has been effectively used for pain relief after total knee arthroplasty (TKA) [10], for knee joint rehabilitation [11] and also to manage chronic knee pain [12,13]. The main reason of its efficacy is that it blocks multiple nerves including SN, NVM, branches of obturator and other branches of femoral nerves which are involved in pain transmission either directly or contributing in the formation of nerve plexus around the knee (sub-sartorial plexus, peripatellar plexus) [14, 15, 16].
When the neurovascular structures pass through the adductor canal, the nerves change their course (direction) and relation. Therefore, contents of AC depend upon which part of the canal is being observed (proximal, middle or distal) [17, 18]. It has been stated that the NVM lies outside in the distal part of the AC in about 90% of the cases [19, 20]. However, other studies do not support this view and have observed that NVM has many branches entering the AC and the mid-portion of the adductor canal is an optimal site to block both the target nerves (SN and NVM) [14]. In our study, we selected proximal AC where motor stimulation confirmed the presence of the NVM in close proximity with SN. PRF in this area would have included the SN, NVM and other sensory nerves contributing to knee pain therefore resulted in better analgesia in Gr-B compared to Gr-A.
Genicular nerves are terminal sensory nerves supplying the knee joint and the RFA and PRF of genicular nerves are established techniques to manage KOA pain [21]. Previous studies have shown that the deep genicular branches originate from a deep plexus with mixed contribution from both the SN and the NVM [14, 22]. Therefore, from the observations of the present study, it can be extrapolated that, the PRF of SN and AC might have neuromodulated the sensory inputs at the source of origin of these genicular nerves (SN and NVM).
To assess the functional outcome of any analgesic intervention in KOA, WOMAC score is commonly used. It assesses three components, namely, pain, stiffness and function. However, WOMAC reporting is inadequate in 53% of the studies [22]. Therefore, we have also incorporated the VAS (0-100) (measured by independent observers) and OKS which has good evidence for its internal consistency and construct validity [8]. Intake of analgesics by patients may work as a confounding factor therefore, we incorporated the MQS (version III). The MQS (version III) is a method of quantifying different pain drugs regimens by evaluating the use of 22 distinct drugs. The score is calculated on the basis of the type of medicine and the amount taken in reference to therapeutic range (1= Sub-therapeutic dose or occasional use (PRN), 2= Lower 50% of the therapeutic dose range, 3=Upper 50% of the therapeutic dose range, 4= Supra-therapeutic dose range) [23]. In our study, as the pain relief was significantly better in Gr-B at 12 weeks, it was expected to have lesser use of medications. However, MQS scores were comparable in Gr-A and Gr-B at 24 weeks and reasons could be other than the pain itself [24].
The radiofrequency ablation (RFA) of genicular nerves is although, an effective technique to manage pain in KOA but, safety of RFA has been questioned [25]. Initially, Choi et al., has suggested 3 targets for RFA [26]. However, it became more difficult and time consuming procedure as new research with revised anatomical targets has suggested five targets to provide effective pain relief [27]. Contrary to that, we used single target procedures for PRF-SN and PRF-AC and found a high acceptance among patients and lesser procedural time. Although, PRF of SN has been used to treat pain of KOA [4] and research is underway to evaluate the effectiveness of pulsed radiofrequency in adductor canal for the treatment of knee pain [28, 29]. The present study is a novel study because, no such comparison has been published earlier to our knowledge. However, there were few limitations in the present study. First of all, we have included only those patients suffering with antero-medial knee pain and therefore, the effect of such treatment cannot be extrapolated for lateral knee pain. Second, we did not analyse the grades of severity with outcome. Lastly, the use of steroids with local anaesthetic after the pulsed RF could have been confounder to influence the pain relief.
Conclusion
PRF of SN and AC effectively reduced pain of KOA-MC and improved the functional outcome. The PRF-AC provided better functional outcome than PRF-SN however, duration of pain relief was not significantly different.
References:
- Ahlback S. (1968) Osteoarthrosis of the knee. A radiographic investigation. Acta Radiol Diagn 277: 7-72. [PubMed.]
- Felson DT, Nevitt MC, Zhang Y, Aliabadi P, Baumer B, et al. (2002) High prevalence of lateral knee osteoarthritis in Beijing Chinese compared with Framingham Caucasian subjects. Arthritis Rheum. 46: 1217-1222. [Ref.]
- Arcila LMA, Rivera DR, Mejía AMA, Jaramillo JS. (2014) Efficacy and safety of ultrasound-guided saphenous nerve block in patients with chronic knees pain. Colomb J Anesthesiol. 42: 166-171. [Ref.]
- Akbas M, Luleci N, Dere K, Luleci E, Ozdemir U, Toman H. (2011) Efficacy of pulsed radiofrequency treatment on the saphenous nerve in patients with chronic knee pain. J Back Musculoskelet Rehabil. 24: 77-82. [PubMed.]
- Baysal PK, Baysal O, Erkılınc A, Gurcu ME, Yeksan AN, et al. (2018) Is saphenous nerve radio frequency an effective treatment for advanced gonarthrosis in elders with cardiac comorbidity? J Back Musculoskelet Rehabil 31: 113-118. [PubMed.]
- Emrani PS, Katz JN, Kessler CL, Reichmann WM, Wright EA, McAlindon TE, et al. (2008) Joint space narrowing and Kellgren-Lawrence progression in knee osteoarthritis: an analytic literature synthesis. Osteoarthritis Cartilage. 16: 873-882. [PubMed.]
- Burch FX, Tarro JN, Greenberg JJ, Carroll WJ. (2008) Evaluating the benefits of patterned stimulation in the treatment of osteoarthritis of the knee: a multi-center, randomised, single-blind, controlled study with an independent masked evaluator. Osteoarthritis Cartilage. 16: 86572. [PubMed.]
- Harris K, Dawson J, Jones LD, Beard DJ, Price AJ. (2013) Extending the use of PROMs in the NHS- using the Oxford Knee Score in patients undergoing non-operative management for knee osteoarthritis: a validation study. BMJ Open 3: e003365. [Ref.]
- Vas L, Pai R, Khandagale N, Pattnaik M. (2014) Pulsed radiofrequency of the composite nerve supply to the knee joint as a new technique for relieving osteoarthritic pain: a preliminary report. Pain Physician 17: 493-506. [PubMed.]
- Grevstad U, Mathiesen O, Lind T, Dahl JB. (2014) Effect of adductor canal block on pain in patients with severe pain after total knee arthroplasty: a randomised study with individual patient analysis. Br J Anaesth. 112: 912-919. [PubMed.]
- Rhatomy S, Rahmadian R, Alam Rasyid F, Margaretha E. (2021) Adductor Canal Block in the Outpatient Clinic for Pain Control Following Knee Surgery. Anesth Pain Med. 11: e110904. [PubMed.]
- Taheri A, Hatami M, Dashti M, Khajehnasiri A, Ghajarzadeh M. (2015) Effect of Ultrasound-Guided Subsartorial Approach for Saphenous Nerve Block in Cases with Saphenous Nerve Entrapment in Adductor Canal for Controlling Chronic Knee Pain. Middle East J Anaesthesiol 23: 25-28. [PubMed.]
- Lee DH, Lee MY, Kwack KS, Yoon SH. (2017) Effect of adductor canal block on medial compartment knee pain in patients with knee osteoarthritis: Retrospective comparative study. Medicine (Baltimore). 96: e6374. [PubMed.]
- Laurant DB, Peng P, Giron Arango L, Niazi AU, Chan VW, et al. (2016) The Nerves of the Adductor Canal and the Innervation of the Knee: An Anatomic Study. Reg Anesth Pain Med. 41: 321-327. [PubMed.]
- Franco CD, Buvanendran A, Petersohn JD, Menzies RD, Menzies LP. (2015) Innervation of the Anterior Capsule of the Human Knee: Implications for Radiofrequency Ablation. Reg Anesth Pain Med. 40: 363-368. [PubMed.]
- Jadon A. (2018) Pulsed radiofrequency lesioning of saphenous nerve and adductor canal in lower limb pain due to metastatic nodule. Indian J Anaesth. 62: 392-393. [Ref.]
- Bendtsen TF, Moriggl B, Chan V, Borglum J. (2015) Basic Topography of the Saphenous Nerve in the Femoral Triangle and the Adductor Canal. Reg Anesth Pain Med. 40: 391-392. [PubMed.]
- Cowlishaw P, Kotze P. (2015) Adductor canal block or subsartorial canal block? Reg Anesth Pain Med 40: 175-176. [PubMed.]
- Kapoor R, Adhikary SD, Siefring C, McQuillan PM. (2012) The saphenous nerve and its relationship to the nerve to the vastus medialis in and around the adductor canal: an anatomical study. Acta Anaesthesiol Scand 56: 365-367. [PubMed.]
- Saranteas T, Anagnostis G, Paraskeuopoulos T, Koulalis D, Kokkalis Z, et al. (2011) Anatomy and clinical implications of the ultrasound-guided subsartorial saphenous nerve block. Reg Anesth Pain Med. 36: 399-402. [PubMed.]
- Ikeuchi M, Ushida T, Izumi M, Tani T. (2011) Percutaneous radiofrequency treatment for refractory anteromedial pain of osteoarthritic knees. Pain Med. 12: 546-551. [PubMed.]
- Kennedy JC, Alexander IJ, Hayes KC. (1982) Nerve supply of the human knee and its functional importance. Am J Sports Med. 10: 329-335. [PubMed.]
- Harden RN, Weinland SR, Remble TA, Houle TT, Colio S, et al. (2005) Medication Quantification Scale Version III: update in medication classes and revised detriment weights by survey of American Pain Society Physicians. J Pain. 6: 364-371. [PubMed.]
- Castelnuovo G, Giusti EM, Manzoni GM, Saviola D, Gabrielli S, et al. (2018) What Is the Role of the Placebo Effect for Pain Relief in Neurorehabilitation? Clinical Implications from the Italian Consensus Conference on Pain in Neurorehabilitation. Front Neurol. 9: 310. [PubMed.]
- Kim SY, Le PU, Kosharskyy B, Kaye AD, Shaparin N, et al. (2016) Is Genicular Nerve Radiofrequency Ablation Safe? A Literature Review and Anatomical Study. Pain Physician. 19: E697-705. [PubMed.]
- Choi WJ, Hwang SJ, Song JG, Leem JG, Kang YU, et al. (2011) Radiofrequency treatment relieves chronic knee osteoarthritis pain: a double-blind randomised controlled trial. Pain. 152: 481-487. [PubMed.]
- Fonkoue L, Stoenoiu MS, Behets CW, Steyaert A, Kouassi JK, et al. (2021) Validation of a new protocol for ultrasound-guided genicular nerve radiofrequency ablation with accurate anatomical targets: cadaveric study. Reg Anesth Pain Med. 46(3): 210-216. [PubMed.]
- ClinicalTrials.gov. (2016) [Internet] National Library of Medicine (US). 2015-09-01-. Identifier: NCT02680392 Functional Outcome and Analgesia in TKA: Radiofrequency vs Continuous Adductor Canal Block) [Ref.]
- ClinicalTrials.gov. (2021) [Internet] National Library of Medicine (US). July 1, 2020-. Identifier: NCT04454710, Pulsed Radiofrequency and Osteoarthritic Chronic Knee Pain) [Ref.]