>Corresponding Author : Jingjing Cai
>Article Type : Case Report
>Volume : 3 | Issue : 1
>Received Date : 13 March, 2023
>Accepted Date : 23 March, 2023
>Published Date : 28 March, 2023
>DOI : https://doi.org/10.54289/JAAD2300101
>Citation : Cai J. (2023) Anesthetic Management of a Case of Airway Bleeding During Pulmonary Artery Mass Resection. J Anaesth Anesth Drug 3(1): doi https://doi.org/10.54289/JAAD2300101
>Copyright : © 2022 Cai J. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access
Department of Anesthesiology, West China Hospital, Sichuan University, Chengdu, Sichuan, China
*Corresponding author: Jingjing Cai, Department of Anesthesiology, West China Hospital, Sichuan University, Chengdu, Sichuan, China
Abstract
Airway bleeding is an uncommon complication of pulmonary artery surgery. It can be caused by fragile bronchopulmonary collateral, vessel perforation, and reperfusion pulmonary edema. Early discovery of the breach and anesthetic management are very important for the prognosis of the patients.
We present a case of 58-year-old female diagnosed with left pulmonary artery mass. After the resection of the mass, the surgeon injected saline into the pulmonary artery and the patient was ventilated manually. Air bubbles were found in the artery, indicating a breach between the airways and the pulmonary circulation. Fiberoptic bronchoscopy revealed the breach on the lateral wall of the left lower bronchus. We replaced the single lumen endotracheal tube with a 32 left-sided double-lumen endobronchial tube to prevent the contamination of the right lung. After a consultation with the thoracic department, left lower lung lobectomy was performed.
Keywords: Airway Bleeding; Pulmonary Embolism; Anesthetic Management
Abbreviations: LPA: Left Pulmonary Artery, MPA: Main Pulmonary Artery, CPB: Cardiopulmonary Bypass, POD: Postoperative Day
Introduction
Pulmonary artery mass resection is a challenging procedure. Airway bleeding is one of the complications. Timely intraoperative diagnosis and treatment are of great significance for the patient.
Case Presentation
We present a case of 58-year-old female diagnosed with left pulmonary artery mass. The disease was found occasionally via physical examination. She didn’t complain about fever, cough, syncope, chest pain and short of breath. PET/CT showed the mass in the left pulmonary artery (LPA) and upper and lower pulmonary artery branches (Figure 1). The glucose metabolism was increased. Pulmonary embolism was a possible diagnosis and tumorigenic lesion was considered. The transthoracic echocardiogram showed dilated main pulmonary artery (MPA), LPA and right pulmonary artery. No significant abnormalities were found in the visible segment of the lumen. The acceleration time of pulmonary valve antegrade flow was about 137 cm/s and subvalvular regurgitation was Vmax=2.2 m/s, PG=20 mmHg. Tricuspid valve has a mild regurgitation of Vmax=3.1 m/s, PG=37 mmHg, according to which the systolic pressure of pulmonary artery was estimated to be about 40 mmHg. Lung perfusion imaging of SPECT showed the diffuse radioactive sparing of the left lung and V/Q mismatched.
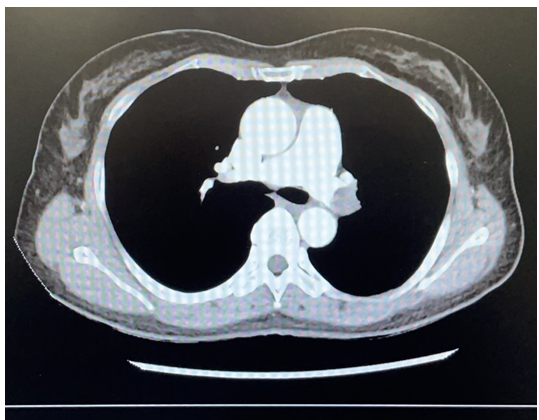
Figure 1: CT showed the mass in the left pulmonary artery.
The anesthetic induction and the resection of the LPA mass were uneventful under cardiopulmonary bypass (CPB)and deep hypothermic circulatory arrest. When the procedures were completed, the surgeon injected saline into MPA and the patient was ventilated manually. Air bubbles were found in the artery, indicating a breach between the airways and the pulmonary circulation. LPA was accompanied by the left bronchus, and it was possible to injure the wall of the bronchus while stripping the mass in the vessel, resulting in shunt between the two lumens. To further confirm the diagnosis, we performed intraoperative fiberoptic bronchoscopy. It showed active bleeding in the left bronchus (Figure 2) and no bleeding in the right bronchus. Careful examination revealed that the location of the breach was on the lateral wall of the left lower bronchus. In order to avoid contamination of the right lung, we replaced the regular single lumen endotracheal tube with a 32 left-sided double-lumen endobronchial tube. After a consultation with the thoracic department, we decided to perform left lower lung lobectomy. The procedure was completed while rewarming. The separation from CPB went smoothly and the patient was send to ICU after the surgery.
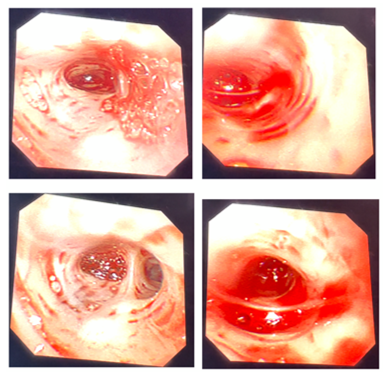
Figure 2: Fiberoptic bronchoscopy showed active bleeding in the left bronchus.
Postoperative fiberoptic bronchoscopy in ICU showed that the mucosa of the left upper lobe was obviously congested and edematous, and the bronchus of the left lower lobe was blocked. There was no obvious abnormality in the segments and mucosa of the right lung. The tracheal intubation was removed on the 3rd postoperative day (POD). The patient returned to the general ward on the 4th POD and was discharged in a stable condition on the 9th POD.
Discussion
Airway bleeding is an uncommon complication of pulmonary artery surgery but has a high mortality rate. Its pathogenesis includes rupture of fragile bronchopulmonary collateral [1], vessel perforation [2], and reperfusion pulmonary edema [1]. During deep hypothermic circulatory arrest, it is not easily detected because there is no blood flow in the pulmonary artery. When the surgeon highly suspects the possibility of vessel perforation, injecting saline into the artery and ventilating manually should be performed. The absence of air bubbles implies no damage to the vessel wall.
If airway bleeding is detected after separation from CPB, the management strategy is based on the patient’s circulation and oxygenation condition. If the circulation is stable and oxygenation can be maintained, treatment with vasoconstrictors [3], positive end‑expiratory pressure, reversal of heparinization, and correction of coagulation can be given. Attention should also be paid to control pulmonary artery pressure, which means avoidance of inadequate anesthesia, hypercapnia, and hypoxemia. If the circulation is unstable and oxygenation can’t be maintained, the anesthesiologist should restart CPB and perform fiberoptic bronchoscopy. If the bleeding is bilateral, treatment with vasoconstrictors, positive end‑expiratory pressure, reversal of heparinization, and correction of coagulation should be considered. If the bleeding is unilateral, lung isolation maybe useful and surgical procedures can be considered. Surgical procedures include vessel repair using a surgical absorbable hemostat [4], temporary overnight clamping of pulmonary artery [5], and bronchial occlusion with a Fogarty balloon catheter [6]. If circulation and oxygenation still can’t be maintained after surgical procedures, VV-ECMO [7] or VA- ECMO [8] should be considered.
Conflicts of interest: the author do not have any conflicts of interest to disclose.
References:
- Kanchi M, Nair HC , Natarajan P, Punnen J, Shetty V, et al. (2021) Management of intrapulmonary hemorrhage in patients undergoing pulmonary thrombo-endarterectomy. Ann Card Anaesth. 24(3): 384-388. [PubMed.]
- Morsolini M, Azzaretti A, Orlandoni G, Armini AMD. (2013) Airway bleeding during pulmonary endarterectomy: the "bubbles" technique. J Thorac Cardiovasc Surg. 145(5): 1409-1410. [PubMed.]
- Manecke GR, Jr Kotzur A, Atkins G, Fedullo PF, Auger WR, et al. (2004) Massive pulmonary hemorrhage after pulmonary thromboendarterectomy. Anesth Analg. 99(3): 672-675. [PubMed.]
- Shetty DP, Nair HC, Shetty V, Punnen J. (2015) A novel treatment for pulmonary hemorrhage during thromboendarterectomy surgery. Ann Thorac Surg. 99(3): e77-78. [PubMed.]
- Reddy S, Rajanbabu BB, Kumar NKS, Rajani I. (2013) Temporary clamping of branch pulmonary artery for pulmonary hemorrhage after endarterectomy. Ann Thorac Surg. 96(4): 1459-1461. [PubMed.]
- Yıldızeli B, Arslan Ö, Taş S, Eldem B, Aksoy E, et al. (2014) Management of massive pulmonary hemorrhage following pulmonary endarterectomy. Thorac Cardiovasc Surg. 62(1): 89-91. [PubMed.]
- Thistlethwaite PA, Madani MM, Kemp AD, Hartley M, Auger WR, et al. (2006) Venovenous extracorporeal life support after pulmonary endarterectomy: indications techniques and outcomes. Ann Thorac Surg. 82(6): 2139-2145. [PubMed.]
- Berman M, Tsui S, Vuylsteke A, Snell A, Colah S, et al. (2008) Successful extracorporeal membrane oxygenation support after pulmonary thromboendarterectomy. Ann Thorac Surg. 86(4): 1261-1267. [PubMed.]