>Corresponding Author : Sahida Abedin
>Article Type : Research Article
>Volume : 1 | Issue : 1
>Received Date : 26 November, 2021
>Accepted Date : 16 December, 2021
>Published Date : 18 December, 2021
>DOI : https://doi.org/10.54289/JCCP2100103
>Citation : Abedin S. (2021) Screening of Cervical Cancer by HPV DNA Testing and Novel Oncoe6 Cervical Assay at North Central Part of Bangladesh. J Cancer Cancer Prev 1(1): doi https://doi.org/10.54289/JCCP2100103
>Copyright : © 2021 Abedin S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Research Article | Open Access
Consultant, Microbiology National Institute of Cancer Research and Hospital, Mohakhali, Dhaka
*Corresponding author: Sahida Abedin, Consultant, Microbiology National Institute of Cancer Research and Hospital, Mohakhali, Dhaka
Abstract
Background: Cervical cancer is the fourth most common cancer in women worldwide. Human papillomavirus (HPV) is considered as the main cause of invasive cervical cancer and cervical intra-epithelial neoplasia. So, screening of cervical cancers by HPV DNA testing and oncoE6cervical test may play a potential role in early detection and management of cervical cancer.
Objectives: The objectives of the study were to detect HPV DNA by nested PCR and OncoE6protien expressed by HPV type 16 or 18 by using OncoE6 cervical test who are attending at tertiary care hospital at north central part of Bangladesh.
Methodology: A cross sectional observational type of study was done at the department of Microbiology, Mymensingh Medical College. About 280 clinically suspected individuals underwent for VIA, colposcopy, histopathology for grading, oncoE6cervical test and nested PCR.
Result: Among 280 cases 120 were VIA (42.85%) positive and 50 (VIA positive) cases were histopathologically positive (41.66%). Out of 120 VIA positive patients, 18 (15%) were OncoE6 positive and 160 VIA negative patients, 3 (1.875%) were positive by OncoE6 cervical test. Among 18 OncoE6 positive 16 (88.88%) patients were positive for HPV-16 and 02 (11.11%) for HPV-18 by OncoE6 cervical test. The sensitivity and specificity of OncoE6cervical test considering the PCR as gold standard were 87.5% sensitive and 100% specific respectively, were done for all cases.
Conclusion: With the above background, this study was carried out for screening of cervical cancerin the patients from Northern part of Bangladesh by different methods including HPV DNA testing and novel, low cost effective immunochromatographic molecular test. Thus, it may be concluded that early detection with HPV DNA testing and HPVOncoE6protein test may minimize the overtreatment as well as the colposcopy referral. So, it can be used as primary screening tool to identify real disease as well as save many lives of women.
Keywords: OncoE6protein test, HPV DNA testing, VIA (Visual inspection with acetic acid), neoplasia.
Abbreviations: CDC: The Centers for Disease Control and Prevention, HPV: Human papillomavirus, VIA: Visual inspection with acetic acid, CIN: cervical intraepithelial neoplasia, ORF: open reading frame, E: early, L: late.
Introduction
Nowadays Cervical cancer become one of the health challenging issue for women worldwide. The Centers for Disease Control and Prevention (CDC) estimates that at least half of all sexually active individuals are likely to acquire HPV infection at some point in their lives, whereas at least 80% of women may acquire this pathogen before the age of 50. Genital persistent infection with high-risk HPV has been firmly established biologically and epidemiologically as playing a causal role in all types of cancer of the uterine cervix; however, other cofactors are necessary for progression of the low-grade cervical lesions to cancer [1]. The greatest burden of disease is in developing countries, but in spite of better screening and surveillance cervical cancer is still a significant burden also in developed world [2]. According to WHO, there are approximately 500,000 new cases and 250,000 deaths from cervical cancer every year worldwide [3].
Some HPV infections persist, and a subset of persistent infections may progress to cervical intraepithelial neoplasia (CIN) or invasive cancer. Because neoplastic changes typically take some years to occur and it is depend on multiple factors like age, parity, sextual behaviour etc. Oncoprotein E6 and E7 play an important role in the development of cervical cancer which can be detected by OncoE6 cervical test .In North India, the percentage prevalence of high risk HPV in case of squamous cell carcinoma in decreasing order are- HPV 16 (64.8%), 18 (14.7%), 45 (6.4%), 33 (6.4%), 35 (5%), 58 (3.8%), 59 (2.1%), 56 (1.9%), 31 (1.7%) and 51 (1.4%) and in case of adenocarcinoma percentage prevalence are- HPV 16 (51.7%), 18 (34.5%), 31 (6.9%), 62 (5.9%), 33 (3.5%), 42 (3.5%) and 45 (3.5%) Globally, HPV type 16 and 18 contribute to over 70% of all cervical cancers, while HPV types 31, 33, 35, 45, 52 and 58 are responsible for approximately 20% cases [4].
HPV are small, non-enveloped, icosahedral double-stranded DNA viruses of Papillomavirus family [5]. The genomes of all HPV types contain eight ORFs (open reading frame). The ORF can be divided into three functional parts: the early (E) region encodes proteins (E1–E7) necessary for viral replication, the late (L) region encodes the structural proteins (L1–L2) required for virion assembly; and a largely non-coding part called long control region (LCR) necessary for the replication and transcription of viral DNA. E6 and E7, the most important oncogenic proteins, inactivate the tumor suppressor genes p53 and Rb (Retinoblastoma) respectively resulting in uncontrolled proliferation of cells [2]. So, their gene products could potentially serve as highly specific biomarkers to identify high-grade precancerous lesions that may progress to cervical cancer if left untreated [6].
Methodology
A cross sectional observational study was carried out in the Department of Microbiology, Mymensingh Medical College, Mymensingh. All VIA positive and negative married women attending at colposcopy clinic of gynaecology and obstetrics department of Mymensingh Medical College Hospital, Mymensingh were selected as subjects. Informed written consent was taken from each patient before her entry into the study. Nonprobability purposive type of sampling technique was used. Sample size was forty-seven. Cervical tissue was taken by endocervical swab. Inclusion criteria was All the VIA positive married women attending at colposcopy clinic for cervical cancer screening with or without symptoms. Exclusion criteria for cases were Patients who were pregnant, patients who were below 20 years of age, patients who were menstruating.
2.1. Data collection and analysis: A set of questionnaires was used for each of cases. All the relevant information and data were systematically recorded in a pre-designed data sheet. The data was analyzed in computer using appropriate statistical method.
Laboratory procedures:
3.1. Collection of specimen: Cervical swab specimen was collected prior to application of acetic acid or iodine for colposcopy examination. Excess mucous was removed from the cervical os and surrounding ectocervix by using a cotton or dacron swab. Swab was discarded. For OncoE6 cervical test samples were collected from the endocervical opening and the ectocervix by inserting the swab just inside the cervical os so that the tip reached a depth of approximately 0.5 cm and by rotating the swab 3 turns in a counter clockwise fashion. Then the surface of the ectocervix was gently wiped. The specimen was stored in the supplied tube without buffer until tested. If the specimen was not used immediately, it was refrigerated at -20 °C. Specimen was thawed for approximately 10 min at ambient temperature before being tested.
3.2. Procedure of OncoE6 cervical test: A cervical Specimen collected using a polyester swab was stored in a tube without buffer until tested. The specimen was prepped sequentially by treating the swab with a lysis solution (930µl) for 15 minutes, a conditioning solution (87µl) for 15 minutes, and then clarifying the specimen solution using a table-top microcentrifuge (10 minutes at > 10,000 rpm) to separate sample lysate from cellular debris. A 0.2 mL aliquot of the clarified specimen solution was then transferred into a Detector Reagent C vial with lyophilized detector monoclonal antibody alkaline–phosphatase conjugate. The test strip with immobilized capture monoclonal antibodies was inserted into Detector Reagent C vial containing specimen-conjugate mixture and the solution was permitted to migrate up the strip by capillary action. After 55 minutes, the test was washed by wash solution (200µl) for 12 minutes and then immersed into the developing solution (650µl) containing the alkaline–phosphatase substrate (Nitroblue Tetrazolium). After 15 to 25 minutes (depending on the ambient temperature), the test unit was removed from the developing solution vials and placed on a reading guide, allowing for visual inspection. Appearance of one or more test lines indicates E6 oncoprotein of the corresponding HPV type present in the initial cervical swab specimen. Results must be read within 3 minutes.
3.3. Storage of specimen: The specimens (both serum cervical swab) were stored at -20 °C for longer duration.
3.4. Polymerase chain reaction (PCR): Detection by PCR from cervical swab was performed by using standard protocol with specific primers for detection of HPV.
3.5. Three major steps of PCR: includes DNA extraction cervical swab samples, DNA amplification in thermal cycler and visualization/documentation under UV light.
3.6. DNA extraction from cervical swab: Frozen cervical swab samples were thawed at room temperature and centrifuged at 12,000 rpm for 15 minutes. Supernatant was discarded. The pellet was suspended in 200 μl of digestion buffer [100mM Tris–Cl (pH 8.0), 5mM EDTA (pH 8.0), 1% SDS] containing freshly thawed proteinase K (20 μg/μl). The sample was then incubated at 55 °C in a water bath overnight.
The digested sample was extracted with phenol - chloroform.
3.7. Phenol-Chloroform Extraction Materials:
• Tris-saturated phenol: chloroform - 1:1DNA amplification in thermal cycle
• Preparation of master mixture for each reaction (PCR mixture) contained
3.8. Protocol of thermal cycle: Initial denaturation at 95 °C for 3 minutes.
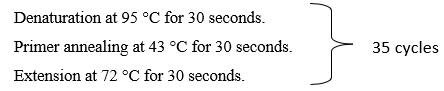
Final extension at 72 °C for 3 minutes.
Above step were repeated for 35 cycles in an automated DNA thermal cycler (DLin, China). Final extension was done at 72 °C for 3 minutes. The PCR products were run in 1.5% agarose gels stained with ethidium bromide and visualized under the UV transilluminator.
Primers used for PCR
HPV specific L1 antigen gene primers (Heah et al. 2012)
Primers
MY 09 F
MY 11 R
GP 5+ F
GP 6 +R
Primer sequence
5'-CGT CCM ARR GGA WAC TGA TC-3'
5'-GCM CAG GGW CAT AAY AAT GC-3'
5'-TTT GTT ACT GTG GTA GAT ACY AC-3'
5’-GAA AAA TAA ACT GTA AAT CAT ATT C -3'
Product size (bp)
450 bp
140 bp
3.9. Visualization and documentation: The amplified product was visualized by electrophoresis in 1.5% agarose gel then viewed in UV light and photographs were taken using digital camera.
Result:
Table I: Detection of OncoE6protein among VIA positive and negative cases by OncoE6 cervical test
Table I showed that among 280 suspected cases 120 were VIA positive and 160 cases were VIA negative. Among 120 VIA positive cases 18 (15%) were positive for OncoE6 cervical test and. Out of 160 VIA negative patients 3 (2.5%) were positive byOncoE6 cervical test.
| OncoE6cervical test done on 280 uj5cases | Number of VIA positive cases (n = 120) | Number of VIA negative cases (n = 160) |
|---|---|---|
| Positive | 18 (15%) | 3 (2.5%) |
| Negative | 102 (85%) | 117 (97.5%) |
| Total | 160 (100%) | 120 (100%) |
Table II: Comparison between OncoE6 cervical test (n = 21) and histopathological diagnosis (n = 50)
Table II represents histologically 50 diagnosed cases, out of 22 CIN I cases 01 (04%) and from 13 cervical carcinoma cases 12 (92.30%) were positive byOncoE6 positive test. The present study also revealed among 21 OncoE6 positive cases 4% (01/22) for CIN I, 37.5% (8/21) for CIN II,71.42 (7/21) for CIN III and 92.30% (12/13) for cervical carcinoma were positive for OncoE6protein.
| Histological diagnosis | Number of cases | OncoE6 positive cases (%) |
|---|---|---|
| CIN-I | 22 | 01 (04%) |
| CIN-II | 08 | 03 (37.5%) |
| CIN-III | 07 | 05 (71.42%) |
| Cervical carcinoma | 13 | 12 (92.30%) |
| Total | 50 | 21 |
Table III: Age distribution of PCR positive and OncoE6 positive cases among the study population (n = 280)
Table III showed that most of the PCR positive and OncoE6 positive cases of study population were in the age group ≥ 50 years followed by age group 30-39 years and 40-49 years.
| Age group in years | Number of PCR positive cases | Number of OncoE6 positive cases |
|---|---|---|
| 30-39 (160) | 07 (4.37%) | 06 (3.75%) |
| 40-49(70)) | 08 (11.42%) | 07 (10%) |
| ≥ 50 (50) | 09 (18%) | 08 (16%) |
| Total | 24 (33.79%) | 21 (20.75%) |
Table IV: Distribution of PCR positive and OncoE6 positive cases according to parity
Table IV showed that maximum number of PCR positive OncoE6 positive cases cases had more than 3children. HPV infection is most common among multiparous women. The result is statistically significant. So, there is association between multiparity and HPV infection.
| parity | PCR positive Cases (n = 24) | OncoE6 positive (n = 21) cases |
|---|---|---|
| Within 3 children (80) | 08 (33.33%) | 06 (28.57%) |
| More than 3 children (110) | 16 (66.66%) | 15 (71.43) |
| Total | 24 (99.99%) | 21 (100%) |
Table V: Sensitivity and Specificity of OncoE6 cervical test considering PCR as gold standard.
Table V showed that all OncoE6 cervical test positive cases were also PCR positive. The sensitivity and specificity of OncoE6cervical test considering the PCR as gold standard were 87.5 % sensitive and 100% specific respectively.
| Test result | OncoE6 cervical test | Total | Sensitivity | Specificity | |
|---|---|---|---|---|---|
| Positive | Negative | ||||
| PCR positive | 21 | 03 | 24 | 87.5% | 100% |
| PCR negative | 00 | 256 | 256 | ||
| Total | 21 | 259 | 280 | ||
Discussion:
Human papillomavirus (HPV) is considered as the main cause of most cervical cancers and cervical intraepithelial neoplasia (CIN) contributing to neoplastic progression through the action of viral oncoproteins mainly E6 and E7 and is thus an important public health challenge for the prevention of cervical carcinoma [6].
In the present study, out of 120 VIA positive cases, 18 (15%) were positive by OncoE6 cervical test. According to Zao et al from china detected OncoE6protein in 50.5% of VIA positive cases by OncoE6 cervical test [7]. Another study performed at Mymensingh by Nahar, F reported that among 47 VIA positive cases 21 (44.68%) were positive by OncoE6 cervical test [9]. Schweizer J et al in his study detected that out of 51 PCR positive cases 45 (88%) were positive by OncoE6 test positive which was consistent with the present study [9].
In the current study among160 VIA negative patients, 3 (1.86%) were positive by OncoE6 cervical test.
(Table I) This result could not be compared with other studies. It was the first study in Bangladesh that could detected OncoE6 protein from VIA negative cases. It indicates that OncoE6 cervical test was much better test than VIA for screening of cervical leisons.
(Table II) The present study also revealed among 21 OncoE6 positive cases 4% (01/22) for CIN I, 37.5% (8/21) for CIN II,71.42(7/21) for CIN III and 92.30% (12/13) for cervical carcinoma were positive for OncoE6protein.Nahar, F (2016) found 01/11 (9.09%) CIN I cases and 20/22 (90.90%) of cervical carcinoma were positive by OncoE6 cervical test [9]. Zhao et al (2012) showed 8.5% and 84.6% were OncoE6 positive in CIN I and cervical carcinoma respectively which were similar with the present study [7]. According to the study percentages of E6 positive increased steadily with increasing severity of leisons. The OncoE6 Cervical Test is able to predict which patients without lesions on biopsy would one year later develop disease (CIN3+) and which patients with abnormal biopsy would regress without treatment. It is found that one out of two women testing positive by the OncoE6 Cervical Test needed treatment, while only one out of ten women with positive HPV DNA or VIA test results required treatment.
From (Table III) In this study an important finding was the age-related distribution of HPV lesions. Most of the cases were in the age group 30-39 years but OncoE6 positive in the age group of ≥ 50 (38.90%). According to Zhao, et al. (2013) the highest OncoE6positive was in women aged 50 years and older which similar to the present study [7]. Because development of cervical cancer it takes more than 10 years. Moreover, women in the menopausal period have reduced immune functions with decreased viral clearance rates and increased HPV infection.
The current study (Table IV) showed that most of the OncoE6 positive cases 71.42% had parity more than 3 children and above. According to Jensen HPV infection was most common among multiparous women 83.3% which was similar with the present study [9]. Local tissue damage during vaginal delivery or cellular oxidative stress with increased likelihood of chance of HPV integration may be possible mechanisms. A role of vaginal delivery was supported by findings from a multicentre study in which an increased risk for cervical cancer. According to Delvenne et al explained that high levels of oestrogen and other sex hormones appear to be involved in cervical carcinogenesis and has been suggested to stimulate HPV gene expression [10]. So, there is association between multiparity and HPV infection.
In the current study, PCR and OncoE6cervical test were done on all the 280 cases as screening test. (Table -V) The sensitivity and specificity of OncoE6cervical test considering the PCR as gold standard were 87.5 % and 100% respectively. According to Nahar, F (2016) the sensitivity and specificity of OncoE6 cervical test were 75% and 100 % respectively which was similar with present study [8].
The sensitivity was less due to OncoE6cervical test only detected HPV-16 and HPV-18 type but unable to detect other high risk HPV types which responsible for cervical cancer. In addition, the elevated expression of E6 is required for epithelial cell transformation to cause cancer. So, detection the oncoE6 proteins represents an attractive, disease specific viral biomarker.
Conclusion:
Based on the findings of the present study, it may be concluded that screening of HPV with E6Oncoprotein is effective tool for the referrals to colposcopy or the overtreatment. The simplicity of use and high specificity of OncoE6 suggests application in high HPV prevalence, high risk population. So,future research should focus on practical application of these screening tools at the regional or national level.
Limitations:
• There are very few similar studies found in the world, so we could not compare those with the present study.
• Non availability as well as high cost of the reagents in the local market.
References
- Fernandes VJ, Meissner VDR. (2011) Human papillomavirus prevalence in women with normalcytology and with cervical cancer in Natal, Brazil. 4(6): 1321-1326. [PubMed.]
- Haghshenas M, Golini-Moghaddam T, Rafiei A, Emadeian O, Shykhpour A. (2013) ‘Prevalence and type distribution of high- risk human papillomavirus in patients with cervical cancer: a population – based study’. Infectious Agents and Cancer. 8: 20-29. [Ref.]
- YI Yang YS, Smith-McCune K, Darragh TM, Lai Y, Lin J. (2012) Direct human papillomavirus E6 whole-cell enzyme linked immunosorbent assay for objective measurement of E6 oncoproteins in cytology samples. ASM Journal. 19(9): 1474-1479. [PubMed.]
- Walboomers JM, Manos MM, Bosch JA, Jacobs MV, Kummer JA, et al. (1999) Human papillomavirus is a necessary cause of invasive cervical cancer worldwide, Bloomberg School of Public Health. 189: 12–19. [PubMed.]
- Bernard E, Pons-Salort M, Heard J, Delarocque-Aotagneau E, Guillemot D, et al. (2013) Comparing human papillomavirus prevalences in women with normal cytology or invasive cervical cancer to rank genotypes according to their oncogenic potential: a meta-analysis of observational studies. 94: 1-11. [PubMed.]
- Rahman T, Tabassum S, Jahan M, Nessa A. (2013) ‘Detection and estimation of human papillomavirus viral load in patients with cervical lesions’, Bangladesh Med Res Counc Bull. 39(2): 86-90. [PubMed.]
- Zhao FH, Jeronimo J, Qiao YL, Schweizer J, Chen W, et al. (2013) ‘An evaluation of novel, lower cost molecular screening tests for human papillomavirus in rural china’, Cancer prevention research. 66(9): 938-948. [PubMed.]
- Nahar F. (2016) ‘Detection of E6 Oncoprotein by Onco E6 cervical test and DNA of human papilloma virus by PCR from endocervical swabs of the patients attending at colposcopy clinic of Mymensingh Medical College Hospital (MMCH), Mymensingh’ M. Phil (Microbiology) Thesis, BSMMU (Published), Department of Microbiology, Mymensingh Medical College, Mymensingh. [Ref.]
- Schweizer J, Mahoney CW, Bergery MB, Ho M, Ramasamy V. (2010) ‘Feasibility study of a Human Papillomavirus E6 Oncoprotein test for diagnosis of cervical precancer and cancer’, Journal of Clinical Microbiology. 48(12): 4646-4648. [Ref.]
- Delvenne P, Herman L, Kholod N, Caberg JH, Herfs M, et al. (2007) ‘Role of hormone cofactors in the human papillomavirus-induced carcinogenesis of the uterine cervix’, Mol Cell Endocrinol. 264(1-2): 1–5. [Ref.]