>Corresponding Author : Saïd Haddadi
>Article Type : Case Report
>Volume : 2 | Issue : 1
>Received Date : 01 March, 2022
>Accepted Date : 13 March, 2022
>Published Date : 16 March, 2022
>DOI : https://doi.org/10.54289/JCRMH2200102
>Citation : Haddadi S, El Mammeri M, Baba A, Touati R. (2022) Association Between Breast Carcinoma and Homolateral Axillary Lymph Node Tuberculosis: A Case Report. J Case Rep Med Hist 2(1): doi https://doi.org/10.54289/JCRMH2100102
>Copyright : © 2022 Haddadi S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access
Surgery Department A. Central Hospital of the Army Docteur Mohamed Seghir Nekkache. BP 244, 16205. Kouba Algiers
*Corresponding author: Saïd Haddadi, Surgery Department A. Central Hospital of the Army Docteur Mohamed Seghir Nekkache. BP 244, 16205. Kouba Algiers
Abstract
Introduction: The association between axillary tuberculosis and breast cancer is rare, and only about thirty cases have been described in the literature. This entity must be mentioned in an endemic country faced with the notion of tuberculosis contagion.
Case presentation: We report the case of a patient in whom the association between breast carcinoma and axillary tuberculosis discovery was fortuitous postoperatively. But retrospectivly her husband contracted the tuberculosis 30 years ago. She had mastectomy with axillary lymph node dissection because the tumour was multifocal. The carcinoma was classified as pT2N0M0 (stage IIA classification TNM) and she was only put on hormone therapy. After 5 years of follow-up, no recurrence was noted despite the therapeutic insufficiency.
Conclusion: Mammary lymph node tuberculosis is rare; it must be mentioned in the context of tuberculosis contagion or in front of the the presence of calcifications in the axillary area on the x-ray. At the slightest suspicion of this diagnosis, the operating parts should not be fixed but sent in the fresh state for a ZIEHL-NELSEN staining for the detection of Koch's bacillus or for a culture. The anti-tuberculosis treatment should be immediately started after the surgery. If the cancer target is indicated, it should not be started until after 1 month of tuberculosis treatment, given the risk of tuberculosis outbreak.
Keywords: Axillary lymph node tuberculosis - Anti-tuberculosis chemotherapy.
Introduction
The association of two major breast pathologies (cancer and tuberculosis) is on the one hand a rarity since only 30 cases have been published worldwide, on the other hand this constitutes a real challenge for the healthcare team. In this observation, we report the case of a patient operated on for breast cancer associated with ipsilateral axillary lymph node tuberculosis.
Case Presentation:
68-year-old patient B.K with a history of hysterectomy and hypertensive under treatment, obese (BMI at 30) admitted for the management of a multifocal mucinous adenocarcinoma of the left breast classified as cT3N0M0. Immunohistochemically, it is luminal A. The patient hasn’t any familiar history of breast carcinoma. The patient underwent a mammectomy with ipsilateral axillary lymph node dissection after his informed consent. The histological study found 04 tumor foci, the largest of which measures 03 cm corresponding to a grade II mucinous carcinoma of SBR with healthy surgical limits. There were no metastases on the 13 lymph nodes of the dissection (N0 / N13). The tumor was classified as pT2N0M0 (stage IIA classification TNM 7th edition 2010 UICC). However, 10 lymph nodes are the site of caseo-follicular tuberculosis. This medical case was presented to our committee, and only hormone therapy was retained given the risk of an outbreak of lymph node tuberculosis under chemotherapy. The anti-HIV 1-2 serologies are negative and the patient was referred for anti-tuberculosis chemotherapy. With a follow-up of 05 years, the patient is alive without any neoplastic or tuberculosis recurrence.
Breast tuberculosis (BT) was first described by Sir ASHLEY COOPER in 1829 [1]. Even in endemic countries, BT is rare and affects 0.1% of all tuberculosis cases [2]. In 1899, WARTHIN demonstrated the possible coexistence between breast cancer and BT [3]. This encounter is very rare, it would occur in 0.0019% of cases according to KAPLAN [4].
Lymph node tuberculosis is one of the extra-pulmonary attacks of tuberculosis (EPT). EPT constitutes 20% of all cases and can reach up to 50% of cases in countries where HIV infection is endemic. Axillary tuberculosis involvement is seen between 3 and 13% of cases [1, 5-7]. The decrease in immunity linked to the development of cancer or HIV is thought to favor the tuberculosis transplant in these patients. This discovery is always fortuitous, and the notion of contage was absent in all the reported cases. Our patient, however, reports that her partner was treated for pulmonary tuberculosis about 30 years ago. According to KHURRAM et al, in 22 breast cancers, tuberculosis was not detected by the usual EHRLICH-ZIEHL-NIELSEN (EZN) stain (EZN), but by PCR, 11 cases of BT were found [8]. If this association is suspected, suspect tissues should not be fixed, but stored in serum for EZN or culture staining.
The presence of calcifications in the axillary area of lymphadenopathy on a frontal chest X-ray points to a tuberculous etiology [9].
There is no consensus for the treatment. In the 30 cases described in the literature, chemotherapy was used in 23 patients (76.66%). Radiotherapy in 13 cases (43.33%), and anti-tuberculosis drugs in 26 patients (86.66%). Tuberculosis drugs should be started immediately after surgery, for at least nine months. Chemotherapy can begin after 04 weeks of anti-tuberculosis treatment for BROUGHTON et al [10]. The dosage should be as follows: Rifampcin 450 mg / D, Isoniazid 300mg / D and Ethambutol 800 mg / D for 02 months, then Isoniazid-Rifampicin for 07 months.
Conclusion:
The association between TM and cancer poses a lot of problems for the healthcare team, given the lack of consensus. This entity should be sought especially in countries endemic to tuberculosis. Its identification allows first to revise the initial TNM classification in the lymph node downwards, and to institute an adequate treatment to avoid both an outbreak of tuberculosis and an undertreatment of breast cancer disease.
Conflicts of interest : The Authors declare that they have no conflict of interest.
Ethics approval : The ethic commity of our institution accepted the publication of this case report.
Consent to participate : Not applicable.
Consent for publication : The patient give us her consent for this publication.
Availability of data and material : The data and material have been used and disseminated legally and transparency.
Code availability (software application or custom code) : Not applicable
Authors' contributions : All the authors approuved the manuscrit and his contents.
Funding : The authors haven’t receive any financial support for this publication.
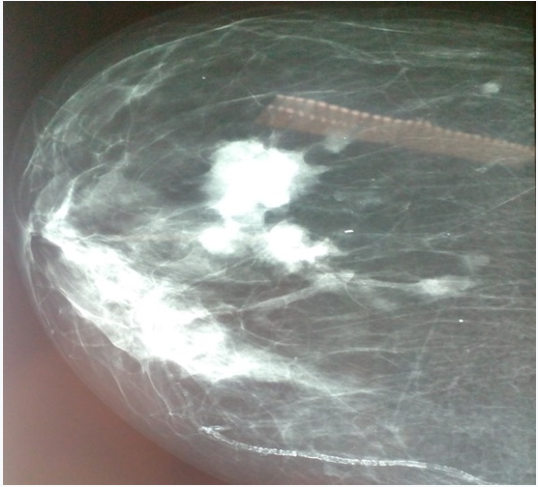
Figure 1: Mammography of the left breast showing a multifocal mucinous carcinoma luminal A associated with tuberculous lymph node.
References
- Kalac N, Ozkan B, Bayiz H, Dursun AB, Demirag F. (2002) Breast tuberculosis. Breast. 11(4): 346-349. [PubMed.]
- Ballini A, Zaritzky A, Lupo L. (1989) Breast tuberculosis and carcinoma. Isr Med Sci. 25: 339-340. [Ref.]
- Warthin AS. (1899) The coexistence of tuberculosis and carcinoma of the mammary gland. Am J Med Sci. 118: 25. [Ref.]
- Kaplan MH, Armstrong D, Rosen P. (1974) Tuberculosis complicating neoplastic disease. A review of 201 cases Cancer. 33(3): 850-858. [PubMed.]
- Shimoide H, Murata Y, Kusajima K, Oishi F, Hirayama N, et at. (1994) The status of extra-pulmonary tuberculosis in community hospital. Kekkaku. 69(8): 519-525. [Ref.]
- Dandapat MC, Mishra BM, Dash SP, Kar PK. (1990) Peripheral lymph node tuberculosis: a review of 80 cases. Br J Surg. 77(8): 911-912. [PubMed.]
- Akbulut S, Sogutcu N, Yagmur Y. (2011) Coexistence of breast cancer and tuberculosis in axillary lymph node: a case report and literature review. Breast Cancer Res Treatment. 130: 1037-1042. [PubMed.]
- Khurram M, Tariq M, Shahid P. (2007) Breast cancer with associated granulomatous axillary lymphadenitis: a diagnostic and clinical dilemma in regions with high prevalence of tuberculosis: a diagnostic ans clinical dilemma in regions with high prevalence of tuberculosis. Pathol Res Pract. 203(10): 699-704. [PubMed.]
- Takaaki F, Morihiko K, Yasuhiro Y, Tokihiro K, Hiroyuki K. (2003) Tuberculosis of axillary lymph nodes with primary breast cancer. Breast Cancer. 10(2): 175-178. [PubMed.]
- Broughton A, Galant C, Hainaut P. (2008) Simultaneous occurrence of metastatic breast cancer, Hodgkin’s disease and tuberculous lymphadenitis in homolateral axillary lymph nodes-a case report. Acta Clin Belg. 63(6): 391-393. [PubMed.]