>Corresponding Author : Bendahou H
>Article Type : Case Report
>Volume : 2 | Issue : 2
>Received Date : 26 June, 2022
>Accepted Date : 10 July, 2022
>Published Date : 20 July, 2022
>DOI : https://doi.org/10.54289/JCRMH2200108
>Citation : Bendahou H, Selmaoui M, Zagdane S, Yamoul J, Hayar S, et al. (2022) Severe Arrhythmia Caused by Abscess Endocarditis on a Bicuspid Aortic Valve: Case Report and Literature Review. J Case Rep Med Hist 2(2): doi https://doi.org/10.54289/JCRMH2200108
>Copyright : © 2022 Bendahou H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access
1Doctor, Cardiology department, Hospital university of Casablanca, Morocco
2Professor, Cardiology department, Hospital university of Casablanca, Morocco
*Corresponding author: Bendahou H, Doctor, Cardiology department, Hospital university of Casablanca, Morocco
Abstract
The incidence of infective endocarditis (IE) on the bicuspid valve is high with serious complications. Perivalvular extension is one of the most serious complications because it can be complicated by conduction disorders such as AV block or bundle branch block or rhythm disorders, often with a poor prognosis.
We report a rare case of infective endocarditis in a bicuspid aortic valve complicated by perivalvular abscess and trifasicular block.
Keywords: Infective Endocarditis; Root Aortic Abscess; Trifasicular Block
Abbreviations: IE: Infective Endocarditis, ECG: Electrocardiogram
Introduction
The bicuspid aortic valve is the most common congenital heart defect, affecting 1% to 2% of the population. Among the various complications, the incidence of infective endocarditis (IE) on the bicuspid valve is high with serious complications [1].
The perivalvular extension of infective endocarditis is one of the most serious complications with a prevalence of 10 to 40%, and which conditions the prognosis in these patients [2]. Thus, their detection is crucial in the overall care of the patient and particularly in surgical procedures [2].
The electrocardiogram (ECG) is useful for monitoring patients, enabling the detection of conduction or rhythm disorders, which conditions the management and prognosis of these patients [3].
We report a rare case of infective endocarditis in a bicuspid aortic valve complicated by perivalvular abscess and trifasicular block.
Case report:
This is a 19-year-old girl, with no cardiovascular risk factors or particular pathological history, who presents to the emergency room for infective endocarditis. On somatic examination, we note an alteration in general state, Blood Pressure = 80/50 mmHg, sinus tachycardia at 140 bpm, fever at 40°, without signs of heart failure. On cardiac auscultation we find: A diastolic murmur at the 5/6 in aortic focus.
The electrocardiogram shows sinus tachycardia at 145 b/min, electric LVH, with no arrhythmia or conduction disorder (Figure 1).
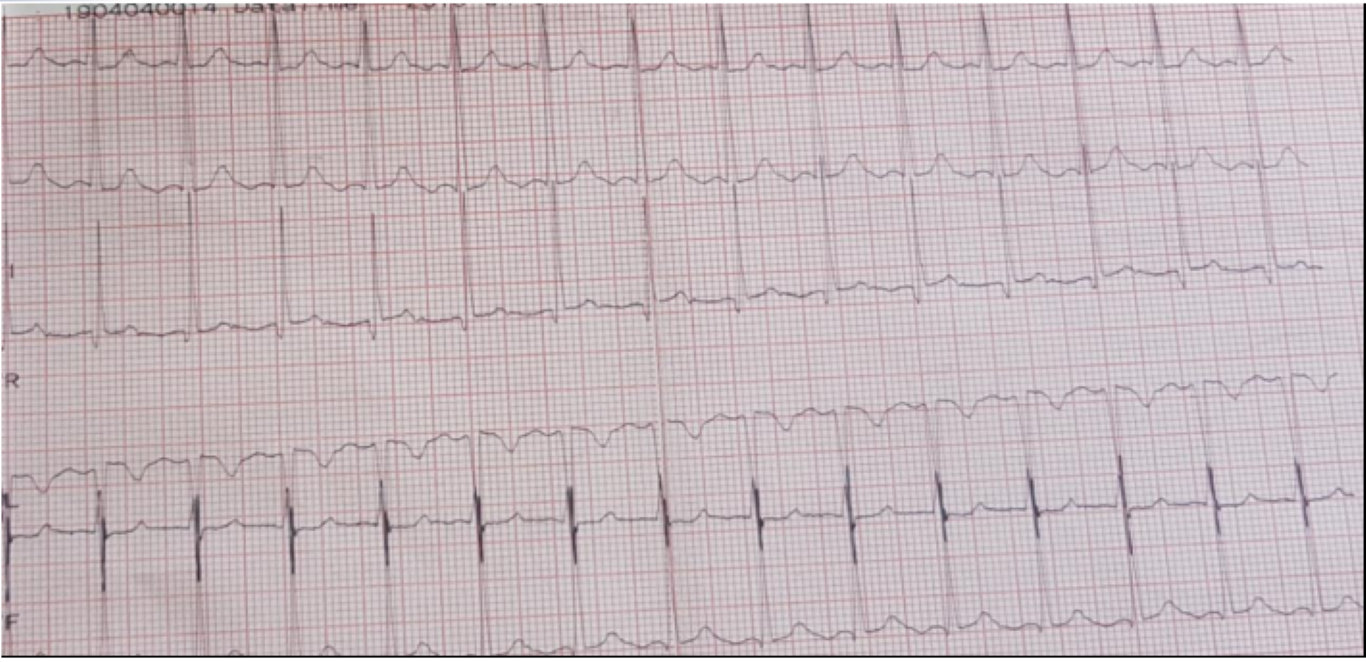
Figure 1: ECG showing sinus tachycardia at 140b/min.
On transthoracic echocardiography, we find an aspect of valvular dilated cardiomyopathy with the presence of 2 vegetations at the level of the aortic valve (Figure 2), severe aortic insufficiency on the bicuspid aortic, and an aneurysmal dilation of the ascending aorta (52 mm), (Figure 3) complicated by an abscess collected at the level of the mitral aorto trigone and a 2nd abscess between the Left and Right cusps of the aortic valve fistulized into the aorta (Figure 4).
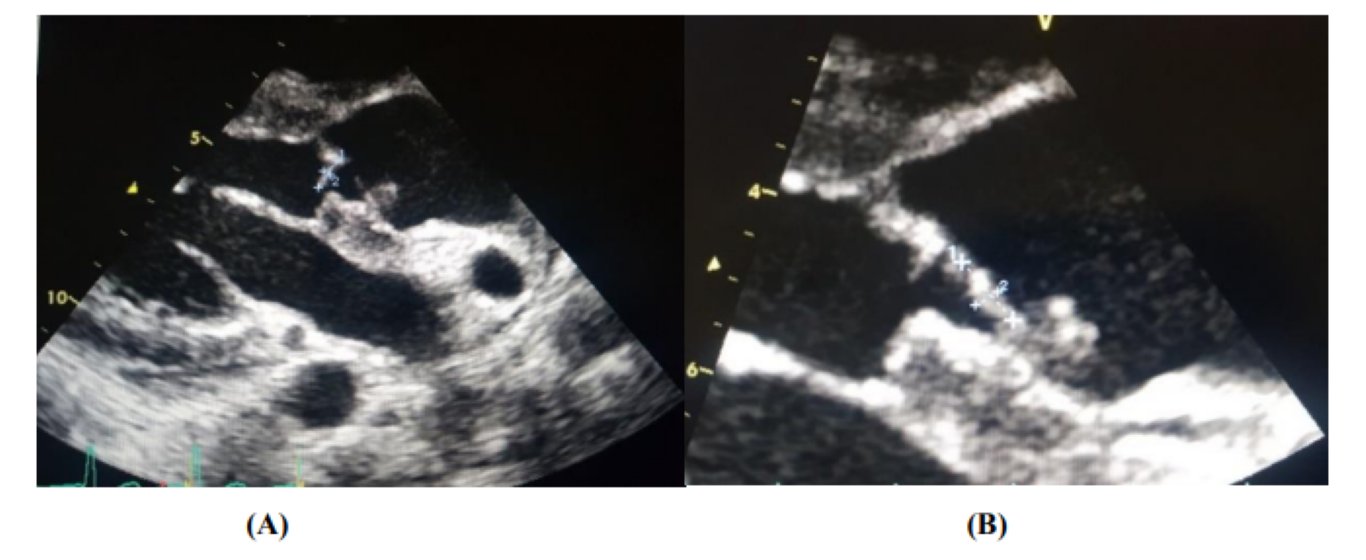
Figure 2: Image of two vegetations at the level of the aortic valve [On the ventricular side (A), and another on the aortic side (B)].
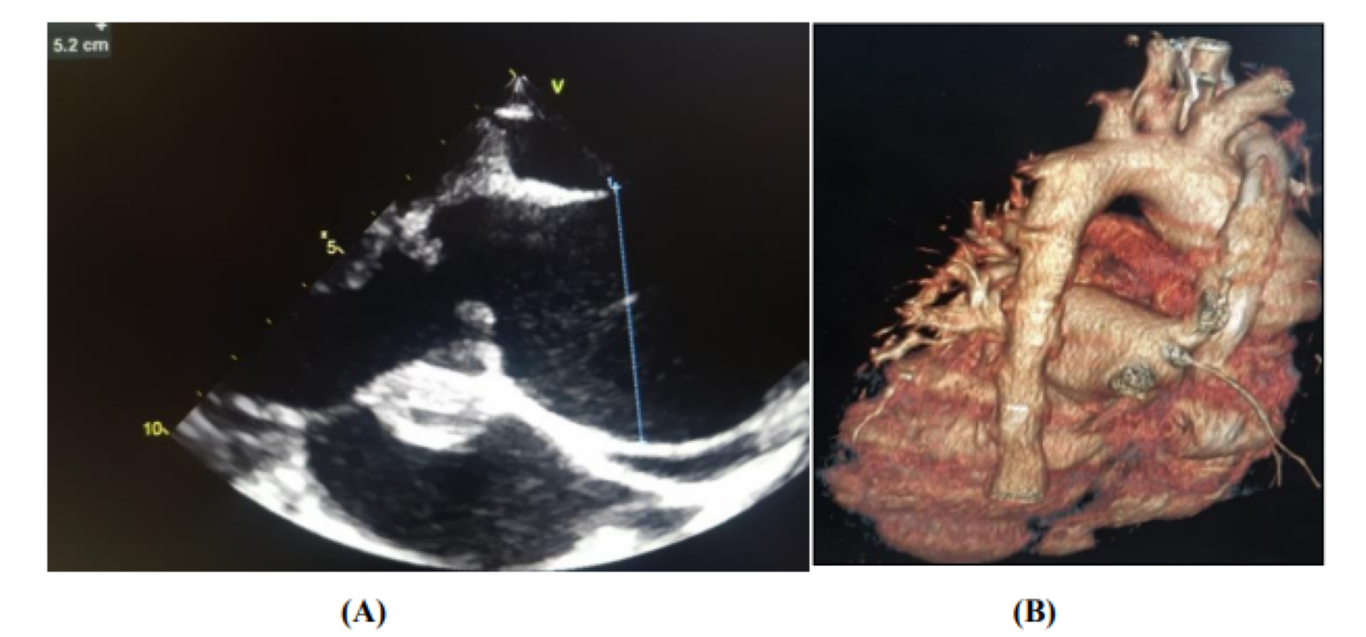
Figure 3: Appearance of aneurysmal dilation of the ascending aorta [Parasternal long axis on ETT (A), 3D reconstruction of chest CT angiography (B)]
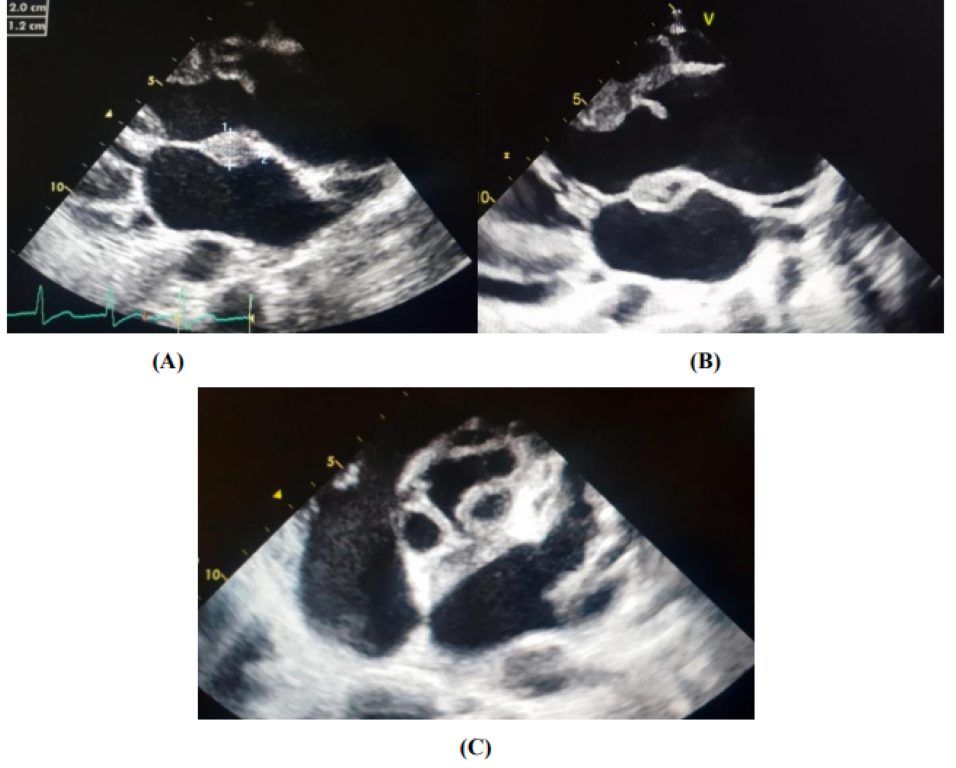
Figure 4: Perivalvular abscesses complicating an aortic IE [An abscess collected at the level of the aorto-mitral trigone (A, B) and a 2nd abscess between the Left and Right cusps of the aortic valve fistulized in the aorta (C)]
An infectious assessment carried out was disturbed with a CRP at 255mg/l, WBC at 33000e/µl, Pct at 8.9ng/l and two positive blood cultures isolating a multi-sensitive staphylococcus aureus.
A research extension report for secondary locations of infective endocarditis was carried out, namely proteinuria for 24 hours, an ophthalmological examination on the fundus, a cerebral CT, a chest CT, and an abdominal ultrasound being normal.
The diagnosis of infective endocarditis on severe aortic insufficiency with aneurysmal dilation of the ascending aorta and without secondary localizations was retained. The patient was put on intravenous antibiotic therapy adapted to the isolated germ. A surgical indication for a Bentall was posed.
The evolution was marked by the improvement of the clinical-biological infectious syndrome, but the worsening of the electrical signs on the ECG initially a BAV 1st degree (figure 5) then a transitory trifascicular block evolving quickly towards death following disorders severe rhythm « ventricular fibrillation » refractory to the necessary resuscitation measures.
Discussion:
Among the various complications of bicuspid aortic valve including aortic stenosis, aortic regurgitation, aortic dissection, the incidence of infective endocarditis in bicuspid aortic valve is high 10-30% in some series [1].
And perivalvular extension of infective endocarditis is a serious complication. Recognition of this complication has been greatly improved thanks to imaging, in particular TEE. A number of studies have been able to determine the risk factors and clinical course of patients with perivalvular extension during this serious infection [2].
Patients with infective endocarditis of the bicuspid aortic valve are often younger with a male predominance and have a higher incidence of perforation, valvular destruction, heart failure and valvular abscess formation, and perivalvular or myocardial. The perivalvular abscess, as reported in our clinical case above, causes conduction disorders following its rapid progression in the bundle of His or the AV node [1].
Perivalvular extension is more common in aortic endocarditis than in mitral or tricuspid valve involvement [3]. And often, the most incriminated germ is staphylococcus aureus [3].
The described prognosis is bleak with a high mortality rate requiring early diagnosis and therefore urgent surgical treatment [1].
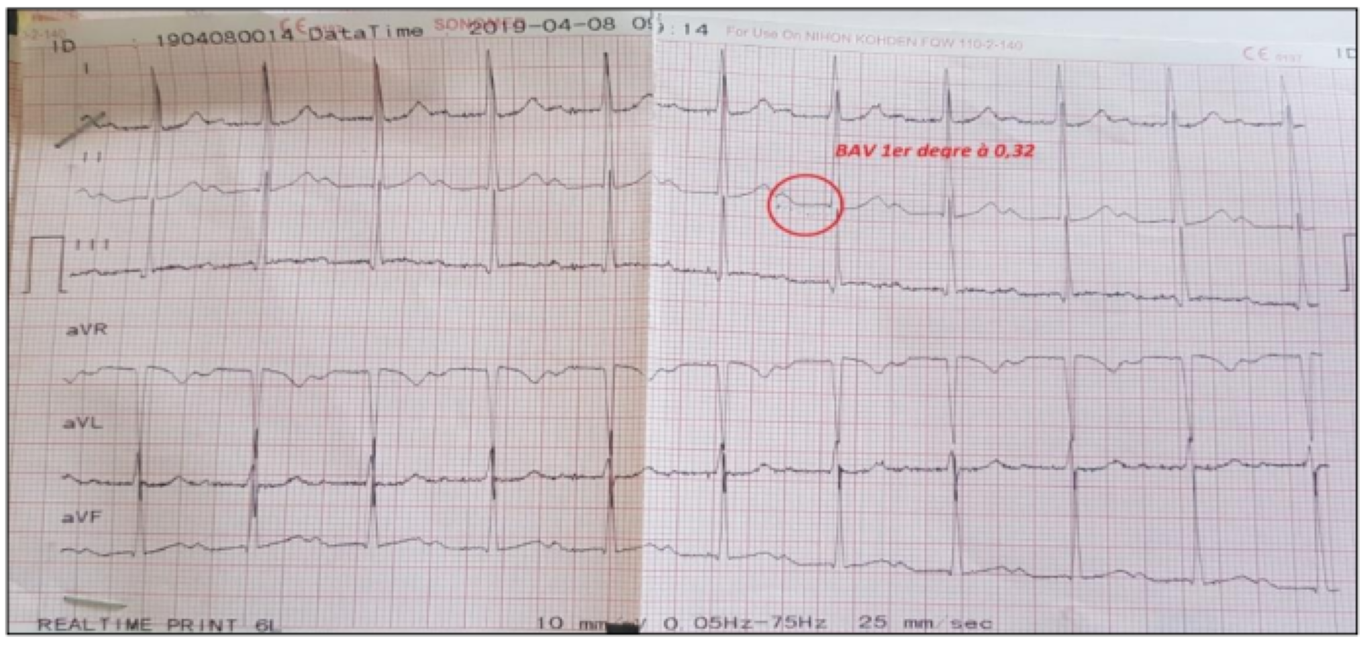
Figure 5: ECG appearance of a 1st degree BAV at 0.32mm.
Electrical aspects:
The conduction system of the heart is in close proximity to the aortic valve; the AV node is located at the apex of Koch's triangle, the boundaries of which are formed by the anterior border of the coronary sinus, the tricuspid ring and the tendon of Todaro, in the right atrium. Then the conduction system moves to the left, enters the central fibrous skeleton and appears between the right, non-coronal cusps. Finally, the conduction bundle splits into left and right branches. Given this close anatomical relationship, conduction abnormalities, such as complete atrioventricular block and bundle branch blocks, have been frequently reported as complications of perivalvular infection following aortic infective endocarditis [3].
In published data, one of the strongest predictors of perivalvular electrocardiographic complications was the occurrence of AV block and bundle branch blocks [4].
In fact, in several studies, the only reliable predictor of peri- and paravalvular abscess was the presence of atrioventricular block (including first-degree block) or previously undescribed bundle branch block [2,5]. This association reflects the tendency of the infection to extend into the weakest part of the paravalvular structures, the membranous septal zone which contains the conductive tissue, in particular the aorto-mitral trigone, as our clinical case reported here -above.
Echocardiography:
Transesophageal echocardiography reliably determines the presence of paravalvular abscesses. Transesophageal echocardiography allows rapid identification of abscesses, accurately defining cardiac anatomy, even in cases of aortic and/or prosthetic endocarditis or both. The precise anatomical information obtained is particularly useful for planning surgical approaches [5].
Microbiology:
The microbiological profile of patients with perianural extension in endocarditis varied between studies. In some studies, staphylococci were the predominant microorganisms. It would seem reasonable that virulent pathogens, such as staphylococci, could cause perannular destruction [2].
In particular, S. aureus is generally characterized by an acute presentation, without the classic physical signs. Its evolution is often fulminant when it involves the mitral or aortic valve, with generalized metastatic infection and death in about 25 to 30% of cases. 6 For this reason, many patients present with advanced disease and multiples complications, as in the case of our patient, who presented with severe complications from S. aureus endocarditis.
Staphylococcal strains that cause endocarditis are often resistant to microbicidal platelet proteins and elaborate proteolytic enzymes that facilitate spread to adjacent [2].
The treatment:
The treatment of infective endocarditis consists of the eradication of infectious foci, antimicrobial treatment and, if necessary, early surgical treatment.
There are different antimicrobial treatment regimens depending on the microbial agent, its drug susceptibility profile, and patient characteristics [2].
Surgical treatment in the active phase of the disease should be considered in the presence of heart failure or uncontrolled infection and to prevent embolic events.
The prognosis:
In-hospital mortality from infective endocarditis ranges from 10 to 26%. Heart failure, perannular complications and S. aureus infections as well as the appearance of conduction or rhythm disorders are the most powerful predictors of a bleak hospital prognosis [6].
However, the clinical evolution of patients with perivalvular infection is of bleak prognosis, and surgery in these patients is technically difficult [2].
The long-term prognosis is highly variable and depends mainly on age, the presence of heart failure and comorbidities [6].
Conclusion
Infectious endocarditis on the bicuspid aortic valve is a rare condition that can be complicated by a perannular abscess. Early detection and prompt intervention could prevent complications from perannular extension. The development of AV block type conduction disorders or bundle branch blocks often has a bleak prognosis. Serial ECGs and monitoring of electrical signs are of great interest for better management.
References
- Jaina R, Kaderb M, Sajeevc CG, Krishnand MN. (2015) Aortic root abscess presenting as alternating bundle branch block: Infective endocarditis of bicuspid aortic valve Rakesh. Cardiological Society of India. 0019-4832. [Ref.]
- Graupner C, Vilacosta I, SanRomán J, Ronderos R, et al. (2002) Periannular Extension of Infective Endocarditis. Journal of the American College of Cardiology. 39(7): 1204-1211. [PubMed.]
- Kariyanna PT, et al. (2020) Significant PR and New Onset Left Bundle Branch Block in Aortic Root Abscess: A Marker of Disease Progression and Poor Prognosis. Am J Med Case Rep. 8(9): 315-320. [PubMed.]
- Akram A, Ibe U, Kazi A. Twisting Tale of Infective Endocarditis. 1-Internal Medicine, St Mary's Hospital, Waterbury, USA. 2-Cardiology, Danbury Hospital, Danbury, USA. 3-Internal Medicine, Saint Mary's Hospital, Waterbury, USA. Cureus. 11(11): e6116. [Ref.]
- Karalis D, Chandrasekaran K, Wahl JM, Vilaro J, et al. (1995) Endocarditis-Associated Paravalvular Abscesses* Do Clinical Parameters Predict the Presence of Abscess? Emily A. Chest. 107: 898-903. [PubMed.]
- Sousa A, Lebreiro A, Sousa C, Correia AS, Almeida P, et al. (2012) An atypical presentation of infective endocarditis a- Cardiology Department. 829-832. [Ref.]