>Corresponding Author : Melisa Uruci
>Article Type : Case Report
>Volume : 2 | Issue : 3
>Received Date : 13 July, 2022
>Accepted Date : 25 July, 2022
>Published Date : 28 July, 2022
>DOI : https://doi.org/10.54289/JCRMH2200113
>Citation : Uruci M, Ruci D and Ajasllari N. (2022) Misdiagnose of Morbus Behcet. J Case Rep Med Hist 2(3): doi https://doi.org/10.54289/JCRMH2200113
>Copyright : © 2022 Uruci M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access
University Medical Center of Tirana "Mother Teresa"
*Corresponding author: Melisa Uruci, University Medical Center of Tirana "Mother Teresa"
Introduction
Behcet's disease is an inflammatory disorder of unknown aetiology, and many of its characteristic recurrent manifestations overlap with those of autoinflammatory diseases. Enhanced inflammatory response and over-expression of proinflammatory cytokines are the prominent features of Behcet's disease, and they are compatible with the findings in other autoinflammatory disorders [1]. Existing and new criteria were tested so: ocular lesions, oral aphthosis and genital aphthosis are each assigned 2 points, while skin lesions, central nervous system involvement and vascular manifestations 1 point each. The pathergy test, when used, was assigned 1 point. A patient scoring 4 points is classified as having BD [2,3]. Pemphigus vulgaris is a chronic autoimmune mucocutaneous disease that initially manifests in the form of intraoral lesions, which spread to other mucous membranes and the skin. The etiology of pemphigus vulgaris is still unknown. but is characterized by the production of autoantibodies against intercellular substances and is thus classified as autoimmune diseases. Most patients are initially misdiagnosed and improperly treated for many months or even years [4,5].
Case Presentation
Patient with initials K.M born on 31.12.1994 with morbid history for coloboma of the left eye, Hashimoto’s thyroiditis diagnosed in 2018 and iron deficiency anemia.
The patient refers that after the removal of a tooth, in January 2021 the story of the appearance of aphthae took place, initially presenting on her inner cheek and then on the tongue. She received treatment from her dentist with oral antiseptic solutions and gel, but without any positive result. At first it was thought of as for a local infection, for which she took antibiotic treatment but to no avail. Aphthae in her oral mucosa started transforming in ulcers which made impossible to feed. Under these circumstances, the patient presents herself to the outpatient service for a direct consult with the doctor, whom based on the clinical signs, the presence of oral and genital canker sores, also positive pathergy test, suspects of Behcet disease.
The patient started treatment with colchicine 2 mg/day, Azathioprine 100 mg/day and methylprednisolone 8 mg/day. This treatment lasted for 3 days only because the patient’s clinical conditions worsened. The patient’s oral and genital aphthae became extremely painful requiring her immediate hospitalization.
After hospitalization in rheumatology ward, in late april 2021 a series of examinations were performed starting from infectious disease tests with HbsAg neg, Anti HCV neg, HIV-1, -2 neg, inflammatory tests PCR 11,2mg/dL (0-5), fibrinogen activity478mg/dL (200-400), immunologic tests anti TPO 1000 IU/mL, TSH 3,809 IU/mL, pANCA neg, cANCA neg, HLA-B51 neg, HGB 11,2 me MCV, MCH, MCHC low.
During hospitalization, the patient was consulted by an infectious disease specialist and resulted in IgG and IgM positive serology for HSV-1 and HSV-2 and biopsy was performed from oral mucosal lesions. The patient was treated by the rheumatology clinic in collaboration with the infectious disease specialist with aciclovir, prednisone, vitamin therapy, supportive therapy and her condition improved.
Discussion and Conclusions
We must emphasize the fact that patients with pemphigus vulgaris are often misdiagnosed as having a more common illness that is seen more frequently by medical and dental professionals. Clinically, it can mimic other oral inflammatory conditions, such as lichen planus, candidiasis, and periodontal disease. The most common misdiagnoses are erythema multiforme, herpes simplex virus, and candida. It can also happen with Behcet disease because of its mucocutaneus lesions. A biopsy and immunofluorescent studies are needed to achieve a correct diagnosis [6].
So, during September 2021 she presented to the dermatologist with eroded aphthous lesions in the mucosa of the mouth, and in the genitals, as well as few bullous lesions in the abdominal area. The suspected cause of the recurrence of these lesions is linked to a decrease in cortisone treatment. After the patient refers the fact that the lesions in the mouth have never disappeared, it is considered by the dermatologist another clinical-histopathological re-evaluation. A second biopsy is performed, and the histopathological diagnosis is still not definitively determined between Behcet’s disease and Pemphigus Vulgaris.
During hospitalization the lesions progressed to numerous vesicular-bullous lesions on the trunk and extremities. It is brought to our attention that the vesicular and bullous cutaneous elements appear after a pruritus and erythematous elements. They were also associated with conjunctivitis that passed from one eye to the other periodically, for which she received treatment with cortisone local drops. Pathological lesions are already localized on the face, trunk, extremities, oral and genital mucosa [7].
Pemphigus Vulgaris is confirmed in the third biopsy with immunohistochemistry and antidesmoglein antibody [8]. In the meanwhile, the patient is kept on cortisone therapy and due to side effects, the initiation of rituximab therapy is expected.
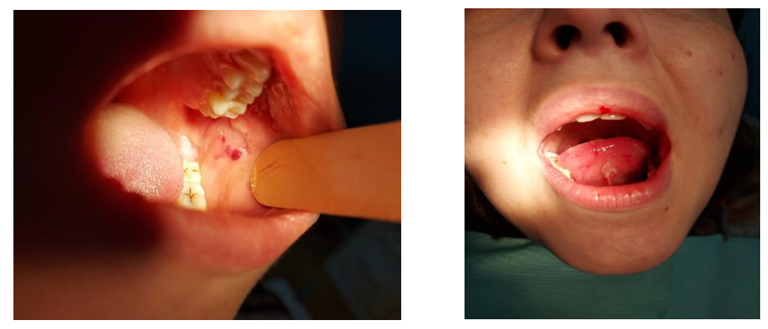
Photos of lesions - Oral aphtoe

Photos of skin lesions

Genital lesions
References
- Gül A. (2005) Behçet's disease as an autoinflammatory disorder. See comment in PubMed Commons below Curr Drug Targets Inflamm Allergy. 4: 81-83. [PubMed.]
- (2006) International Team for the Revision of the International Criteria for Behcet’s Disease. Revision of the International Criteria for Behcet’s Disease (ICBD). Clin Exp Rheumatol. 24. [Ref.]
- International Team for the Revision of the International Criteria for Behçet's Disease (ITR-ICBD). (2013) The International Criteria for Behçet's Disease (ICBD): a collaborative study of 27 countries on the sensitivity and specificity of the new criteria. [PubMed.]
- Chaudhary N, Chaudhary V, Goswami GK and Pathak AN. (2014) Case Report Open Access. Oral Pemphigus Vulgaris: A Case which was Misdiagnosed as Stomatitis. [Ref.]
- Dagistan S, Goregen M, Miloglu O, Cakur B. (2008) Oral pemphigus vulgaris: a case report with review of the literature. J Oral Sci. 50: 359-362. [PubMed.]
- Sirois D, et al. (2000) “Diagnostic Patterns and Delays in Pemphigus Vulgaris: Experience with 99 Patients.” Archives of Dermatology. 136(12): 1569-1570. [PubMed.]
- Flood D, Lezanski-Gujda A, Miletta NR. (2019) Diagnosing Pemphigus Foliaceus: A Rare Blistering Disease Masquerading as a Common Dermatologic Disorder. 84(5-6): e455-e457. [PubMed.]
- Mortazavi H, Shahdi M, Amirzargar AA, Naraghi ZS, Valikhani M, et al. (2009) Desmoglein ELISA in the diagnosis of pemphigus and its correlation with the severity of pemphigus vulgaris. 8(1): 53-56. [PubMed.]