>Corresponding Author : Musleh Mubarki
>Article Type : Case Report
>Volume : 2 | Issue : 4
>Received Date : 03 Aug, 2022
>Accepted Date : 13 Aug, 2022
>Published Date : 17 Aug, 2022
>DOI : https://doi.org/10.54289/JCRMH2200117
>Citation : Mubarki M, Alahmari M, Alahmari A, Magboul NA, Najmi A, et al. (2022) Myxoma of Paranasal Sinus, Case Report. J Case Rep Med Hist 2(4): doi https://doi.org/10.54289/JCRMH2200117
>Copyright : © 2022 Mubarki M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
Department of ORLHNS, Aseer central hospital, Aseer, KSA
*Corresponding author: Musleh Mubarki, Department of ORLHNS, Aseer central hospital, Aseer, KSA and Mohammed Alahmari, Department of ORLHNS, Aseer central hospital, Aseer, KSA
Abstract
Head and neck myxomas are uncommon neoplasms with few reports in the literature, only sporadic cases of myxomas of the temporal bone, pharynx, larynx, soft tissues of the face and neck, and paranasal sinuses have been reported, with the majority of these tumors arising from the mandible and maxilla. Recurrence rates might reach 25%, which is mainly due to insufficient first excision, we hereby, report a case of a nasal myxoma, endoscopic surgery was conducted, and surgical procedures aided in the total removal of the tumor.
Keywords: Nasal; Myxoma; FESS
Abbreviations: DNS: Deviated Nasal Septum
Introduction:
Myxomas are benign connective tissue tumors composed of stellate and spindle-shaped cells in a myxoid stroma with benign-appearing nuclei. They're most commonly found in the heart, soft tissues, muscles, and bones [1]. Nasal myxomas and paranasal sinus myxomas are quite uncommon. The mandible and maxilla are responsible for the majority of the neoplasia in the head and neck, The age varies from 11 months to the eighth decade, with a peak incidence of 25 to 35 years, and there is a little female predominance [2]. They're benign, however they can be invasive in certain area, soft tissue myxomas of the head and neck are uncommon, with fewer than 50 cases reported, on histological examination, a sinonasal myxoma consists of a loose proliferation of stellated, round, or spindled cells with thin cytoplasmic projection and hyperchromic tiny nuclei that are not encapsulated [3].
Case report
We discuss the case of a 50-year-old women who presented with a unilateral increasing nasal obstruction and was diagnosed with a allergic fungal polyp, For the past 4 months, she had a headache, a decreased sense of smell, snoring and occasional mucoid nasal discharge. Fever, epistaxis, or ocular complaints were not present.
Anterior rhinoscopy was used to do the clinical examination, which revealed a pink fleshy mass projecting from the inferior concha and extending to the nasal cavity on the left side, soft to firm in texture and did not bleed when touched. On the decongestion test, the mass did not regress, there was deviated nasal septum (DNS) to the right side. (figure 1), and CT was respect and show left maxillary sinus opacifications with homogeneous mass extension into the nasal cavity and was pushing the nasal septum in opposite side, Lamina was pushed laterally, with erosion of anterior superior and medial walls of the maxillary sinus was noted. (figure 2), and MRI with contrast was show lobulated left maxillary nasal mass heterogenous enhancement in intermediate T2 extend to left nasal cavity and erodes the left orbital floor (figure 3).
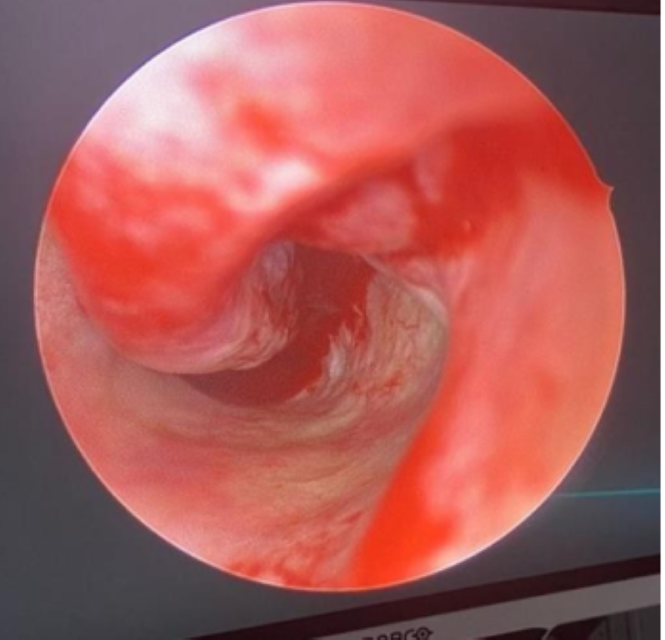
Figure 1: (pink fleshy mass projecting from the inferior concha the left side)

Figure 2: (left maxillary sinus opacifications with homogeneous mass extension into the nasal cavity with erosion of anterior superior and medial walls of the maxillary sinus)
Biobsy was taken and sent for histopathological examination, In the background of loose myxomatous and gelatinous stroma, the tumour was mostly made up of sparsely cellular spindle and stellate cells. Calcification, ossification, and chondroid differentiation foci were also observed, as well as a localized mononuclear cell infiltrate, there was no mitosis, cellular pleomorphism, or necrosis (figure 3). S 100 and calretinin immunohistochemistry were negative in the stellate cells, A myxoma histological diagnosis was provided.
Patient consented for surgery, radical primary resection has been achieved with modified denker procure using a microdebrider-assisted endoscopic sinus surgery approach, medial portion of anterior maxillary wall removed to enable access to all the antrum wall.
Bone was drilled out and all mucosa extracted (figure 5).
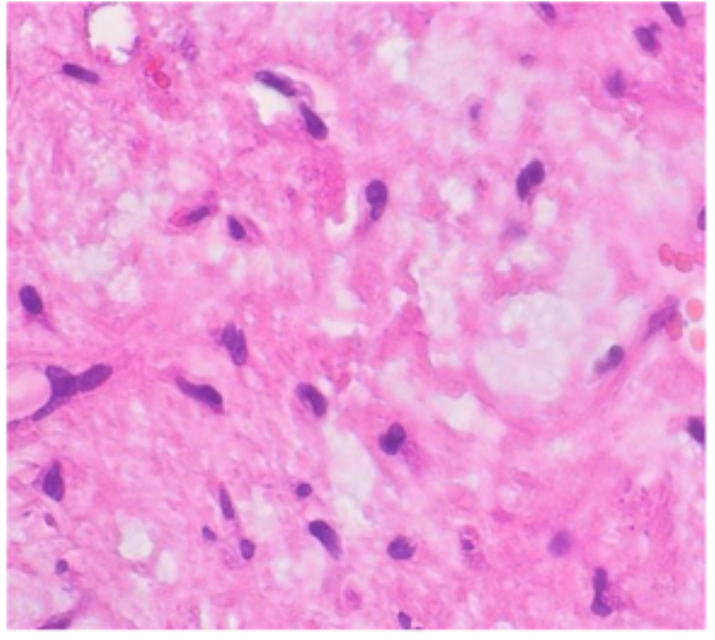
Figure 3: (In the background of loose myxomatous and gelatinous stroma, sparsely cellular).
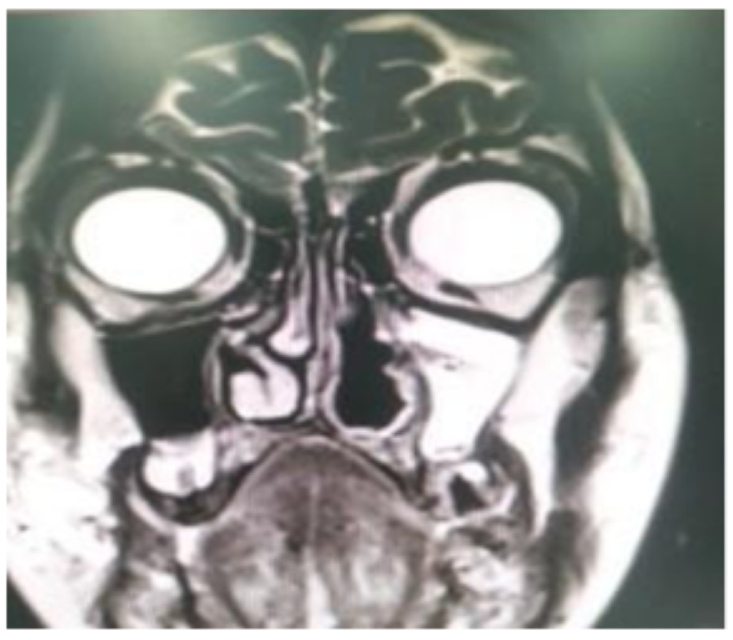
Figure 4: (MRI T2 show lobulated left maxillary nasal mass heterogenous enhancement in intermediate T2 extend to left nasal cavity and erodes the left orbital floor).
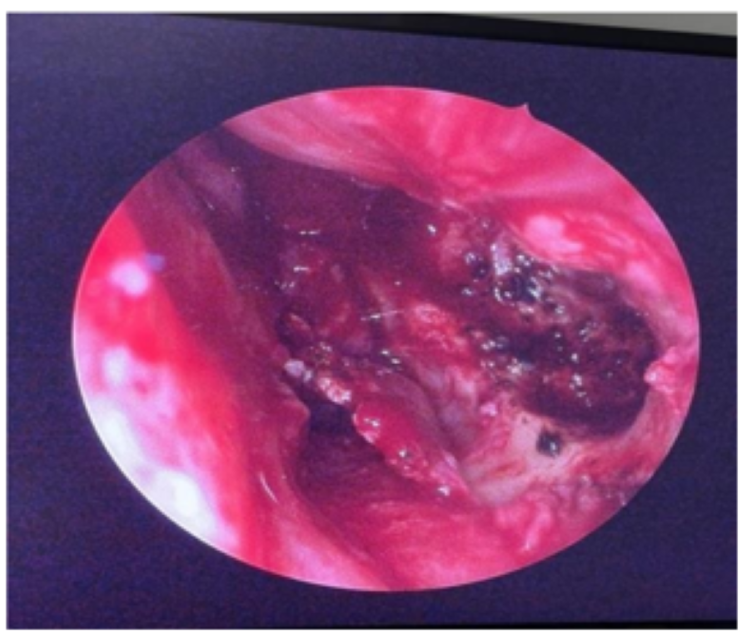
Figure 5: (modified denker procure, medial portion of anterior maxillary wall removed achieved, bone was drilled out and all mucosa extracted)
Discussion
Myxomas are neoplasms that arise from basic mesenchymal tissue and are benign. Virchow invented the term "myxoma" in 1871 to characterize tumors that resemble the mucinous appearance of the umbilical cord, myxomas were initially described as genuine mesenchymal neoplasms by Stout [4]. The heart is the most common site of involvement, but it Head and neck. can also affect bone, skin, subcutaneous tissue, and growing painless tumor that emerges late with obstructive symptoms is the most prevalent presenting symptom. roughly 0.1 percent of all head and neck tumors [5]. A slowly Rhinorrhea, epistaxis, headache, proptosis, infraorbital skeletal muscle myxomas are uncommon, accounting for paresthesia, facial deformity, visual abnormalities, CSF leak, and cranial nerve palsies are some of the other symptoms, Myxoid changes can be found in a variety of benign and malignant tumors, including sarcomas, after ruling out several benign conditions such as neurofibroma, neurilemoma, myxolipoma, myxochondroma, pleomorphic adenoma, and malignant lesions such as myxoid chondrosarcoma, myxoid liposarcoma, malignant fibrous histiocytoma, embryonal rhabdomyosarcoma etc [6]. Complete excision of the tumor with a limited quantity of normal surrounding tissue is the definitive treatment for myxoma. Their infiltrative nature and tendency for recurrence necessitate a comprehensive surgical approach. The absence of a true capsule and the potential for bioactive enzyme production, such as hyaluronic acid and acid phosphatase, contribute to the tumor's locally infiltrative character, to conduct a full surgical excision, intranasal, transantral, transseptal, transethmoidal, and numerous external approaches have all been used. With recurrence rates as high as 25%, which are usually attributed to insufficient primary excision, some authors have recommended for radical primary resection, with en bloc removal when possible [7]. FESS is a surgical method that is most typically utilized for the treatment of serious unresponsive nasal sinus diseases. Because the obstruction tissues are removed, this procedure improves symptoms in up to 90% of patients [8]. To accomplish full tumor removal, resection in these locations necessitates excellent exposure and meticulous surgical technique. Despite these drawbacks, total surgical resection offers the best chance of survival, as these tumors do not respond well to radiation or chemotherapy. We were able to properly visualize the tumor limits using endoscopy and so achieve total eradication Endoscopically, we were able to better visualize the tumor limits and, as a result, achieve total clearance.
Conclusion
FESS is an effective and preferred method of treating nasal myxoma, resulting in the full excision of the tumor. Longer follow-up should be established, to ensure that there is no long-term recurrence.
Acknowledgment:
We would like to thanks all otolaryngologist and radiologist, histopathologist and OR staff in Aseer central hospital
Funding: No Funding sources
Conflict of interest: None Declared
Ethical approval: The case report was approved by the Institutional Ethics Committee
References
- Hunchaisri N. (2002) Myxoma of the nasal cavity and paranasal sinuses: report of a case. J Med Assoc Thai. 85(1): 120-124. [PubMed.]
- Quintal M-C, Tabet J-C, Oligny L, Russo P. (1994) Oral soft tissue myxoma: report of a case and review of the literature. J Otolaryngol. 23(1): 42-45. [PubMed.]
- Daoud R, Alqarni K, Alanazi MS. (2021) Bilateral nasal myxoma in 22 years psychiatric male-a case report. Published online. [Ref.]
- Stout AP. (1948) Myxoma the tumor of primitive mesenchyme. Ann Surg. 127(4): 706-719. [PubMed.]
- Slootweg PJ, Wittkampf ARM. (1986) Myxoma of the jaws: an analysis of 15 cases. J Maxillofac Surg. 14: 46-52. [PubMed.]
- Moore BA, Wine T, Burkey BB, Amedee RG, Butcher RB. (2008) Sphenoid sinus myxoma: case report and literature review. Ochsner J. 8(4): 166-171. [Ref.]
- Perzin KH, Panyu H, Wechter S. (1982) Nonepithelial tumors of the nasal cavity, paranasal sinuses and nasopharynx. A clinicopathologic study. XII: Schwann cell tumors (neurilemoma, neurofibroma, malignant schwannoma). Cancer. 50(10): 2193- 2202. [PubMed.]
- Behiry EA, Elshazly HM, Abdel-Shafy IA, Adel Hussein H. (2019) Evaluation of quality of life after Functional Endoscopic Sinus Surgery (FESS) in chronic rhinosinusitis patients in Menoufia Governorate. Egypt J Ear, Nose, Throat Allied Sci. 20(3): 131-136. [Ref.]