>Corresponding Author : Noronha T
>Article Type : Case Report
>Volume : 2 | Issue : 7
>Received Date : 02 Nov, 2022
>Accepted Date : 14 Nov, 2022
>Published Date : 17 Nov, 2022
>DOI : https://doi.org/10.54289/JCRMH2200134
>Citation : Ettagmouti Y, Maaroufi A, Rochd M and Habbal R. (2022) Carbamazepine Induced Myocarditis in an Epileptic Adolescent: A Rare Case Report. J Case Rep Med Hist 2(7): doi https://doi.org/10.54289/JCRMH2200134
>Copyright : © 2022 Ettagmouti Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access
Physiotherapist, Primary care at ACES Oeste Norte, ARSLVT Portugal
*Corresponding author: Noronha T, Physiotherapist, Primary care at ACES Oeste Norte, ARSLVT Portugal
Abstract
The impact of environmental context and lifestyle to our health is crucial. Balancing physical activity and rest, especially sleep, is the key to healthier ageing and greater functional capacity.
Humans spend about 1/3 of their lives sleeping, usually in the recumbent position.
Favourable sleeping environment is not only a quiet place but also an adjustable sleep system may hold one of the keys to sleep right and tight.
All systems deteriorate with ageing, and the vascular system is particularly affected, which in turn aggravates the natural limitations that occur in the musculoskeletal system. In this paper we will see why sleeping system should be addressed to meet the increased impairment of the musculoskeletal system and the sleep function.
The age-related decrease in vascular function affects all body systems, and also exposes the musculoskeletal system to greater risk factors for chronic pain conditions.
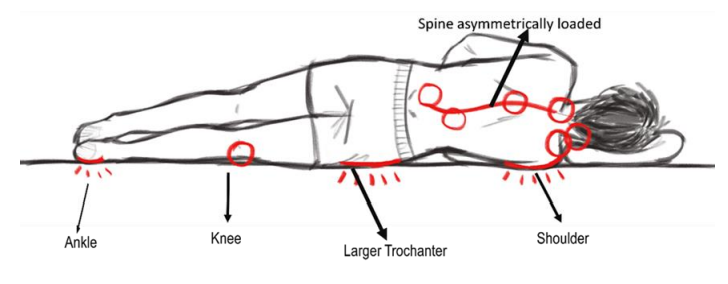
Changes occurs also in sleep architecture, the decreasing shifting of positions while asleep, the adoption of side lying and less posture options due to health conditions alone are some of the risk factors for sustained compression on all the musculoskeletal structures, particularly in the side of the body in contact with the bed. Shoulders and hips are the regions of the body that suffer greater pressure and impaired blood perfusion.
Musculoskeletal conditions and sleep disorders in the United States alone affect about 50%of the 126.6 million American adults; about 40% of those subjects who suffer from low back/neck pain, sustain pain and sleep disturbances despite analgesic treatment. Women are more susceptible to these complaints, especially those with more prominent body contours, or frail people with severe muscle atrophy.
Ageing increases the demand for a better contextual environment, not only during activity but also at rest and especially during sleep.
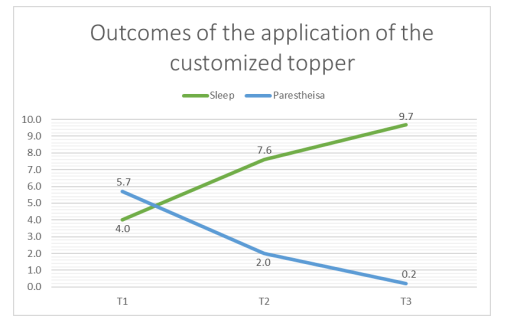
This paper based on the records of a case-series study of 19 subjects focusing only on paraesthesia and comorbid insomnia and their evolution with the systematic application of a customised topper.
Keywords: Chronic Musculoskeletal Condition; Sleep Disturbance; Contextual Approach; Postural Adjustment; Physiotherapy Management
Abbreviations: VAS: Visual Analog Scale
Background
As a physiotherapy consultant in a public health centre with over 60,000 users, my mission is to promote health by supporting everyone who comes to me for help to solve their health conditions or to find a way to reduce their burden.
In 2017, the family physicians of my health centre referred to my service 169 patients with chronic complaints of various health conditions with no positive response to pharmacological treatment, of which 138 subjects with musculoskeletal condition complaints and impairment in multiple activities of daily living.
More than 50% of the patients had multiple health conditions, presenting various limitations of daily living and multiple pain sites, in a pattern similar of which is found in the literature [1,2]. Many of these patients’ complaints of sleep disturbance and impaired walking, others have difficulty in accomplishing tasks of their job, a finding that is also referred by [3-7].
Despite a vast amount of epidemiological data on pain and sleep disturbance, the scientific community is still trying to understand the mechanism of both chronic pain and insomnia [8-13].
Since 2015, at the first contact with the patients, I have been using this image to identify the affected sites referred by the patients this practice is echoed by other researchers, such as [14-17].
The physiotherapy assessment also included:
a) Patient-Specific Functional Scale Assessment;
b) Visual Analog Scale (VAS) for Pain and Paraesthesia;
c) Postural Assessment in activity and at rest.
When appropriate, the intervention was directed at:
• Patient empowerment in the management of pain
• Home exercise program
• Postural adjustment in side lying with the application of customized topper.
All these procedures were applied during 3 direct contacts (T1; T2:T3) and was completed with electronic contact in a 12 months period.
The initial assessment (T1):
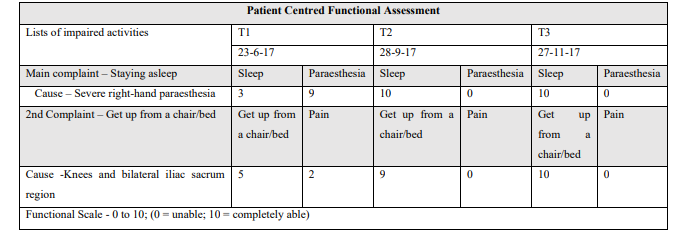
To determine the functional limitation of Sleeping and other daily activities, was applied the Patient Specific Functional Scale, ranging from 0 = unable and 10 = able as before complaints.
The pain with neuropathic characteristic was assessed by “VAS”, the Visual Analog Scale, ranging from 0 = no pain/paraesthesia; 10 = worst pain/paraesthesia ever.
Besides the assessment of pain and functional limitations, most patients were advised to avoid aggravating factors and to adopt modified gestures for their daily or occupational activities. Others were advised to get some support equipment in conjunction with the therapeutic exercise prescription.
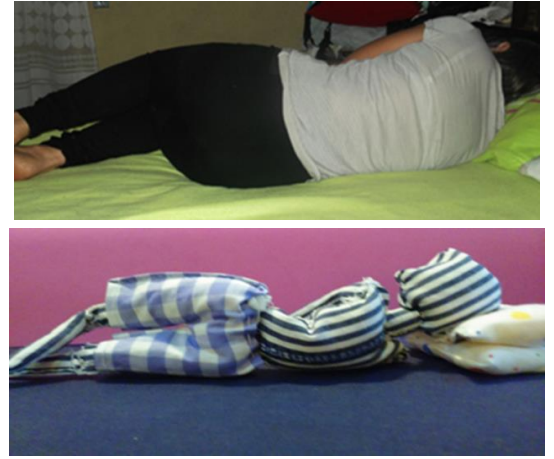
Before being able to apply the topper, the patients were first instructed to place a long fluffy pillow under the chest and up to the waist in order to create an open space for the arm to reduce some compression, and folded towels were placed under the head pillow to match the height created by the pillow placed under the chest.
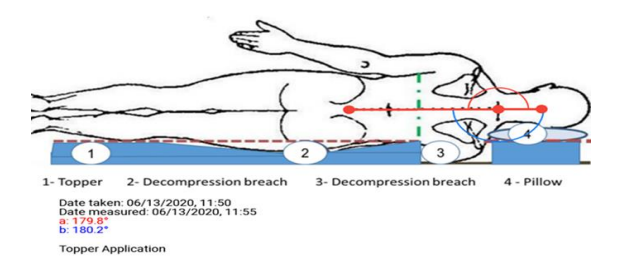
Postural assessment in the preferential sleep position on subject’s sleep system was done via image sent by email.
Patients were advised to ask someone to take their front and back images from head to toe while stay lying on their own bed and pillow at a horizontal plane in order to get the exact angle to measure any misalignment of the spine.
Second direct contact (T2):
This contact was scheduled after receiving recumbent posture images taken from the subject's sleep system to analyse the posture with the subject and to adjust more accurately and to teach how to make one's own topper according to the personal conditions.
The preferred sleeping position most adopted was side lying, which is in accordance with the findings of [18-22].
To customise the topper, it is essential to determine the points that are directly in contact with the mattress by obtaining the anthropometric parameters and evaluating the lying posture in one's usual sleeping system [23-26].
The following measures were taken:
1. The widest part of the body that is pressed onto the mattress is the deltoid region or the hip, in accordance with the contour of the body. The width measured from the most lateral surface of the right to left deltoid muscles.
2. The circumferences of the Chest, the waist and the hip.
3. The length from C7 to L5; L2 to the Iliac crest and Great Trochanter to malleolus.
There were some contacts between these direct contacts to ensure the timely monitoring and rectify some inaccurate topper application.
In 2017, the contextual approach was systematised to reduce one of the factors of pain complaint and sleep disturbance through the introduction of a customized topper.
Third direct contact (T3):
Scheduled to discharge usually 6 to 12 months after achieving maximum functionality relating to the patient's health conditions. The criteria to discharge were the highest functional level and the reduction of pain/paraesthesia.
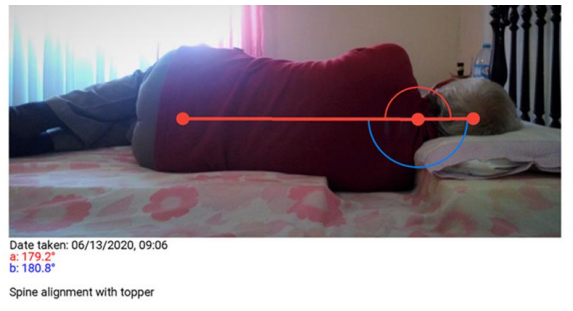
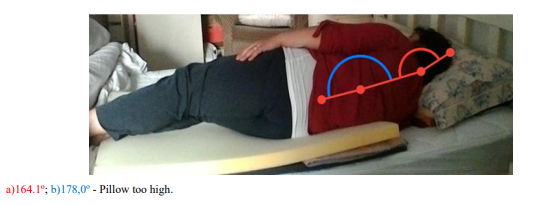
*The angle is measured with the Angulus software with the photo sent by the subject.
The sample consists of 8 men and 11 women ranging in age between 29 and 78 with a mean of 55,7 years old, all of whom presented complaints of increased paraesthesia and comorbid insomnia
*The angle is measured with the Angulus software with the photo sent by the subject.
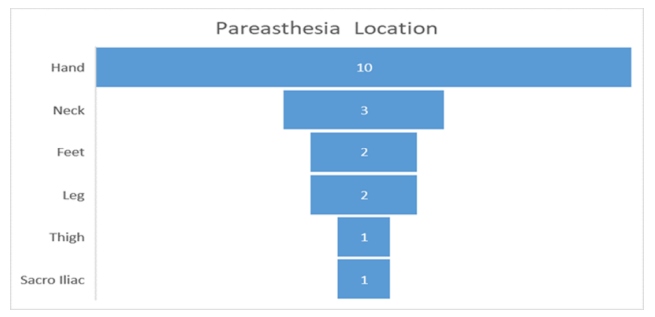
It was hypothesised that most of the paraesthesia shown in the graph may come from misalignment of the cervical spine, and thus, the rationale for the intervention was directed to the recumbent posture adjustments.
The table below presents the data collected from the subjects with exacerbation of paraesthesia in recumbent posture and the outcome following application of the customised topper.
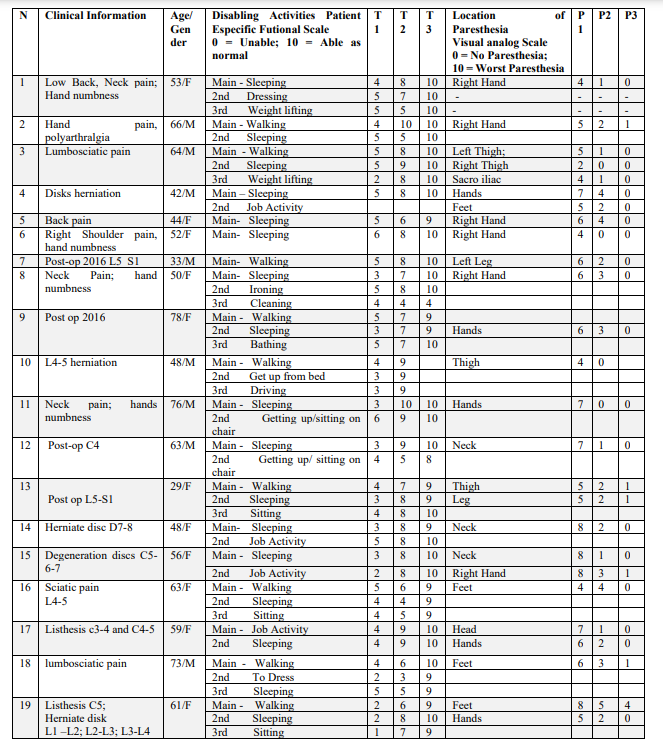
T1 - First assessment – Ability to “Stay Asleep” T2 - Assessment - Timeframe of approximately 7 to 10 days after the image of side lying taken from the subject's sleep system “Stay Asleep”. T3 - Last Assessment - Timeframe of approximately 6 to 12 months after the application of the topper Ability to “Stay Asleep”
P1- Level of paraesthesia at first contact; P2 - Level of paraesthesia following topper application; P3 - Level of paraesthesia at the last direct contact
To better illustrate this intervention, I will describe and analyse two clinical cases.
For instance, to the case number 8, a patient with an onset of 2 months and no relief from pharmacological treatment. One usual evolution of this condition, that is not responding to traditional pharmacological therapy, should be a case chronification with a tendency of widespread complaints.
Case 8 was referred by the GP on 12-april-2017.
Clinical information:
- Right shoulder pain with numbness and decreased strength in the right upper limb.
- Onset of pain and paraesthesia within 2 months and progressive aggravation despite the use of anti-inflammatory therapy.
- The cervical X-ray and EMG of the upper limb were normal.
- First contact (T1) on 5-may-2017
- Observation:
- Asymmetrical posture with inclination of the face to the right. Protraction of the head; increased physiological
- spinal curvature.
- Exacerbation of shoulder pain and paraesthesia is occurring at night while sleeping, preferential sleep posture being on the right side which, due to pain, the patient tries to sleep on the left side.
T1 - 5-may-2017 - Functional evaluation:
Main Complaint -- Functional limitation in sleeping (severe sleep disturbance) and in daily activities due to paraesthesia of right hand and pain in both shoulders, more severe on left side.
Exhaustion and decreased strength for ironing and cleaning windows.
Constant pain, level 4, increasing to level 6 with upper limb movements of flexion, abduction, adduction and internal rotation.
Mild paraesthesia of the right hand and lack of strength.
Exacerbation of shoulder pain escalating to level 8 and awake with hand paraesthesia while asleep.
The table below synthesizes the findings.
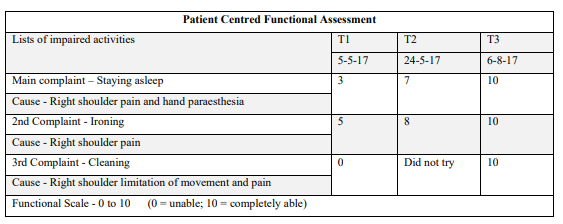
T2 - Observation- 24-May-2017
The patient reported a significant improvement both in her ability to stay asleep as well as a decrease in paraesthesia.
The custom topper application was well applied but not fully adjusted.
The height increase induced by the topper is also levelled out at the pillow height by applying the same number of layers of denser sponges placed under the pillow.
The image shows a slight deviation of the cervical spine due to the lack of adjustment of the pillow, which may be the source of complaints. Therefore, the need to evaluate it directly.
The pillow was too high causing a slight cervical misalignment. In order to refine and remove any malalignment, she was advised to bring the pillow to evaluate the need to replace or adjust it.
Maintain specific exercises to improve functional capacity.
T3- Observation 6-August-2017:
The patient had changed her pillow for one with hollow cotton fibre filling placed in a cotton pillowcase with elastane fabric with a zipper to make it easier to manage its height.
She was discharged fully functional with no pain nor paraesthesia.
She described a relapse episode due to a weekend trip to another city, and immediately experienced the same symptoms as before the application of the customize topper.
She has already perceived the cause of her complaints and has been taught the needful adjustment, if not succeed could reach me by email.
Case 11
76 years old retired male.
Clinical information:
- Bilateral gonarthrosis and heart disease.
- Overall health conditions - Cardiac condition, Sequelae of direct trauma of the knees, sleep apnea.
- Onset of Paraesthesia of right hand at night for over 6 months.
T1 - 23-jun-2017
Observation:
- Symmetrical posture with slight trunk flexion but without impairing normal gait.
- The patient has understood the strategy and sent the images the next day. He got the prescription of the topper by email, but the patient was unable to come before September.
After applying the customize topper he sent the images of his preferred lying posture on the topper.
He was advised to use a roll of hollow fibre with 40cm x 120cm, to place between the lower limbs to prevent knees compression on side lying and lessen the load of the hemi body was in contact with the mattress.
The table below synthesizes the findings
During October, the patient had travelled every weekend to assist a relative in another town. He has reported that he experienced paraesthesia of the right hand every time he was away from home and not been able to use his topper (“t-off”).
The table below presents the effect of an adjusted sleep system.
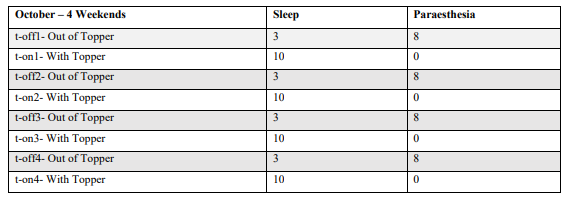
This case reinforces my view that customised topper improved the contextual conditions by removing the biomechanical stress mechanism that the musculoskeletal system was being exposed to, thus reducing comorbid insomnia due to pain or paraesthesia.
Discussion
All subjects in this sample have severe musculoskeletal complaints, with worsening neuropathic symptoms related to lying position and awakening several times during the night and no relief with pharmacological treatment. This presentation of symptoms has been already identified by several authors [27-29].
As a primary care physiotherapist my mission is to promote functional capacity and increase health literacy, as proposed by [30].
One of the skills of the physiotherapist is the postural assessment, the current practice the evaluation at work or sport activity, but the assessment in lying posture in clinical practice is not so common.
In the literature, the sleep system is commonly considered constituted by mattress and its support structure [23,31].
From my point of view, it should consist of all the elements in direct contact with the body in the recumbent position, such as pillow, mattress and toppers. All the bedding should also be included, because if the chosen fabrics are too slippery, like satin, it would interfere with the muscle relaxation during sleep.
The pillow is also a very important element of the sleeping system [32-36]. But adjusting solely the pillow may partially resolve the complaints [37], and may prevent worsening, but does not reduce paraesthesia and pain [38-40].
Therefore, as some authors [41,42], propose to ensure the necessary adjustment to prevent any deviation of the spine, the postural assessment of a person lying in their preferred position in their usual context is the key to manage this pain/paraesthesia with nocturnal exacerbation [43].
Nevertheless, in my practice, to assess the lying posture of the patients on their own sleep system was a big challenge [11].
Most of my patients are elderly with low literacy and only a few know how to use smartphone and send emails. It’s essential to adequately convince them to get their images taken lying in their own bed.
For the side lying, the spine should be like a straight line [17,18,23,31]. To trace any deviation of the body in relation to the sleep system together with the instruction to the photographer to take the image sitting in front of the bed, an image is sent as an example in order to obtain a view that allows correct analysis.

Despite of all the details given most of the images are not suitable for postural assessment in recumbent position, as shown in the picture below.

This picture only perceives subject’s knees
Almost all patients have financial difficulties and lack of support from family and friends.
To convince them to apply a customise topper, first I suggest them to use anything they have at home like duvets, pillows and towels to form the shoulder breach to decompress the affected area.
In clinical context is impossible to demand too much accuracy, and the lack of resources from the health centre and the patients requires a flexible and creative solutions in order to reduce any financial burden and get the best outcome, using any materials available at home.

When analysing the Case number 8, presented above, we can recognise that it is a recent case of musculoskeletal condition with no tangible cause and no response to analgesic or anti-inflammatory treatment.
In T1, a pain assessment was made that includes the strategy to be adopted by the patient to reduce it. This patient reported that throughout the day with the activity developed at work relieved her pain, a situation identified by several authors [18,44].
At the beginning of the complaint [45], she avoided lying on the right side, but as soon as she enters “nREM”, her body moves towards the preferred sleeping position, later awakening with paraesthesia and pain, as it is referred to occur by some authors [18,46].
But after a month, she couldn't even lie on her left side because she started to feel the shoulder pain on that side, a finding that is also described in the literature as a natural evolution of the condition when not treated [47,48,49]. Gradually, she began to feel functional limitation at work.
To make the patient understand and adhere to the intervention, she was explained the possible cause of her Paraesthesia/pain.
The intervention addressed the contextual factors and she was instructed to use a pillow placed under the trunk at the level of the 10th rib and another under the head to create the shoulder breach, for her to realize the way to reduce the pressure on the painful shoulder.
She was urged to send me the images of her lying posture to enable the assessment of lying posture in her usual context to prescribe the customized topper.
After applying this topper and changing her pillow all complaints disappeared an outcome already reported by [50].
There was only one relapse due to a two nights trip out of town without the sleeping equipment, which made the pain and neuropathic signs reappear.
The outcome of the management for case number 8 was very satisfactory both at the health condition and patient literacy.
Without removing that risk factor, the evolution of should be a natural aggravation of insomnia and multiplication of pain sites [44,49,51-54]. In fact, the disappearance of all complaints contributed to the total improvement of her functionality.
She was also advised to pay attention to the wear and tear of the material of any constituent elements of the sleep system or her anthropometric change, as it may mean the system might need readjustment, as stated by [55-57].
I discharged this patient only when I was assured that she already mastered the strategy and got my contacts if necessary.
Returning to the Case number 11, from the first direct contact (T1) the patient understood the strategy and sent the images the next day and received the indication with the measures and thicknesses of 3 foams sheets to make the customise topper. However, the T2 (second direct assessment) was only scheduled for almost 3 months after the adjustment of the sleep system. Nevertheless, analysing the image lying down with the topper applied that he sent, I advised him to use a cotton roll measuring 40cm x 120cm, to reduce knee pain by avoiding compression of the knees against each other

This patient experienced paraesthesia and pain for 4 consecutive weekends from sleeping outside his bed and the complaints disappeared as soon as he went back to the adjusted sleep system.
This fact strongly suggests that, by improving the environmental context, one could expect to reduce pain and eventually correct some postural misalignment, therefore delaying the process of musculoskeletal deterioration.
What happens to a subject who has a maladjusted sleep system, exposing himself, night after night, of sustained compression, especially on the side that is in direct contact with the mattress, and, on top of that [58-60], in conjunction with the natural deterioration of soft tissues due to aging?
During my 36 years as a physiotherapist, the following is the most heard story told by a shoulder pain sufferer:
- At the beginning, they woke up in the morning with some discomfort and stiffness on the shoulder, that would dissipate with physical activity [5,45].
- Night after night the situation deteriorated to the point that they start waking up in the middle of the night with acute shoulder pain [61-63].
- Functional limitation like taking off a T-shirt with pain when raising their arm more than 90º or taking out a wallet of the back pocket of the trousers, etc.
- They started to avoid their preferred sleeping position
sharp pain on their sleeping posture pressing the painful shoulder.
- Sometime later, they could only sleep in supine position. As the lack of comfortable sleeping position, muscle tension increased and began to feel multiplies pain sites. Neck, back and even heel pains [64-66].
Most common treatments used for these cases, [54,67-69], have not yet been able to meet the needs of these sufferers and the world health system cannot stop the increasing cases year after year, as reported by [70].
Is an overview that poor posture at work can be a risk factor for musculoskeletal injuries and how about a sustained spinal misalignment night after night?
Health professionals need to think that “Man” as an element that interacts continuously with the entire environment whether active or at rest.
Conclusion
The postural assessment of the patient's usual context in recumbent position has allowed me to discover postural deviation and sustain pressure on the most prominent areas of the body usually on the side of the preferred sleeping position.
The systematic application of a customised topper succeeds in reducing pain and paraesthesia, thus improving comorbid insomnia, and offers a feasible pathway of care for these health conditions.
These findings from my clinical practice could only be a clue to promote research with greater methodological rigor.
The possibility of developing a topper easy to customise as a resource for the management of musculoskeletal conditions with comorbid insomnia could be the answer for millions of sufferers.
References
- McBeth J, et al. (2001) Risk factors for persistent chronic widespread pain: a community-based study. Rheumatology. 95-101. [PubMed.]
- Parsons S, et al. (2007) Prevalence and comparative troublesomeness by age of musculoskeletal pain in different body locations. Farm Pract. 308-316. [PubMed.]
- World Health Organization. (2003) Special Theme -Bone and Joint Decade 2000-2010. Burden of major musculoskeletal conditions. [PubMed.]
- Sivertsen B, et al. (2015) Sleep and pain sensitivity in adults. Pain. 156(8): 1433-1439. [PubMed.]
- Axén, Iben. (2016) Pain-related Sleep Sisturbance. A Prospective Study with Repeated Measures. [autor do livro] Clin. J. Pain. Pain-related Sleep Disturbance. s.l: Wolters Kluwer Health, Inc. 32(3): 254-259. [PubMed.]
- Bone and Joint Burden Organization. (2016) The Impact of Musculoskeletal Disorders on Americans- Opportunities fo Action. Rosemont: United States Bone and Joint Initiative. [Ref.]
- Uhlig BL, Sand T, Nilsen TI, et al. (2018) Insomnia and risk of chronic musculoskeletal complaints: longitudinal data from the HUNT study, Norway. BMC Musculoskelet Disord. 19(1): 128. [PubMed.]
- Walker, Bone K, et al. (2004) The Anatomical pattern and determinats of pain in the neck and upper limbs: an epidemiologic study. Pain. 109(1-2): 45-51. [PubMed.]
- Afolalu, et al. (2017) Effects of sleep changes on pain-related health outcomes in the general population: A systematic review of longitudinal studies with exploratory meta-analysis. Sleep Medicine Reviews. 1e16. [Ref.]
- Tang, Nicole KY, et al. (2015) Impact of musculoskeletal pain on insomnia onset: a prospective cohort study. Rheumatology. 54(2): 248-256. [PubMed.]
- Asih S, et al. (2014) Insomnia in a chronic musculoskeletal pain with disability population is independent of pain and depression. Spine J. 14(9): 2000-2007. [PubMed.]
- Andersen, Monica, et al. (2013) Sleep Sisturbance and Pain. A Tale of Two Common Problems. Spine J. 2000-2007. [Ref.]
- Gran, Jan Tore. (2003) The epidemiology of chronic generalized musculoskeletal pain. Best Practice & Research Clinical Rheumatology. 17(4): 547-561. [PubMed.]
- Choy EH. (2015) The role of sleep in pain and fibromyalgia. Nat Rev Rheumatol. 11(9): 513-520. [PubMed.]
- Treede RD, et al. (2015) A classification of chronic pain for ICD-11. Pain. 156(6): 1003-1007. [Ref.]
- Elavarasi, Kumar. (2016) Definition of pain and classification of pain disorders. Journal of Advanced Clinical & Research Insights. 3: 87-90. [Ref.]
- Park SJ, Kim JS, Kim CB. (2009) Comfort evaluation and bed adjustment according to sleeping positions. Human Factors and Ergonomics in Manufacturing & Service Industries. 19: 145-157. [Ref.]
- McCabe SJ, et al. (2011) Preferred sleep position on the side is associated with carpal tunnel syndrome. Hand. 6(2): 132-137. [Ref.]
- Kempf B, Kongsted A. (2012) Association between the side of unilateral shoulder pain and preferred sleeping position: a cross-sectional study of 83 Danish patients. J Manipulative Physiol Ther. 35(5): 407-412. [PubMed.]
- Roizenblatt M, et al. (2012) Pain-related diseases and sleep disorders. Braz J Med Biol Res. 45(9): 792-798. [Ref.]
- Bettlach CLR, et al. (2019) Preferences in Sleep Position Correlate With Nighttime Paresthesias in Healthy People Without Carpal Tunnel Syndrome. 2, NY: Hand. 14(2): 163-171. [Ref.]
- Skarpsno ES, Mork PJ, Nilsen TIL, Holtermann A. (2017) Sleep positions and nocturnal body movements based on free-living accelerometer recordings: association with demographics, lifestyle, and insomnia symptoms. Nat Sci Sleep. 9: 267-275. [PubMed.]
- Verhaert V, et al. (2011) Ergonomics in bed design: the effect of spinal alignment on sleep parameters. Ergonomics. 54(2): 169-178. [PubMed.]
- Radwan A, et al. (2015) Effect of different mattress designs on promoting sleep quality, pain reduction, and spinal alignment in adults with or without back pain; systematic review of controlled trials. Sleep Health. 1(4): 257-267. [PubMed.]
- Lee WH, Ko MS. (2017) Effect of sleep posture on neck muscle activity. J Phys Ther Sci. 29(6): 1021-1024. [Ref.]
- Low FZ, et al. (2017) Effects of Mattress Material on Body Pressure Profiles in Different Sleeping Postures. J Chiropr Med. 16(1): 1-9. [Ref.]
- Gilron I, et al. (2013) Combination pharmacotherapy for management of chronic pain: from bench to bedside. Lancet Neurol. 12(11): 1084-1095. [PubMed.]
- Roizenblatt M, et al. (2012) Pain-related diseases and sleep disorders. Braz J Med Biol Res. 45(9): 792-798. [Ref.]
- Haack M, et al. (2020) Sleep deficiency and chronic pain: potential underlying mechanisms and clinical implications. Neuropsychopharmacology. 45(1): 205-216. [PubMed.]
- Slater H, Briggs AM. (2017) Models of Care for musculoskeletal pain conditions: driving change to improve outcomes. Pain Management. 7(5): 351-357. [PubMed.]
- Haex B. (2005) BACK AND BED - Ergonomic Aspects of Sleeping. Boca Raton: CRC PRESS. [Ref.]
- Ren S, et al. (2016) Effect of pillow height on the biomechanics of the head-neck complex: investigation of the cranio-cervical pressure and cervical spine alignmen. PeerJ. 4: e2397. [Ref.]
- Gordon SJ, Grimmer-Somers KA, Trott PH. (2010) Pillow use: the behavior of cervical stiffness, headache and scapular/arm pain. J Pain Res. 11(3): 137-145. [PubMed.]
- Hodkinson JB, et al. (2013) Time to stabilisation of the cervical spine when supported by a pillow in side lying. Ergonomics. 56(9): 1474-1485. [PubMed.]
- Qu N, et al. (2022) Neck Pain: Do We Know Enough About the Sensorimotor Control System? Frontiers in Computational Neuroscience. 16: 1-10. [Ref.]
- Chun-Yiu JP, Man-Ha ST, Chak-Lun AF. (2021) The effects of pillow designs on neck pain, waking symptoms, neck disability, sleep quality and spinal alignment in adults: A systematic review and meta-analysis. Clin Biomech. [PubMed.]
- Bernateck M, et al. (2008) Sustained effects of comprehensive inpatient rehabilitative treatment and sleeping neck support in patients with chronic cervico brachialgia: a prospective and randomized clinical trial. Int J Rehabil Res. 31(4): 342-346. [PubMed.]
- Lähdeoja T, Karjalainen T, Jokihaara J, et al. (2020) Subacromial decompression surgery for adults with shoulder pain: a systematic review with meta-analysis. British Journal of Sports Medicine. 54(11): 665-673. [PubMed.]
- Roth Bettlach CL, et al. (2019) Preferences in Sleep Position Correlate With Nighttime Paresthesias in Healthy People Without Carpal Tunnel Syndrome. Hand. 14(2): 163-171. [PubMed.]
- McCabe SJ, Xue Y. (2010) Evaluation of sleep position as a potential cause of carpal tunnel syndrome: preferred sleep position on the side is associated with age and gende. Hand. 5(4): 361-363. [Ref.]
- Wong DW, et al. (2019) Sleeping mattress determinants and evaluation: a biomechanical review and critique. PeerJ. 25(7). [Ref.]
- Radwan A, et al. (2015) Effect of different mattress designs on promoting sleep quality, pain reduction, and spinal alignment in adults with or without back pain; systematic review of controlled trials. Sleep Health. National Sleep Foundation. 1(4):257-267. [PubMed.]
- Millar NL, et al. (2012) Hypoxia: a critical regulator of early human tendinopathy. Ann Rheum Dis. 71(2): 302-310. [PubMed.]
- Aili K, et al. (2015) Sleep disturbances predict future sickness absence among individuals with lower back or neck-shoulder pain: a 5-year prospective study. Scand J Public Health. 43(3): 315-323. [PubMed.]
- Korthuis RJ. (2011) Skeletal Muscle Circulation in Disease States and Aging: Protective Effects of Exercise. [autor do livro] Korthuis. Skeletal Muscle Circulation. San Rafael: Morgan & Claypool Life Sciences. [Ref.]
- Cary D, Jacques A, Briffa K. (2021) Examining relationships between sleep posture, waking spinal symptoms and quality of sleep: A cross sectional study. PLOS ONE. Matias Noll, Instituto Federal Goiano. 1-13. [Ref.]
- Smith MT, et al. (2007) The effects of sleep deprivation on pain inhibition and spontaneous pain in women. Sleep. 30(4): 494-505. [PubMed.]
- Mork PJ, Nilsen TI. (2012) Sleep problems and risk of fibromyalgia: longitudinal data on an adult female population in Norway. Arthritis Rheum. 64(1): 281-284. [PubMed.]
- Carnes D, et al. (2007) Chronic musculoskeletal pain rarely presents in a single body site: results from a UK population study. Rheumatology. 46(7): 1168-1170. [PubMed.]
- Persson L, et al. (2009) Neck pain and pillows - A blinded study of the effect of pillows on non-specific neck pain, headache and sleep. Advances in Physiotherapy. 3(8): 122-127. [Ref.]
- Ross J, et al. (2016) Muscle IL1β Drives Ischemic Myalgia via ASIC3-Mediated Sensory Neuron Sensitization. Journal of Neuroscience. 26(36): 4582-4515. [Ref.]
- Inoue S, et al. (2017) The prevalence and impact of chronic neuropathic pain on daily and social life: A nationwide study in a Japanese population. Eur J Pain. 4(21): 727-737. [PubMed.]
- Holdaway LA, et al. (2018) Is sleep position associated with glenohumeral shoulder pain and rotator cuff tendinopathy: a cross-sectional study. BMC Musculoskelet Disord. 1: 19. [PubMed.]
- Kovacs FM, et al. (2015) Patients with neck pain are less likely to improve if they experience poor sleep quality: a prospective study in routine practice. Clin J Pain. 8(31): 713-721. [PubMed.]
- Denninger M, Martel F, Rancourt D. (2011) A single step process to design a custom mattress that relieves trunk shear forces. Int J Mech Mater. 7: 1-16. [Ref.]
- Haex B, Sloten JV, Audekercke RV. (1996) "Required stiffness distribution in a mattress for an optimal curvature of the human spine during bedrest." Amsterdam, Netherlands: Proceedings of 18th Annual International Conference of the IEEE Engineering in Medicine and Biology Society. [Ref.]
- Sadek I, et al. (2017) Novel Unobtrusive Approach for Sleep Monitoring Using Fiber Optics in an Ambient Assisted Living Platform. Paris: Springer Nature. [Ref.]
- Mulligan EP, et al. (2015) Sleep quality and nocturnal pain in patients with shoulder disorders. J Shoulder Elbow Surg. 24(9): 1452-1457. [PubMed.]
- Kempf B, Kongsted A. (2012) Association between the side of unilateral shoulder pain and preferred sleeping position: a cross-sectional study of 83 Danish patients. J Manipulative Physiol Ther. 5(35): 407-412. [PubMed.]
- De Koninck J, Lorrain D, Gagnon P. (1992) Sleep positions and position shifts in five age groups: an ontogenetic picture. Sleep. 2(15): 143-149. [PubMed.]
- Gordon SJ, Trott P, Grimmer KA. (2002) Waking cervical pain and stiffness, headache, scapular or arm pain: gender and age effects. Aust J Physiother. 1(48): 9-15. [PubMed.]
- Smith MT, Haythornthwaite JA. (2004) How do sleep disturbance and chronic pain inter-relate? Insights from the longitudinal and cognitive-behavioral clinical trials literature. Sleep Med Rev. 2(8): 119-132. [PubMed.]
- Yarznbowicz R. (2020) A prospective study of patients with shoulder pain and Mechanical Diagnosis and Therapy. J Man Manip Ther. 1(28): 41-48. [PubMed.]
- Scudds RJ, Robertson JM. (2000) Pain factors associated with physical disability in a sample of community-dwelling senior citizens. J Gerontol A Biol Sci Med Sci. 7(55): 393-399. [PubMed.]
- Vogt MT, et al. (2003) Aging and Body Composition Study. Neck and shoulder pain in 70- to 79-year-old men and women: findings from the Health, Aging and Body Composition Study. Spine J. 6(3): 435-441. [PubMed.]
- Fischbein R, et al. (2015) The assessment and treatment of back and neck pain: an initial investigation in a primary care practice-based research network. Prim Health Care Res Dev. 5(16): 461-469. [PubMed.]
- Lang E, et al. (2002) Interventions for improvement of primary care in patients with low back pain: how effective are advice to primary care physicians on therapies and a multimodal therapy program arising out of cooperation of outpatient health care structures? Schmerz. 1(16): 22-33. [PubMed.]
- Pribicevic, Mario. (2012) The Epidemiology of Shoulder Pain: A Narrative Review of the Literature. Pain in Perspective. s.l. IntechOpen. [Ref.]
- Lewis J, O’Sullivan P. (2018) Is it time to reframe how we care for people with non-traumatic musculoskeletal pain? British Journal of Sports Medicine. 52: 1543-1544. [PubMed.]
- World Health Organization. (2022) Musculoskeletal health. s.l. WHO. [Ref.]