>Corresponding Author : Houssein Darwish
>Article Type : Case Report
>Volume : 3 | Issue : 2
>Received Date : 03 Feb, 2023
>Accepted Date : 16 Feb, 2023
>Published Date : 22 Feb, 2023
>DOI : https://doi.org/10.54289/JCRMH2300107
>Citation : Kawatharani S, Darwish H, Rahme R, Baajour J and Bsat S. (2023) Importance of Instant Thrombectomy to Treat Cerebral Vessel Occlusion During TAVI in Third World Country. J Case Rep Med Hist 3(2): doi https://doi.org/10.54289/JCRMH2300107
>Copyright : © Kawatharani S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access | Full Text
1Neurosurgery American University of Beirut Medical Center
2Assistant Professor of Neurosurgery, American University of Beirut Medical Center
3American University of Beirut Medical Center
*Corresponding author: Houssein Darwish, Assistant Professor of Neurosurgery, American University of Beirut Medical Center
#First author: Sarah Kawatharani, Neurosurgery American University of Beirut Medical Center
Abstract
Background: Transcatheter aortic valve implantation (TAVI) is considered to be one of the treatments for symptomatic severe aortic stenosis. This procedure has been associated with cerebrovascular events be it thromboembolic or hemorrhagic in nature that increase the periprocedural mortality and morbidity. Strokes post TAVI are mostly ischemic in origin; they can be either due to symptomatic or silent emboli. These thromboembolic events may occur during the procedure or up to 2 months after the procedure. In the acute setting, especially during the procedure, immediate intervention is crucial for better patient outcome. Mechanical thrombectomy is the best treatment modality for immediate revascularization and stroke prevention.
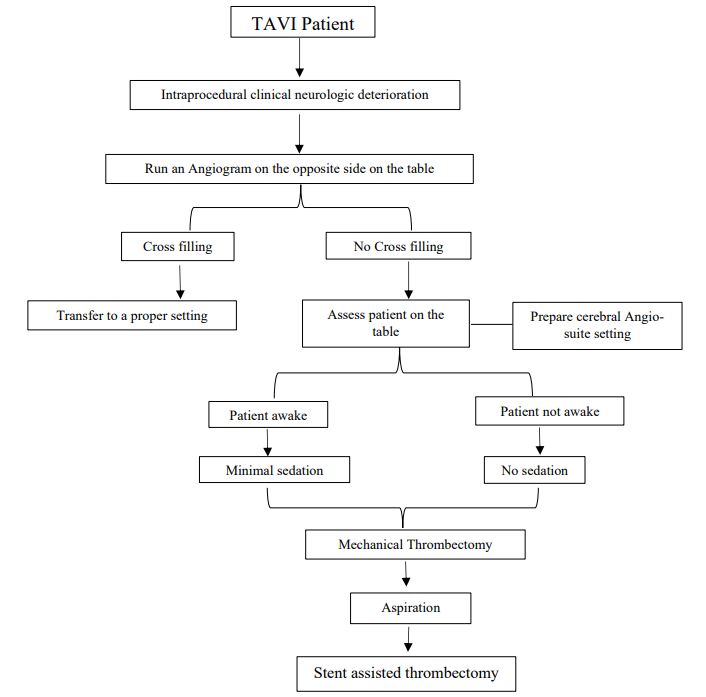
Case description: We present a case of a patient who developed symptomatic signs of hypoperfusion during the procedure that required an urgent mechanical thrombectomy in a third world country. The patient didn’t undergo CT imaging and wasn’t transferred to the brain angiography suite; the procedure was done using the x-ray machine and in the cardiology catherization lab which lacks proper equipment to do cerebral DSA (Digital subtraction angiography). This case is the 8th to be reported in the literature where mechanical thrombectomy was done on the table during a TAVI procedure. Based on this case and the literature review, we will propose an algorithm for dealing with similar cases.
Conclusion: We highlight the importance of instant thrombectomy that should be done in a patient suffering from a thromboembolic event while performing TAVI procedure. Using the same endovascular access, in the same setting in the cardiac catherization lab to assess thrombus location, even if done sub-optimally without DSA, in correlation with patient’s symptoms, without taking the patient to perform a CT scan, is life saving and guarantees quick reperfusion after clot aspiration with clinical improvement afterwards and better patient outcome.
Abbreviations: TAVI: Transcatheter Aortic Valve Implantation, DSA: Digital Subtraction Angiography, AS: Aortic Stenosis, AKI: Acute Kidney Injury
Introduction
AS (Aortic stenosis) is a valvular disease that increases in prevalence with aging whereby an intervention is usually needed. Up to 1/3rd of elderly patients are not candidates for surgery thus requiring less invasive interventions such as TAVI [1]. This procedure involves the insertion of a prosthetic valve into the stenotic vessel endovascularly, and thus avoiding the need for surgery. Despite the reduced operative risks, TAVI poses its own risks which include, but are not limited to, atrioventricular conduction system injuries, AKI (acute kidney injury), aortic regurgitation and cerebrovascular injuries. In fact, vascular injuries account for the majority of complications post-TAVI and can range from dissection and perforation to acute thrombotic occlusion [2]. Manipulation of a calcified aortic valve be it with catheters, balloon valvuloplasty or via stent valve engenders embolic material which can lodge and block arteries resulting in a stroke [1].
In the past years, the clinical incidence of peri-procedural stroke during TAVI remains to be around 2.3% [3]. There are several factors that can predict the risks of cerebrovascular events during TAVI which can be further subclassified into procedural and patient related. Procedural factors include aortic atheroma, smaller aortic valve area, valve embolization and learning curve [4].Patient related factors include prior atrial fibrillation, prior stroke, chronic kidney disease, peripheral vascular disease and aortic regurgitation [2].To our knowledge, 7 cases have been reported in the literature where the patient developed a thromboembolic event that required immediate intervention on the table in the catheterization lab; Our case is the 8th case where we had to intervene immediately through mechanical thrombectomy [5].
Case presentation
We present a case of an 88-year-old gentleman not known to have any documented comorbidities who was diagnosed with severe aortic stenosis to which he was planned for TAVI. During the procedure patient experienced left sided weakness during balloon inflation and had decreased level of consciousness, left sided weakness, and aphasia.
We were called urgently to the catheterization lab, and using the same access, in the same setting without doing a CT scan, we started with a left carotid run to check for the status of the cerebral perfusion and circle of Willis. This was done to assess whether or not we have time to transfer the patient to the cerebral angiography suite. But the fact that there was no cross filling (Figure 1) made us attempt mechanical thrombectomy on the table instantly under suboptimal conditions. We then did a right common carotid artery run and found total occlusion of the proximal internal carotid artery (Figure 2). Using Sophia 6F we did the first aspiration using a 20-cc syringe with continuous negative pressure for 2 minutes at the proximal internal carotid artery. Following the first attempt, there was opening of the internal carotid artery all the way to the intracranial bifurcation and thus we were left with a T occlusion. We then introduced a 7F guiding catheter and using Sophia 6F, three attempts of aspiration were performed until we had total reperfusion in both the anterior cerebral artery and middle cerebral artery (Figure 3). A picture of the aspirated clot is displayed in (Figure 4).
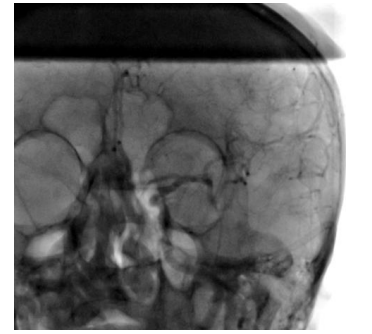
Figure 1. Left carotid run to check for cross filling which was not present in this patient
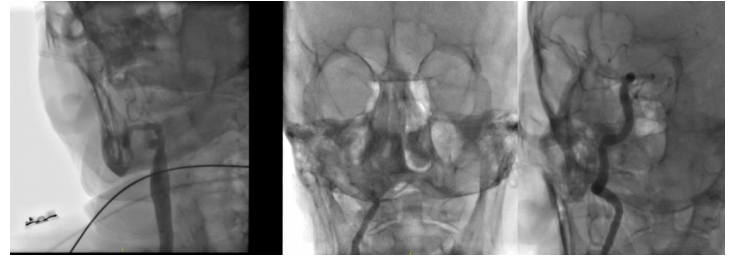
Figure 2. The first right carotid run showing total proximal occlusion
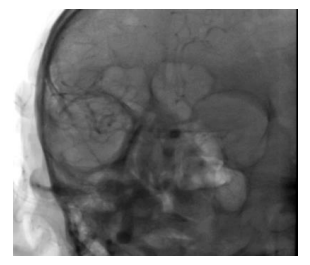
Figure 3. After the third attempt of aspiration at the ICA bifurcation

Figure 4. Thrombus after aspiration
The patient did extremely well right after reperfusion was established and returned to his baseline. He became fully alert, verbalized and his left sided weakness started to subside. The whole procedure took 45 minutes. CT and MRI done post thrombectomy did not show any infarcts.
Discussion
Transcatheter aortic valve implantation (TAVI) has been considered one of the treatments for severe aortic stenosis whereby cerebrovascular events remain one of the most feared complications with increased mortality and morbidity on patients [2]. It is worth noting that most acute strokes are ischemic in origin with <5% reported as hemorrhagic stroke [6]. Patients can experience clinical as well as silent cerebral embolisms in both the acute and later stages [2]. Incidence of cerebrovascular events varied among centers and studies but ranges from 1-11% [7]. Studies that categorized stroke severity into disabling stroke and non-disabling, reported higher incidence of the former 58% compared to the later 26% [6]. While the intraprocedural incidence is around 19 %, studies have shown that the incidence of stroke is highest in the first 24-48 hours after the procedure covering up to 40% of the cases [3]. Patients remain susceptible for up to 2 months after TAVI after which the risk decreases and stabilizes over time [1].
In this particular case we had to intervene immediately on the table in the cardiac angiography suite. The patient was under local anesthesia with no sedation given, and the angiography machine lacked a program for DSA. The cerebral angiography suite in our hospital is on a different floor and due to the clinical status of the patient, his acute sudden deterioration and the absence of a complete circle of Willis with the cross-filling perfusion from the other carotid, we opted to intervene on spot without further delays.
The whole procedure took 45 minutes, and the patient returned to his baseline post procedure with total perfusion of his right hemisphere without any clinical or radiological signs of infarcts. The major challenges in this case were that the patient was continuously moving with minimal sedation, with no proper vision and highly tortuous vessels. In the perfect setting, the angiography suite would be equipped to perform digital subtraction angiography (DSA). These two factors make a huge difference in identifying the proper road map so that we can navigate to the area of the thrombus to perform a proper thrombectomy. In our case, no sedation was given to this patient because of his rapid clinical deterioration. Moreover, we could not do a CT scan especially that the patient was fully anti-coagulated and we weren’t sure if he bled or not. Based on all what we’ve presented, we will introduce an algorithm for dealing with such cases in a third world country in a place where we lack a perfect setting (Figure 5).
Conclusion
We highlight the importance of instant thrombectomy that should be done in a patient suffering from a thromboembolic event while performing TAVI procedure. Using the same endovascular access, in the same setting in the cardiac catherization lab to assess thrombus location, even if done sub-optimally without DSA, in correlation with patient’s symptoms, without even taking the patient to perform a CT scan, is life saving and guarantees quick reperfusion after clot aspiration with clinical improvement afterwards.
References
- Alsara O, Alsarah A, Laird-Fick H. (2014) Advanced age and the clinical outcomes of transcatheter aortic valve implantation. J Geriatr Cardiol. 11(2): 163-170. [PubMed.]
- Armijo G, Nombela-Franco L, Tirado-Conte G. (2018) Cerebrovascular Events After Transcatheter Aortic Valve Implantation. Front Cardiovasc Med. 5: 104. [PubMed.]
- Linder M, Higgen FL, Voigtländer L, Weimann J, Ludwig S, et al. (2022) Stroke events after transcatheter aortic valve implantation: Temporal relationships and affected brain regions. Am Heart J. 247: 112-122. [PubMed.]
- Vlastra W, Jimenez-Quevedo P, Tchétché D, Chandrasekhar J, de Brito FS Jr, et al. (2019) Predictors, Incidence, and Outcomes of Patients Undergoing Transfemoral Transcatheter Aortic Valve Implantation Complicated by Stroke. Circ Cardiovasc Interv. 12(3): e007546. [PubMed.]
- Pyra K, Szmygin M, Olszewski K, Tarkowski P, Sojka M, et al. (2020) Mechanical thrombectomy for intra-procedural ischemic stroke during transcatheter aortic valve implantation. Postepy Kardiol Interwencyjnej. 16(4): 519-520. [Ref.]
- Franco JI, et al. (2018) Central neurocytoma: Cytological features and histological confirmation of an uncommon neoplasm. Cytopathology. 29: 126. [Ref.]
- Auffret V, Regueiro A, Trigo MD, Altisent OAJ, Campelo-Parada F, et al. (2016) Predictors of Early Cerebrovascular Events in Patients With Aortic Stenosis Undergoing Transcatheter Aortic Valve Replacement. J Am Coll Cardiol. 68(7): 673-684. [PubMed.]