>Corresponding Author : Kurt Widhalm
>Article Type : Case Report
>Volume : 3 | Issue : 4
>Received Date : 30 May, 2023
>Accepted Date : 12 June, 2023
>Published Date : 16 June, 2023
>DOI : https://doi.org/10.54289/JCRMH2300118
>Citation : Gopinath SK. (2023) Utility of VATS in Thoracic Trauma: When? Why? and How? J Case Rep Med Hist 3(4): doi https://doi.org/10.54289/JCRMH2300118
>Copyright : © 2023 Gopinath SK. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access
Sir Ganga Ram Hospital, New Delhi, India
*Corresponding author: Srinivas Kodaganur Gopinath, Sir Ganga Ram Hospital, New Delhi, India
Abstract
Background: Thoracoscopy/VATS is an under utilized modality in thoracic trauma. In this article we aim to review the utility of thoracoscopy in chest trauma patients. We have also illustrated a case from our hospital, to demonstrate the effective use of VATS in trauma.
Main Body: Indications for VATS in trauma can be divided into emergency, early and late, based on the timing of the intervention. In emergency situations, if the patient is hemodynamically stable, VATS can be used to control bleeding from the chest wall and intercostal vessels, it can also be useful for evacuation of clots, removal of foreign bodies, diagnosing diaphragmatic injuries and to visualize other internal organs of the thoracic cavity. In a delayed setting it can be used for evaluation and control of persistent pneumothorax, repair of lung lacerations and diaphragmatic injuries and also for fixing rib fractures. Uniportal VATS is a new technology that is coming up quickly, but is yet to be proven superior to traditional 3 port VATS in chest trauma.
Conclusion: VATS is an important tool in the armamentarium of surgeons involved in dealing with chest trauma. However, it is not a substitute for emergency thoracotomy, but can only be a supplement to it.
Keywords: Thoracic Trauma; Stab Injury; VATS; India; Chest Injury; Penetrating Injury; Knife in Situ; Lung Laceration
Abbreviations: VATS: Video Assisted Thoracic Surgery, STS: Society of Thoracic Surgeons, CT: Computed Tomography, USG: Ultrasonography, FAST: Focused Assessment with Sonography in Trauma, OT: Operating theatre
Background
Thoracic trauma is a major cause of morbidity and mortality all over the world [1]. Effective management of chest trauma involves basic resuscitation and a simple tube thoracostomy in more than 90% of the cases [2].
VATS (Video Assisted Thoracic Surgery) as a therapeutic modality in management of trauma is becoming popular in recent years. However, due to various factors, it has not become widespread and routine. The use of VATS in evacuation of retained hemothorax is well established [3]. However, its role in penetrating injuries of the chest is still debated [1,4].
Thoracoscopy/VATS is an effective tool, when applied in the appropriate setting. As of today, thoracoscopy remains underutilized in all aspects of thoracic surgery. It has been more than 30 years since the first VATS lobectomy was performed in the United States [5] and still, as per recent data from the STS (society of thoracic surgeons) database, only around 30% of the lobectomies performed in the United States are done by VATS [6]. We can safely assume, that in Asia, the numbers are far lower.
Main Body
Thoracoscopy in the setting of trauma, was first reported in 1976 by Jackson and Ferreira [7]. they describe the use of thoracoscopy to rule out diaphragmatic injuries.
In 1981, an interesting paper illustrated the concept of an “emergency thoracoscopy”, Jones and colleagues [4] describe a series of patients, who underwent thoracoscopy under local anesthesia. They were able to avoid thoracotomy in 44% of the cases. As we see in the earlier days of thoracoscopy, it was mainly used for diagnostic purposes.
The role of thoracoscopy in trauma has evolved over the decades, as the technique became refined, and surgeons became more confident with VATS. VATS started being used for evacuating retained hemothoraces [3]. Evacuation of blood clots was a technically simple procedure and it avoided a thoracotomy in trauma patients, who were already suffering from multiple rib fractures and soft tissue injuries to the chest wall, thereby improving outcomes [8,9]. As techniques evolved, VATS was used to deal with more complex problems such as control of intercostal vessel bleeding, removal of foreign bodies, evaluation of persistent pneumothorax and also dealing with sequelae of trauma such as empyema [9].
Indications
Ahmed et al [9], have proposed an unique classification, that can help surgeons decide on the application of VATS in trauma. According to their paper, chest trauma can be broadly divided into four categories
i) Fatal injuries- cardiac injuries, aortic injuries which result in death immediately or requires an emergency room thoracotomy- no role for VATS
ii) Potentially fatal injuries- requiring initial resuscitation and then a thoracotomy for on going hemorrhage from chest wall, lung, and diaphragm. Tracheo-bronchial and esophageal injuries are included in this category- Diagnostic VATS is useful and possibly therapeutic in minor bleeding.
iii) Non fatal injuries- comprise 80-85% cases, require tube thoracostomy and medical management, no role of VATS in emergency settings
iv) Delayed Complications- Retained hemothorax, empyema, diaphragmatic hernia and loculated pneumothorax- VATS is extremely useful and specific indications will be discussed further.
Milanchi et al [10] have given a clinically useful classification regarding the indications for VATS in chest trauma patients (Table 1). This classification is based on the timing of application of VATS and can be a very useful guide to the cardiothoracic surgeon planning to use VATS for trauma patients.
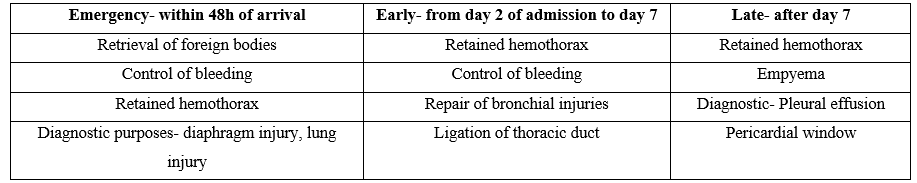
Table 1:Indications for VATS in trauma classified on the basis of timing of intervention-(from S Milanci et al [10])
Specific Indications
1) To rule out diaphragmatic injuries-
Diaphragmatic injuries are missed in 10-30% cases of penetrating thoraco-abdominal injuries [11]. Physical exam, Chest X-ray, diagnostic peritoneal lavage and a focused abdominal sonogram (FAST) alone or in combination can still miss diaphragmatic injuries in upto 30% of the cases [11].
Left side diaphragmatic injuries are more likely to be missed as on the right side the diaphragm is more closely applied to the liver and any diaphragmatic injury is associated with concomitant liver injury leading to a hemoperitoneum or a hemothorax, which is usually picked up by any imaging modality [9]. Secondly, a missed right diaphragmatic injury can heal by secondary intention without having much consequences, where as on the left side, the chances of hollow organ herniation into the chest is higher [11].
Hence, in all stab injuries, gun shots of the left lower chest and abdomen, upto 59% are associated with diaphragmatic injuries [12].
Thoracoscopy offers an excellent modality to visualize the diaphragm, the entire hemidiaphragm can be visualized with more ease than laparoscopy [9]. Laparoscopy is also a good option in these settings, however laparoscopy has certain disadvantages i.e a tension pneumothorax can develop if there is a defect in the diaphragm and a pneumoperitoneum is created during laparoscopy [13].
Not only is thoracoscopy diagnostic, for small tears, it can be therapeutic and primary repair of the diaphragm can be done thoracoscopically [14].
2) Residual hemothorax- this is the most common indication for VATS in trauma [3]. 18-30% of patients who have had a significant hemothorax post chest trauma end up with this complication and require some sort of intervention [15]. The options available are a second chest tube, VATS evacuation or a thoracotomy.
Small quantities of hemothorax resorb over time, Larger quantities are problematic resulting in empyema, pleural thickening and fibrothorax. VATS has been found clinically useful in patients with greater than 500 cm3 of clotted blood, this roughly corresponds to one-third of the hemithorax on a standard CT scan [15].
VATS when compared to thoracotomy or a second chest tube has been associated with better post operative outcomes, in terms of decreased length of stay and overall decreased hospital costs [3]. It has also been shown that 10-15% of patients treated with a second chest tube eventually required thoracotomy or VATS for evacuation of the clots.
During evacuation by VATS, a high pressure suction irrigation system has been found to be very useful [9]. In the authors’ institution a Yankeur sucker and a ring forceps are good enough for the job. Complete lung expansion should be ensured before closure, this might require a formal decortication in some cases.
In recent years, surgeons have become more aggressive and are pushing for Early evacuation of retained hemothoraces by VATS [16,17]. Most authors recommend evacuation by day 3 of trauma and maximum by day 6 [16-18].
Pin-Chou et al have shown in their prospective comparative study that repair of lung lacerations during evacuation of hematoma results in better outcomes. Fixation of rib fractures at the time of hematoma evacuation has also been shown to be beneficial [19].
3) Persistent Pneumothorax- Traumatic pneumothorax is the most common sequelae of parenchymal lung injury [9]. Majority of these pneumothoraces resolve within 72h after a tube thoracostomy [20]. However, there are certain set of patients, whose air leak does not resolve with a chest tube and persist beyond 72h. Some authors also recommend usage of a closed suction, and have reported earlier resolution of pneumothoraces [20]. Inspite of using a closed suction, air leak can persist and lung expansion may not have been achieved. In such cases, the first step is to do a bronchoscopy to rule out any major airway injury. If there is no major airway injury and the air leak is localized to the lung parenchyma, VATS seems to be a good option [9]. VATS results in resolution of air leak and complete lung expansion. The points of air leak can be identified and the involved part of the lung parenchyma can be stapled off.
4) Post traumatic empyema- Trauma is one of the common causes for development of empyema [9]. Upto 25% of chest trauma patients can develop empyema [21]. Most of these patients have had a chest tube placed for hemothorax. In the setting of a retained hemothorax, where multiple chest tubes have been placed, these tubes may act as pathways of spread of infections and result in empyema formation. The most common causative organism in a large series of trauma patients, was Staph. Aureus [22], indicating the possibility of this organism travelling via the chest tube. Early evacuation of retained clots from the chest, can prevent empyema from developing. VATS has been shown to be effective in treating empyema [9,23]. It is now the standard treatment in early empyemas [9] and in expert hands can also be used in advanced empyemas [23].
5) Other uses- VATS can also be effectively employed to treat non hemodynamically significant hemorrhage [9]. Bleeding arising from the intercostal arteries can be easily tackled by VATS, this leads to early removal of chest tube, prevents clot formation and retained hemothoraces. Extraction of foreign bodies, bullets, weapons can be done by VATS. There are also reports of Rib Fixation being done by VATS with specialized equipment [24].
6) Role of VATS in penetrating chest trauma: As mentioned earlier, thoracoscopy is useful for diagnosing diaphragmatic injuries after penetrating trauma. The largest series of 123 cases by Jin et al [25] from China, have demonstrated that effective utilization of VATS can avoid thoracotomy in penetrating chest trauma. We would also like to share a case report from our unit to demonstrate the effective use of VATS in penetrating chest trauma.
A 26 year old gentleman, presented to the casualty with history of stab injury to the back of the left chest. The incident took place in a nearby market area, there was no history of loss of consciousness, seizures or any bleed from the mouth, nose or ears. He was immediately brought to our casualty by the bystanders. On arrival to the Casualty, he was evaluated and managed according to the ATLS (Advanced Trauma and Life Support) guidelines issued by the American College of Surgeons. He was found to be conscious, oriented and was able to speak clearly. He was noted to have tachycardia with a heart rate of 120/min. His blood pressure was 110/70 mm of Hg and Respiratory rate of 18/min. He was complaining of pain in the left side of the chest.
On examination a knife was seen protruding from the wound in the posterior aspect of the left chest in the infrascapular area (Fig.1). A part of the weapon was inside the chest wall, therefore no attempt was made to extract the weapon in the casualty.

Figure 1Photograph of patient in casualty with knife in-situ
Secondary survey involving detailed examination of other systems were carried out. On examination of the chest, there were no signs of mediastinal shift, hemothorax or pneumothorax. Rest of the organ systems were normal. All peripheral pulses were normally felt.Under the supervision of a Thoracic Surgery Resident, he was carefully shifted to the Operating theatre (OT). The resident ensured that the weapon did not accidently get displaced during transport.Plan was made to explore the left hemithorax by thoracoscopy and proceed further.
Surgical details
Anesthesia: As patient could not be turned supine, due to the impaled weapon, our senior anesthetist was called in. A Double lumen tube (left sided) was inserted under bronchoscopy guidance in the lateral position and patient was put under general anesthesia.
Positioning: Right Lateral decubitus position with mild extension at the lower chest to open up the rib spaces.
Using C- Arm Fluroscopy an X- ray was taken before incision, which showed the tip of the knife well within the thoracic cavity (Fig 2).
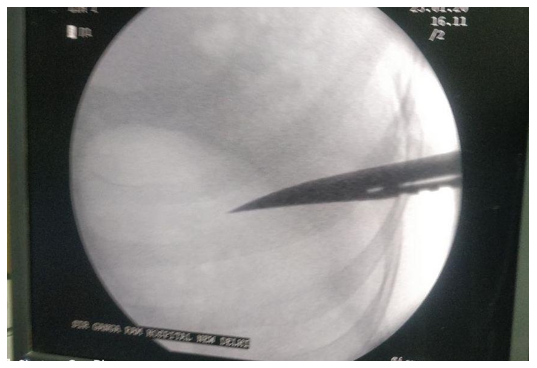
Figure 2: Fluoroscopic image taken in OT after induction
A 10 mm 30 degree scope was inserted in the 4th intercostal space and diagnostic thoracoscopy was performed after ensuring collapse of the left lung. Around 500 ml of frank blood was seen in the left chest, the tip of the knife was just seen protruding through the chest wall. A 2 x2 cm laceration was seen in the lateral surface of the lower lobe, there seemed to be no active bleeding from the lung laceration. Descending thoracic aorta, lung hilum, pericardium and diaphragm appeared normal.
Now, from the outside, the entry wound was extended on both sides till the chest wall, the intercostal space was further enlarged and the weapon was extracted under vision.
All the blood was evacuated (Fig 3), lung laceration was sutured with non absorbable fine suture (prolene 3-0) (Fig 4). Air leak test was done and no leak was seen from the laceration. Thoracic cavity was thoroughly washed, single chest tube (28 Fr) was inserted and all the wounds were closed primarily after saline irrigation.
Patient was extubated and shifted to recovery room. He was shifted to the ward on day 1 and chest tube was removed on day 3 and patient was discharged on day 4.
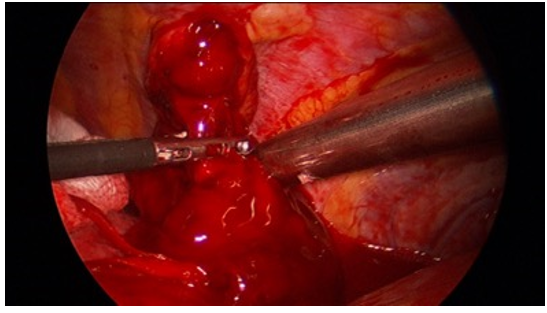
Figure 3: Intraoperative image showing evacuation of clots
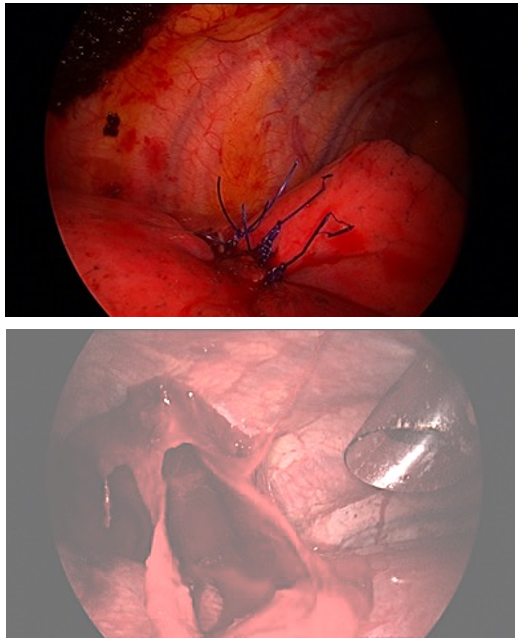
Figure 4: Sutured lung laceration
7) Uniportal VATS and chest trauma: As uniportal surgeries have become the new norm in the world of thoracic surgery. Chest trauma has not been left untouched. Rocco et al, in his series of uniportal surgeries has demonstrated that uniportal VATS is effective in evacuating hemothoraces [26]. Swierzy et al [27] have also shown effective application of uniportal VATS for chest trauma in hemodynamically stable patients. However, there are no comparative studies or trials to show that uniportal method is superior to traditional 3-port VATS in managing chest trauma patients.
Contraindications
It is essential for the trauma surgeon to know when not to use VATS. A hemodynamically unstable patient is a clear contraindication [9,10]. Patients with suspected cardiac injury, great vessel injury are other instances where VATS should not be used [8]. If there is a contraindication to the lateral position (spinal fractures) or single lung ventilation or patient is suffering from a bleeding diathesis VATS is contraindicated [10].
Conclusion
Surgeons dealing with trauma, should be familiar with VATS. It is important note that thoracoscopy is not a substitute for thoracotomy but is to be selectively used in a subgroup of patients, which may obviate the need for a thoracotomy.
References
- Wu N, Wu L, Qiu C, Yu Z, Xiang Y, et al. (2015) A comparison of video-assisted thoracoscopic surgery with open thoracotomy for the management of chest trauma: A systematic review and meta-analysis. World Journal of Surgery. Springer New York LLC. 39: 940-952. [PubMed.]
- Demirhan R, Onan B, Oz K, Halezeroglu S. (2009) Comprehensive analysis of 4205 patients with chest trauma: a 10-year experience☆. Interact Cardiovasc Thorac Surg. 9(3): 450-453. [PubMed.]
- Meyer DM, Jessen ME, Wait MA, Estrera AS. (1997) Early evacuation of traumatic retained hemothoraces using thoracoscopy: A prospective, randomized trial. Ann Thorac Surg. 64(5): 1396-1401. [PubMed.]
- Jones JW, Kitahama A, Webb WR, McSwain N. (1981) Emergency thoracoscopy: A logical approach to chest trauma management. J Trauma - Inj Infect Crit Care. 21(4): 280-284. [PubMed.]
- McKenna RJ, Houck W, Fuller CB. (2006) Video-assisted thoracic surgery lobectomy: Experience with 1, 100 cases. Ann Thorac Surg. 81(2): 421-425. [PubMed.]
- Seder CW, Wright CD, Chang AC, Han JM, Mcdonald D, et al. (2016) The Society of Thoracic Surgeons General Thoracic Surgery Database Update on Outcomes and Quality. Ann Thorac Surg. 101: 1646-1654. [PubMed.]
- Jackson AM, Ferreira AA. (1976) Thoracoscopy as an aid to the diagnosis of diaphragmatic injury in penetrating wounds of the left lower chest: a preliminary report. Injury. 7(3): 213-217. [PubMed.]
- Billeter AT, Druen D, Franklin GA, Smith JW, Wrightson W, et al. (2013) Video-assisted thoracoscopy as an important tool for trauma surgeons: A systematic review. In: Langenbeck’s Archives of Surgery. 515-523. [Ref.]
- Ahmed N, Jones D. (2004) Video-assisted thoracic surgery: State of the art in trauma care. Injury. 35(5): 479-489. [PubMed.]
- Margulies D, Milanchi S, Makey I, McKenna R. (2009) Video-assisted thoracoscopic surgery in the management of penetrating and blunt thoracic trauma. J Minim Access Surg. 5(3): 63-66. [PubMed.]
- Madden MR, Paull DE, Finkelstein JL, Goodwin CW, Marzulli V, et al. (1989) Occult diaphragmatic injury from stab wounds to the lower chest and abdomen. J Trauma - Inj Infect Crit Care. 29(3): 292-298. [PubMed.]
- Martinez M, Briz JE, Carillo EH. (2001) Video thoracoscopy expedites the diagnosis and treatment of penetrating diaphragmatic injuries. Surg Endosc. 15(1): 28-32. [PubMed.]
- Milfeld DJ, Mattox KL, Beall AC. (1978) Early evacuation of clotted hemothorax. Am J Surg. 136(6): 686-692. [PubMed.]
- Rombolá C, Crespo MG, López PT, Martínez AH, Atance PL, et al. (2016) Video-Assisted Minithoracotomy Diaphragmatic Plication: Respiratory Effects in Adults. Thorac Cardiovasc Surg. 64(8): 647-653. [PubMed.]
- Heniford BT, Carrillo EH, Spain DA, Sosa JL, Fulton RL, et al. (1997) The role of thoracoscopy in the management of retained thoracic collections after trauma. Ann Thorac Surg. 63(4): 940-943. [PubMed.]
- Smith JW, Franklin GA, Harbrecht BG, Richardson JD. (2011) Early VATS for blunt chest trauma: a management technique underutilized by acute care surgeons. J Trauma [Internet]. 71(1): 102-105. [PubMed.]
- Lin HL, Huang WY, Yang C, Chou SM, Chiang HI, et al. (2014) How early should VATS be performed for retained haemothorax in blunt chest trauma? Injury. 45(9): 1359-1364. [PubMed.]
- Huang FD, Yeh WB, Chen SS, Liu YY, Lu IY, et al. (2018) Early Management of Retained Hemothorax in Blunt Head and Chest Trauma. World J Surg [Internet]. 42(7): 2061-2066. [PubMed.]
- Lin HL, Tarng YW, Wu TH, Huang FD, Huang WY, et al. (2019) The advantages of adding rib fixations during VATS for retained hemothorax in serious blunt chest trauma - A prospective cohort study. Int J Surg. 65: 13-18. [PubMed.]
- Schermer CR, Matteson BD, Demarest GB, Albrecht RM, Davis VH. (1999) A prospective evaluation of video-assisted thoracic surgery for persistent air leak due to trauma. Am J Surg. 177(6): 480-484. [PubMed.]
- OʼBrien J, Cohen M, Solit R, Solit R, Lindenbaum G, et al. (1994) Thoracoscopic Drainage And Decortication As Definitive Treatment For Empyema Thoracis Following Penetrating Chest Injury. J Trauma Inj Infect Crit Care [Internet]. 36(4): 536-539. [PubMed.]
- Mandal AK, Thadepalli H, Mandal AK, Chettipalli U. (1997) Posttraumatic empyema thoracis: A 24-year experience at a major trauma center. J Trauma - Inj Infect Crit Care. 43(5): 764-771. [PubMed.]
- Kumar A, Asaf BB, Lingaraju VC, Yendamuri S, Pulle MV, et al. (2017) Thoracoscopic Decortication of Stage III Tuberculous Empyema Is Effective and Safe in Selected Cases. Ann Thorac Surg. 104(5): 1688-1694. [PubMed.]
- Merchant NN, Onugha O. (2018) Novel extra-thoracic VATS minimally invasive technique for management of multiple rib fractures. J Vis Surg. 4: 103-103. [PubMed.]
- Jin J, Song B, Lei Y, Leng X. (2015) Video-assisted thoracoscopic surgery for penetrating thoracic trauma. Chinese J Traumatol - English Ed. 18(1): 39-40. [PubMed.]
- Rocco G, Martucci N, La Manna C, Jones DR, De Luca G, et al. (2013) Ten-year experience on 644 patients undergoing single-port (Uniportal) video-assisted thoracoscopic surgery. Ann Thorac Surg. 96(2): 434-438. [PubMed.]
- Swierzy M, Faber S, Nachira D, Günsberg A, Rückert JC, et al. (2018) Uniportal video-assisted thoracoscopic surgery for the treatment of thoracic emergencies. In: Journal of Thoracic Disease. AME Publishing Company. S3720-3725. [Ref.]