>Corresponding Author : Mukherjee Sayantan
>Article Type : Case Report
>Volume : 3 | Issue : 5
>Received Date : 18 June, 2023
>Accepted Date : 30 June, 2023
>Published Date : 06 July, 2023
>DOI : https://doi.org/10.54289/JCRMH2300121
>Citation : Sayantan M, Jaspreet K, Bansal M and Navneet A. (2023) Acute Necrotising Encephalitis: A life threatening manifestation of Dengue Fever. J Case Rep Med Hist 3(5): doi https://doi.org/10.54289/JCRMH2300121
>Copyright : © 2023 Sayantan M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access
1GMCH, General Medicine, West Bengal, IN 700082
2RG Kar Medical College and Hospital, Kolkata, IN 700004
3GMCH, General Medicine Chandigarh, Punjab, IN
4Post Graduate Institute of Medical Education and Research, Internal Medicine Chandigarh, IN
*Corresponding author: Mukherjee Sayantan, Department of General Medicine, Government Medical College Chandigarh, Chandigarh Sector 32.
Abstract
Dengue fever is an arthropod-borne illness spread by Aedes aegypti, most commonly occurring in the tropics and subtropical regions of the world. Dengue virus is a flavivirus that manifests itself in the human body, in the form of an asymptomatic illness to a fulminant hemorrhagic disease. Expanded dengue syndrome covers the unusual manifestations that usually does not fall into the typical dengue fever, dengue shock syndrome, or dengue hemorrhagic fever. These findings call for greater in-depth research into these connections in order to help high-risk patients to be recognized promptly when they present to the hospital. High clinical suspicion with early aggressive measures are the only ways to attempt in reducing further mortality and morbidity.
Abbreviations: GCS: Glasgow Coma Scale, NCCT: Non Contrast Computed Tomography, CEMRI: Contrast Enhanced Magnetic Resonance Imaging, CSF: Cerebrospinal Fluid, CBNAAT: Cartridge Based Nucleic Acid Amplification Test, EDS: Expanded Dengue Syndrome, WHO: World Health Organization
Case Discussion
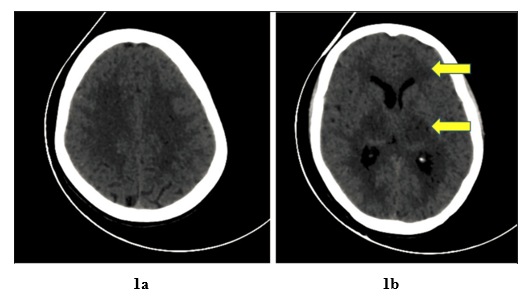
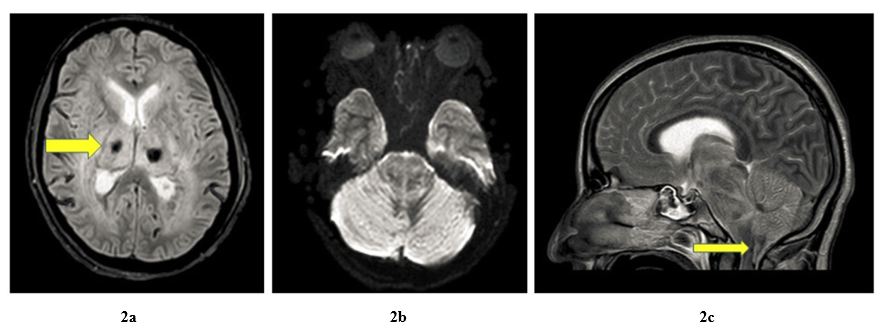
A 35-year-old female, housewife, presented to the hospital with altered sensorium, since the last 9 hours. She had a history of fever 10 days back; documented to be 100-101˚F for which she was prescribed antipyretics locally following which her fever had resolved. On presentation, her Glasgow Coma Scale (GCS) was E2V2M3, with bilateral sluggish pupils and bilateral plantar showing extensor response, with no evidence of neck rigidity. She was intubated in view of her poor GCS. Blood investigations were suggestive of a normal leukocyte count with thrombocytopenia and transaminitis. Serology for Dengue NS1 came out to be positive. Hepatitis A, E, B, C, HIV, Scrub Typhus IgM, and Malaria were all negative. Fundus examination was negative for papilledema. Her Non Contrast Computed Tomography (NCCT) Head revealed diffuse white matter oedema in the periventricular region (Figure 1a) and basal ganglia with effacement of the third and posterior horns of lateral ventricles. (Figure 1b, yellow arrows) During her stay in the hospital she underwent Contrast Enhanced Magnetic Resonance Imaging (CEMRI) of the brain with findings suggestive of Acute Necrotising Encephalitis (T2 FLAIR Figure 2a - showing necrosis in bilateral thalami and basal ganglia) or leucoencephalitis with cerebellum edema, descending transtentorial and tonsillar herniation. (Figure 2b and 2c) Subsequently her Cerebrospinal fluid (CSF) analyses revealed 2 cells with neutrophilic predominance and total sugar of 115, total protein of 360 and ADA of 13. CSF culture came out to be sterile and Cartridge based Nucleic acid amplification test (CBNAAT) test was negative. Based on her clinical and laboratory parameters provisional diagnosis of viral encephalitis was made. In view of her dengue serology being positive and signs and symptoms of encephalitis she was managed as a case of Expanded Dengue syndrome (EDS). She received intravenous fluids, inotropes, and mechanical ventilation, but despite best efforts the patient succumbed to her illness.
Discussion
Dengue fever according to World Health Organization (WHO) is suspected when a high fever (40˚F/104˚F) is followed by 2 of the following during the febrile phase (2-7) days: Severe headache/pain behind the eyes/muscle and joint pains/nausea/vomiting/swollen glands/rash. Severe dengue is a fatal complication due to leakage of plasma, fluid accumulation, respiratory distress, severe bleeding, or organ impairment [1].
Expanded Dengue syndrome (EDS) was coined for the atypical manifestations of Dengue virus which do not fall in the category of Dengue fever or Dengue Haemorrhagic fever [2]. The manifestations of expanded dengue syndrome presenting as neurological symptoms includes- encephalopathy, encephalitis, febrile seizures, infarcts, transverse myelitis, hypokalemic paralysis, mononeuropathy, polyneuropathy, Guillain Barre syndrome and intracranial bleed. A study conducted in 2012 in a teaching hospital found that gastrointestinal manifestations are the most common presentation of EDS with neurological manifestations being the second most common [3]. Guo-Hong Li et.al, in his study showed that out of all the dengue patients admitted to hospital 0.5-21% had encephalitis like features [4]. Another study by Carod-Artal FJ et. al, showed the incidence rate to be as high as 4-47% of dengue in patients with encephalitis-like illnesses [5].
The delayed manifestations affecting the nervous system as seen in our case is presumptively due to immunologically mediated neurological injury [5]. This injury results in cerebral oedema and haemorrhage, basal ganglia and thalamus complex bilaterally, and are frequently involved in vascular leaks, producing in a distinctive ‘double doughnut’ sign on MRI [6]. Other less commonly affected areas include the cerebellar hemispheres and brainstem. Our case depicts the involvement of these rarely and less commonly affected areas as well. Patients with neurological manifestations are rarely salvageable and have been shown to have high mortality [3,7]. Our case highlights the importance of early identification by proper timely brain imaging and by keeping high index of suspicion in dengue patients presenting to the emergency with neurological manifestations in preventing further mortality.
Declaration of Patient Consent: The authors certify that appropriate patient consent was obtained.
Financial Support and Sponsorship: Nil
Conflicts of Interest: There are no conflicts of interest.
References
- World Health Organization. (2023) Dengue and severe dengue. World Health Organization. [Ref.]
- Umakanth M, Suganthan N. (2020) Unusual Manifestations of Dengue Fever: A Review on Expanded Dengue Syndrome. Cureus. 12(9): e10678. [Ref.]
- Mohanty B, Sunder A, Pathak S. (2019) Clinicolaboratory profile of expanded dengue syndrome - Our experience in a teaching hospital. J Family Med Prim Care. 8: 1022-1027. [Ref.]
- Li GH, Ning ZJ, Liu YM, Li XH. (2017) Neurological Manifestations of Dengue Infection. Front Cell Infect Microbiol. 7: 449. [PubMed.]
- Carod-Artal FJ, Wichmann O, Farrar J, Gascón J. (2013) Neurological complications of dengue virus infection. Lancet Neurol. 12: 906-919. [PubMed.]
- Jugpal TS, Dixit R, Garg A, et al. (2017) Spectrum of findings on magnetic resonance imaging of the brain in patients with neurological manifestations of dengue fever. Radiol Bras. 50: 285-290. [Ref.]
- Rajapakse S, Wattegama M, Weeratunga P, Sigera PC, Fernando SD. (2018) Beyond thrombocytopaenia, haemorrhage and shock: the expanded dengue syndrome. Pathog Glob Health. 112: 404-414. [Ref.]