>Corresponding Author : Mukherjee Sayantan
>Article Type : Case Report
>Volume : 3 | Issue : 5
>Received Date : 18 June, 2023
>Accepted Date : 03 July, 2023
>Published Date : 10 July, 2023
>DOI : https://doi.org/10.54289/JCRMH2300122
>Citation : Sayantan M, Jaspreet K and Navneet A. (2023) Green Pleural Fluid: An Uncanny Encounter. J Case Rep Med Hist 3(5): doi https://doi.org/10.54289/JCRMH2300122
>Copyright : © 2023 Sayantan M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access
1GMCH, General Medicine, West Bengal, IN 700082
2RG Kar Medical College and Hospital, Kolkata, IN 700004
3GMCH, General Medicine Chandigarh, Punjab, IN
4Post Graduate Institute of Medical Education and Research, Internal Medicine Chandigarh, IN
*Corresponding author: Mukherjee Sayantan, Department of General Medicine, Government Medical College Chandigarh, Chandigarh Sector 32.
Abstract
Pleural effusions a commonly encountered case in clinical practice, warrants investigation via thoracocentesis, after a comprehensive physical and radiological workup [1]. Green pleural fluid is rarely seen in clinical practice and a case showing the same is portrayed in this report.
Introduction
Pleural effusion can have variety of colours based on the cause or underlying pathophysiology. It can range from being straw coloured in parapneumonic effusions/transudates, to chylous in neoplasms/tuberculosis/amyloidosis, to bloody as in trauma/pulmonary embolism. The proper treatment of pleural effusion can be done after meticulous differential diagnosis [2]. Purulent pleural effusion is generally found in Empyema and tuberculosis. But green coloured pus is a rare scenario, documented only in a post-traumatic bilothorax [3]. The current case shows a different scenario.
Case
A 40-year-old male, who was a chronic smoker and alcoholic for 20 years and a cocaine abuser 5 years who presented to the medicine emergency of Government Medical college and Hospital Chandigarh, with complaints of shortness of breath for 1.5 months which exacerbated over the last 4 days and right pleuritic sided chest pain x 4 days and fever (high grade, 102F) and cough with mild expectoration x 4 days. It was not associated with wheeze, or haemoptysis, swelling in the lower extremities, weight loss or anorexia. There was no history of any significant comorbidities. He had no history of tuberculosis or contact history of tuberculosis, or any known comorbidities. General physical examination was unremarkable. Chest X Ray done on admission was suggestive of right sided moderate pleural effusion. Pleural tap done under Ultrasound guidance was done showing a green coloured thick and viscous fluid which was suggestive of full field pus cells in the fluid with gram staining showing gram positive cocci in chains(?streptococci) , and fluid protein 2.1gm%, fluid ADA 147 IU/L, glucose 10. Patient was started on broad spectrum antibiotics after sending 3 sets of blood cultures and pus cultures. An Intercostal tube was inserted in view of empyema and the tube started draining frank green pus. Patient started showing clinical improvement on broad spectrum antibiotics 9injection piperacillin tazobactam) on day 2 and day three of therapy. Antitubercular therapy was not started during stay. Blood cultures sent were sterile after 5 days of incubation as well as pus cultures and sputum cultures showed mixed flora. 2D Echo done to rule out infective endocarditis was suggestive of a normal ejection fraction and no evidence of vegetation, clot, pericardial effusion. On day 5 of admission, ICD was removed after no evidence of pleural effusion and fully expanded lung. ICD was removed subsequently after pulmonology consult and patient was discharged on oral antibiotics.
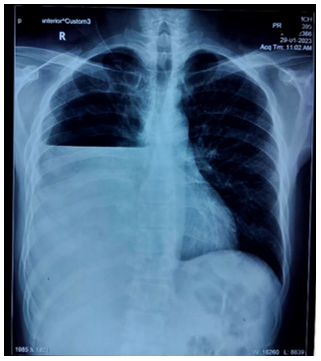
Figure showing the Chest x ray of the patient at presentation
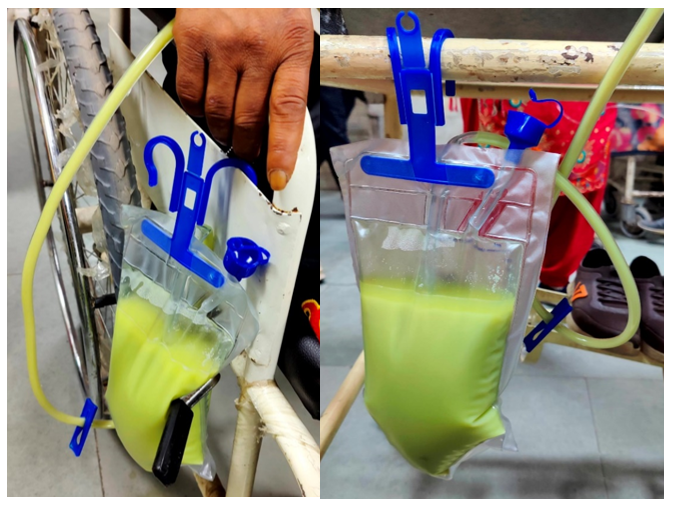
Figures showing the Intercostal drainage bag showing the green pus
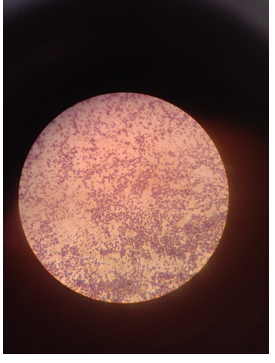
Figure showing gram positive cocci in chains seen in gram stain of pleural fluid
Discussion
Pleural fluid is analysed based on Light’s criteria to be transudative or exudative. These can be done by analysing the protein and albumin gradients between pleural fluids and serum [4]. Exudative pleural effusions are due to malignancy, pneumonia, tuberculosis, pulmonary embolism, pancreatic pseudocysts, intraabdominal abscesses [5]. When chylothorax is suspected then pleural fluid cholesterol and triglycerides play a role; whereas when even after pleural fluid analysis the cause remains doubtful, a three dimensional scanning, followed by thoracoscopy and pleural biopsy is recommended.
Green pus instantaneously reminds of a Pseudomonal infection [6]. But this case rarely showed the presence of gram positive cocci in chains in the gram stain from the pus once aspirated which in all likelihood would be streptococci which is a rare and undocumented case scenario.
Conclusion
Purulent pleural effusions although very commonly seen, should always be investigated to find out the cause. Cause based management should be instigated. The case scenario shows a case of a common organism exposing itself in a different way.
Conflicts of interest: None
References
- Porcel JM. (2011) Pearls and myths in pleural fluid analysis. Respirology. 16(1): 44-52. [PubMed.]
- Jany B, Welte T. (2019) Pleural Effusion in Adults-Etiology, Diagnosis, and Treatment. Dtsch Arztebl Int. 116(21): 377-386. [Ref.]
- Niekerk CV, Fan K, Sarcon A, Luu B. (2017) An Interesting Case of a Bilious Pleural Effusion. J Investig Med High Impact Case Rep. 5(3). [PubMed.]
- Romero-Candeira S, Hernández L, Romero-Brufao S, Orts D, Fernández C, et al. (2002) Is it meaningful to use biochemical parameters to discriminate between transudative and exudative pleural effusions? Chest. 122(5): 1524-1529. [PubMed.]
- Light RW. (2006) The undiagnosed pleural effusion. Clin Chest Med. 27(2): 309-319. [PubMed.]
- Wilson MG, Pandey S. (2022) Pseudomonas Aeruginosa. In: Stat Pearls [Internet]. Treasure Island (FL): Stat Pearls Publishing. [Ref.]