>Corresponding Author : Anurag Dahra
>Article Type : Case Report
>Volume : 3 | Issue : 5
>Received Date : 04 July, 2023
>Accepted Date : 26 July, 2023
>Published Date : 12 Aug, 2023
>DOI : https://doi.org/10.54289/JCRMH2300124
>Citation : Dahra A, Bansal S, Walia Y and Sharan S. (2023) Intracranial Vascular Complication of Mucormycosis: A Fascinating Report. J Case Rep Med Hist 3(5): doi https://doi.org/10.54289/JCRMH2300124
>Copyright : © 2023 Dahra A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access
1Junior Resident, Department of General Medicine, Government Medical College and Hospital, Chandigarh
2Medical Student, Government Medical College and Hospital, Chandigarh
3Junior Resident, Department of Pediatrics, Government Medical College and Hospital, Chandigarh
4Medical Student, Government Medical College and Hospital, Chandigarh
*Corresponding author: Anurag Dahra, Junior Resident, Department of General Medicine, Government Medical College and Hospital, Chandigarh
Abstract
We here present an unusual presentation of Mucormycosis in a 60-year-old vegetable vendor with history of uncontrolled diabetes. Patient presented only with headache, ophthalmoplegia and right eyelid drooping. Radiological investigations of the head showed obliteration of all the paranasal sinuses along with orbital abscess. Biopsy of nasal scrapings was done and patient was diagnosed with rhino-orbital-cerebral Mucormycosis.
Abbreviations: ROCM: Rhino-Orbital-Cerebral Mucormycosis
Introduction
Mucormycosis is a fungal infection caused by species of genera Mucorales. Rhizopus species are the most common cause of mucormycosis responsible for almost 48% of cases [1]. It is difficult to estimate the exact incidence of mucormycosis as it is not a reportable disease [2]. Species of Mucorales are ubiquitous in nature but they are normally removed by our immune system. That’s why mucormycosis occurs mostly in the presence of a condition compromising our immune system [2]. Diabetes mellitus is the most common risk factor found in 40% of cases, followed by hematologic malignancies found in 32% of cases, followed by solid or hematopoietic stem cell transplantation in 14% of the cases [1]. Rhino-orbital-cerebral infection is the most common presentation responsible for almost 34% of the cases [1]. It has a very high rate of mortality ranging from 25-62% [2]. There were numerous case reports of association between COVID-19 and mucormycosis [3]. Most of these case reports originated from India. We present a case of mucormycosis with unusual presentation.
Case presentation
A 66-year-old male vegetable vendor with past medical history of diabetes mellitus and hypertension for 5 years and is non-compliant with medication presented to the Emergency department with 5 days of right occipital headache. It was associated with difficulty opening the right eye. There was no associated history of altered sensation, smell, or similar complaints in the past.
On examination, vitals were stable and neurological examination showed normal motor, sensory, and cerebellar function tests. Ophthalmological examination showed complete ophthalmoplegia of the right eye, and drooping of the right eyelid. Labs were significant for leukocytosis and HbA1c of 9.3 mg/dl. NCCT head was done which showed obliteration of all paranasal sinuses despite no symptoms of sinusitis (Figure 1) and right orbital abscess along with the possibility of cavernous sinus thrombosis. Additionally, a wedge-shaped hypodense area in the right parieto-occipital region with loss of grey-white differentiation was seen which was suggestive of brain infarct. CEMRI was done to evaluate the extent of the infarct which depicted an acute right PCA infarct involving the right parieto-occipital lobe with attenuation of P3 and P4 segments of PCA. Additionally, it showed right ICA thrombosis as well which was unexpected (figure 2). Contrast-enhanced angiography was done which showed involvement of the entire right ICA resulting in non-opacification. Anterior and middle cerebral artery circulation was maintained through the flow from the contralateral side via the circle of Willis (figure 3), while during venous phase it showed no flow in right cavernous sinus (figure 4). Endoscopic evaluation of sinuses was done and scraping from the sinus was sent for examination. KOH mount was made and it revealed broad, aseptate hyphae with right angle branching suggestive of Mucormycosis (figure 5).
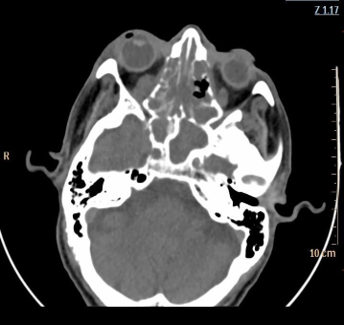
Figure 1: Pansinusitis with hypodense material filled up in ethmoid sinus and nasal cavity with obliteration of medial wall of right orbit along with extension of same in that cavity
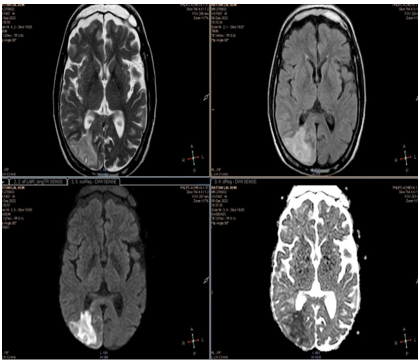
Figure 2: Pansinusitis with hypodense material filled up in ethmoid sinus and nasal cavity with obliteration of medial wall of right orbit along with extension of same in that cavity
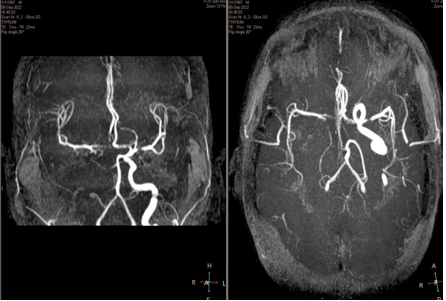
Figure 3: Contrast enhanced angiography showing right Internal carotid artery nonopacification due to occlusion but flow to anterior and middle cerebral artery was maintained through contralateral circulation
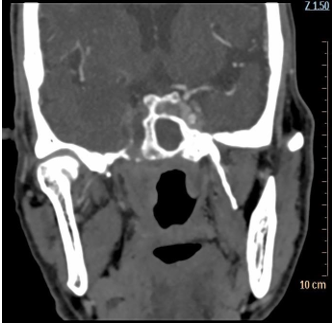
Figure 4: Cect head during venous phase showing no flow in right cavernous sinus
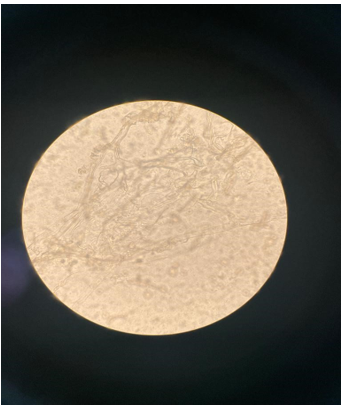
Figure 5: KOH wet mount showing aseptate hyphae with right angle branching
Once the diagnosis of rhino-cerebral mucormycosis was made, patient underwent endoscopic debridement and medical management with liposomal amphotericin B. The patient responded well and was discharged home as he was hemodynamically stable and was able to perform activities of his daily living. Ptosis and ophthalmoplegia were not resolved as there were irreversible changes but we were able to prevent further progression of this fatal disease.
Discussion
Mucormycosis is a highly fatal disease with 46% mortality rate [1]. Most common route of infection is inhalation of spores which are normally pushed to pharynx with the help of cilia and thus removed by gastrointestinal system whereas in susceptible patients these spores cause infection either in nasal turbinates or after going in alveoli [4]. Patients with diabetes mellitus are most vulnerable to mucormycosis. 40% of patients with mucormycosis have history or are diagnosed with diabetes mellitus on presentation and 20% of the patients present with Diabetic ketoacidosis [1]. There are various proposed mechanisms by which hyperglycemia in DM increases the risk of mucormycosis: a) hyperglycation of ironsequestering proteins hindering normal iron sequestration; b) upregulation of GRP78 receptor which binds to Mucorales, enabling penetration of tissues; c) causes defects in phagocytic function [5].
Mucormycosis is highly angio-invasive and rapidly progressive infection causing various different clinical manifestations [5]. Clinical manifestations can be of 6 different types: Rhinoorbital-cerebral, pulmonary, cutaneous, gastrointestinal, disseminated and miscellaneous.
Patients with different predisposing risk factors develop different clinical presentations. Those with diabetes mellitus develop rhino-orbital-cerebral mucormycosis (ROCM) in 43% cases [2]. ROCM usually presents clinically as fever, nasal congestion, purulent nasal discharge, sinus pain and headache. Usually, within a few days, all the sinuses are affected. After damaging the sinus wall, fungus can infiltrate the orbit and causes periorbital edema, proptosis, and blindness. It can enter the cavernous sinus hematogenously or by continuous spread from the orbits. Cavernous sinus involvement results in cranial nerve palsy, carotid artery involvement, and may result in symptoms in the opposite eye. Facial numbness is common due to infarction of sensory branches of facial nerve. But all these symptoms are not necessarily present in all the patients. According to a study by Yohai et al, fever is present in 44% of patients, Nasal ulceration in 38%, periorbital swelling in 34%, decreased vision in 30%, ophthalmoplegia in 29%, sinusitis in 26%, headache in 25% [6]. We need to have a high index of suspicion to detect this infection especially in high risk groups like diabetes mellitus because it could be rapidly fatal. Our patient presents only with headache and drooping of right eyelid, there was decreased vision but the patient had a cataract so fundus could not be examined. Apart from this, our patient did not have any other symptom which could prompt us for mucormycosis. We did CT scan to look for stroke which this patient had but along with the stroke, the patient also had obliteration of all the sinuses which made us think of the possible mucormycosis infection.
Biopsy with histopathological examination of the suspected site is the most sensitive and specific modality for definitive diagnosis of mucormycosis. It shows aseptal hyphae which branch at right angles [5]. Culture may come negative in more than half of the cases of mucormycosis. The reason for low sensitivity for culture in these patients is long filamentous structure of Mucorales species which got killed during the process of tissue homogenization [7]. In our patient, we took biopsy of the sinus tissue and visualized under KOH wet mount which showed aseptate hyphae with right angle branching and confirmed the diagnosis of mucormycosis (figure).
There are 3 elements of management of mucormycosis patients: 1) Medical management with antifungal agents. 2) Surgical debridement and 3) Elimination of predisposing factors such as hyperglycemia, immunosuppression, neutropenia, and deferoxamine administration [8]. For best prognosis, all 3 things should be done simultaneously. Liposomal amphotericin B is the drug of choice for management of mucormycosis as this is less nephrotoxic than traditional amphotericin B [5]. Aggressive surgical debridement of involved tissues should be considered as soon as diagnosis of mucormycosis is suspected. Most significant factors associated with high mortality rate are leukemia, hemiplegia/hemiparesis, bilateral sinus involvement, renal disease and treatment with deferoxamine [6]. We gave liposomal amphotericin B and endoscopic surgical debridement and limits the progression of the disease.
Conclusion
This case highlights an unusual presentation of mucormycosis, emphasizing the importance of maintaining a high index of suspicion, particularly in high-risk groups. Early diagnosis, multidisciplinary management, and aggressive treatment are essential for improving patient outcomes in this potentially life-threatening fungal infection.
Patient’s Perspective
“We heard about the black fungus during COVID pandemic, when awareness was spread about the alarming signs and symptoms. With covid pandemic settling down I never expected one of our family members to get affected by the same with such a different scenario. With all the management being done, even surgery, we hope the disease does not spread more.” – quoted by one of the family members of the patient.
References
- Jeong W, Keighley C, Wolfe R, et al. (2019) The epidemiology and clinical manifestations of mucormycosis: a systematic review and meta-analysis of case reports. Clinical Microbiology and Infection. 25(1): 26-34. [PubMed.]
- Roden MM, Zaoutis TE, Buchanan WL, et al. (2005) Epidemiology and outcome of zygomycosis: a review of 929 reported cases. Clin Infect Dis. 41(5): 634-653. [Ref.]
- Joshi S, Telang R, Tambe M, et al. (2022) Outbreak of Mucormycosis in Coronavirus Disease Patients, Pune, India. Emerg Infect Dis. 28(1): 1-8. [Ref.]
- Ferguson BJ. (2000) Mucormycosis of the nose and paranasal sinuses. Otolaryngol Clin North Am. 33(2): 349-365. [PubMed.]
- Spellberg B, Ibrahim AS. (2018) Mucormycosis. Harrison’s Principles of Internal Medicine. 20th ed. McGraw-Hill Education. [Ref.]
- Yohai RA, Bullock JD, Aziz AA, Markert RJ. (1994) Survival factors in rhino-orbitalcerebral mucormycosis. Surv Ophthalmol. 39(1): 3-22. [PubMed.]
- Bavikar P, Mehta V. (2017) Rhino-Orbital-Cerebral Mucormycosis: A Fatal Complication of Uncontrolled Diabetes Mellitus. Cureus. 9(11): e1841. [Ref.]
- Spellberg B, Walsh TJ, Kontoyiannis DP, Edwards J, Ibrahim AS. (2009) Recent advances in the management of mucormycosis: from bench to bedside. Clin Infect Dis. 48(12): 1743-1751. [Ref.]