>Corresponding Author : S Haddadi
>Article Type : Case Report
>Volume : 3 | Issue : 8
>Received Date : 15 Nov, 2023
>Accepted Date : 27 Nov, 2023
>Published Date : 02 Dec, 2023
>DOI : https://doi.org/10.54289/JCRMH2300139
>Citation : Haddadi S, Adda-Abbou F, Khelafi L, Messaoud YY, Baba A, et al. (2023) Posttraumatic Ileal Perforation in Crohn's Disease A Case Report. J Case Rep Med Hist 3(8): doi https://doi.org/10.54289/JCRMH2300139
>Copyright : © 2023 Haddadi S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access
1Surgery Department A. Central Hospital of the Army Docteur Mohamed Seghir Nekkache. BP 244, Kouba, Algiers
2Algiers University I Benyoucef Benkhedda, Medecine Faculty, Algiers, Algeria
*Corresponding author: S Haddadi, Surgery Department A. Central Hospital of the Army Docteur Mohamed Seghir Nekkache. BP 244, Kouba, Algiers and Algiers University I Benyoucef Benkhedda, Medecine Faculty, Algiers, Algeria
Abstract
Introduction: Free peritoneal perforations in Crohn's disease are extremely rare. In this observation, we report the case of a patient who presented with this condition following abdominal blunt trauma.
Case presentation: This is a 30-year-old patient with Crohn's disease who was being followed anarchically. She presented with peritonitis following violent abdominal blunt trauma, which was operated on with some diagnostic delay.
Discussion: Abdominal blunt trauma could lead to small bowel perforation in patients with Crohn's disease. Especially when the small bowel is weakened by non-adherence to therapy, as in our case.
Diagnosis is often delayed, as the clinical signs are discreet. On the other hand, trauma surgeons focus more on solid organs than hollow ones.
Conclusion: Abdominal blunt trauma in Crohn's disease increase the risk of occurrence of perforated bowel, especially when the therapeutic follow-up of these patients is not rigorous or in the event of non-adherence to therapy. Delayed diagnosis of these perforations may increase their morbidity.
Keywords: Crohn's disease-Perforation- Blunt abdominal trauma
Abbreviations: CD: Crohn's Disease
Introduction
Crohn's disease (CD) is a chronic inflammatory disease of the digestive tract that rarely perforates on free peritoneum. These perforations occur almost exclusively in the small bowel, either in the middle of a lesion or, more rarely, upstream of a stricture. During the course of these diseases, there is a parallel progression of inflammation and intestinal "destruction". Traumatic intestinal and mesenteric lesions occur in 1-5% of patients with closed abdominal trauma. Perforations are most often secondary to violent traumas; their diagnosis is suspected on the basis of intense pain and peritoneal signs. However, symptoms are often discreet, delaying diagnosis and clouding prognosis. Emergency CT can confirm the diagnosis. Most digestive lesions are an indication for laparotomy, unlike solid organ lesions. We report a rare case of ileal perforation peritonitis in Crohn's disease following blunt abdominal trauma.
Clinical observation
Patient RN, aged 30, smoker, followed for Crohn's disease but having stopped her treatment of her own accord. As a result, she presents with diarrhea at a rate of 03 bowel movements per day. At 2pm the previous day, she had been involved in a traffic road accident resulting in abdominal blunt trauma. She was initially treated in a public hospital, where an abdominal emergency was ruled out. The patient returned to our hospital the following day at 6 p.m. with diffuse abdominal pain associated with fever. On examination, the patient was WHO 0, hemodynamically stable (Blood pressure: 10/06 cmHg, HR: 86 b/min) with a fever at 38.5 C. The rest of clinical examination revealed contusion lesions mainly over the right iliac wing and calf. Generalized abdominal contracture on palpation was noticed. Rectal examination was unremarkable. Biological workup was normal, except for a hyperleukocytosis of 15700/mm3.
A body computed tomography was performed, revealing circumferential parietal thickening of the last ileal loop, measuring 10 mm and extending over 30 cm, with arterial enhancement and parietal loss of substance of an ileal loop estimated at 02 cm in extent, located 10 cm from the ileo-caecal junction, with multiple air bubbles and fluid opposite. This was associated with infiltration of mesenteric fat. The imager concluded that the peritonitis was due to perforation of the last ileal loop in Crohn's disease (figures 1 and 2).

Figure 1.Computed tomography section showing extra-digestive air bubbles opposite the last ileal loop (red arrow)
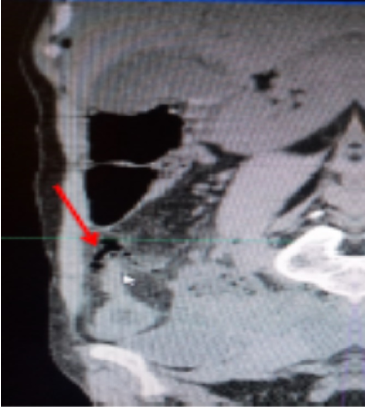
Figure 2.Computed tomography (coronal section) showing extra-digestive air bubbles (red arraow) opposite the last ileal loop which is thickened
The patient underwent emergency surgery, and intraoperative exploration revealed a cardboard ileal loop with sclerolipomatosis, the site of a 07 mm perforation leaking digestive fluid (figure 3). An ileocaecal resection was performed, with closure of the distal colonic end and stoma of the proximal ileal end. Abundant peritoneal lavage with isotonic saline was performed. The patient underwent antibiotic therapy with ertapenem 1g/d and preventive anti-coagulation with lovenox 40ui/d. Post-operative follow-up was straightforward, with the patient discharged on postoperative day 8. Re-establishment of digestive continuity was carried out 03 months later in another hospital department, as the patient resided abroad.
Eighteen month after the accident, the patient's progress was favourable under the medical treatment instituted by her gastroenterologist. Beyond that, the patient was lost to follow-up.
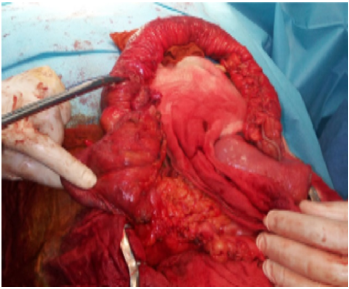
Figure 3.Intraoperative view of ileal perforation
Discussion
Post-traumatic perforations in Crohn's disease are extremely rare [1]. The mesenteric edge of longitudinal ulcers is the preferred site for these perforations [2]. In our case, the vulnating agent is thought to be the seatbelt, which compressed the intestine weakened by the untimely cessation of treatment.
The clinical signs of intestinal-mesenteric injury (abdominal pain and peritoneal irritation) are often non-specific or delayed in onset in cases of abdominal blunt trauma. A delay of only 8 to 12 hours in the diagnosis of these injuries increases morbidity and mortality threefold. Traumatic ruptures occur preferentially at anatomical fixation points: the duodeno-jejunal angle (ligament of Treitz) and the ileocaecal valve. Perforations complicating Crohn's disease are perforations covered by other intestinal structures, but perforations in the free peritoneum are exceptional [3]. Hemodynamically stable or stabilized patients should benefit from further investigations. CT has become the method of choice for assessing hemodynamically stable abdominal trauma patients. The results of various studies show sensitivities ranging from 69 to 95% and specificities from 94 to 100% for their diagnosis [4]. Its diagnostic superiority in the detection of intestinal-mesenteric lesions over clinical examination, peritoneal lavage and ultrasonography is now well recognized [5]. Intra-operatively, the presence of advanced peritonitis should prompt the surgeon to perform a sparing resection with a stoma at both ends of the bowel when there is a bowel perforation. Restoring continuity in this context can lead to anastomotic release, as in the case of Tomita et al [3]. A terminal ileostomy was performed in our case, after stapling with GIA forceps (Ethicon) of the distal ileum flush with the ceacum. In our case, the diagnosis was made late, and was revealed by a generalized peritonitis, with perforation in the free peritoneum. Ultrasound initially revealed only a thickening of the last ileal loop, the preferred site for post-traumatic perforations, which have been attributed to Crohn's disease.
Conclusion
Abdominal blunt trauma in the case of Crohn's disease increase the risk of perforation, especially when patients are not rigorously monitored or when they fail to comply with treatment. Late diagnosis of these perforations increases their morbidity. As a result, these "doubly inflicted" patients need to be hospitalized in a surgical environment. Only armed clinical monitoring will enable timely decisions to be made, and patients to be saved.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Bibliography
- Johnson GA, Baker J. (1990) Colonic perforation following mild trauma in a patient with Crohn’s disease. Am J Emerg Med. 8(4): 340-341. [PubMed.]
- Ikeuchi H, Yamamura T. (2002) Free perforation in Crohn’s disease: review of the Japanese literature. J Gastroenterol. 37(12): 1020-1027. [PubMed.]
- Tomita H, Hojo I, Yasuda S, Nakamura T, Takemura K, et al. (1993) Jejunal perforation caused by blunt abdominal trauma in a patient with Crohn’s disease: report of a case. Surg Today. 23(12): 1099-1102. [PubMed.]
- Regent D, Balaj C, Jausset F, Oliver A, Sellal-Aubriot C, et al. (2014) Perforations du tube digestif. Feuillets de Radiologie. 54(1): 9-31. [Ref.]
- Faget C, Millet I, Ruyer A, Alili C, Taourel P. (2023) Masson E. EM-Consulte. Traumatismes du tube digestif et du mésentère. [Ref.]