>Corresponding Author : Achraf El Kabli
>Article Type : Case Report
>Volume : 3 | Issue : 9
>Received Date : 21 Nov, 2023
>Accepted Date : 04 Dec, 2023
>Published Date : 08 Dec, 2023
>DOI : https://doi.org/10.54289/JCRMH2300142
>Citation : Kabli AE, Mhaber S, Mourabit S, Echchilali K, Moudatir M, et al. (2023) Breast Cancer and Autoimmune Hemolytic Anemia: A Rare Paraneoplastic Syndrome. J Case Rep Med Hist 3(9): doi https://doi.org/10.54289/JCRMH2300142
>Copyright : © 2023 Kabli AE, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access
1Resident Physician, Department of Internal Medicine, Ibno Rochd University Hospital, Casablanca, Morocco
2Professor in the Department of Internal Medicine at the Ibno Rochd University Hospital in Casablanca, Morocco
*Corresponding author: Achraf El kabli, Resident Physician, Department of Internal Medicine, Ibno Rochd University Hospital, Casablanca, Morocco
Abstract
Autoimmune hemolytic anemia (AIHA) is a pathological process involving the destruction of red blood cells by the humoral immune system. Although there is a well-established relationship between the presence of AIHA and lymphoproliferative malignancies, AIHA rarely presents in association with solid malignancies. Few cases of solid cancer associated with AIHA have been reported. AIHA rarely presents as a paraneoplastic syndrome indicative of solid cancer. We report a case of breast cancer revealed by AIHA.
Keywords: Autoimmune Hemolytic Anemia; Breast Cancer; Solid Tumor; Paraneoplastic Syndrome
Abbreviations: AIHA: Autoimmune Hemolytic Anemia, IgG: Immunoglobulins G, IgM: Immunoglobulins M, IgA: Immunoglobulins A, NSCLC: Non-Small Cell Lung Cancer, DIC: Disseminated Intravascular Coagulation
Introduction
The paraneoplastic manifestation of hemolytic anemia in patients with solid tumors is often a sign of poor prognosis. In rare cases, it is a feature of an occult primary malignant neoplasm. Hemolysis usually occurs late in the course of the disease and manifests abruptly as severe anemia. We report a case of hemolytic anemia in breast carcinoma.
Case report
A 32-year-old patient with no previous medical history was admitted for etiological assessment of a recently worsening anemia syndrome evolving 5 months prior to admission. Clinical examination on admission showed signs of poor tolerance of her anemia, and a rapid CBC showed a highly regenerative normocytic normochromic anemia at 6 g/l with no abnormalities in other blood lines. After stabilizing the patient, the rest of the clinical examination revealed diffuse bone pain and a suspicious breast mass measuring 2x2cm in the upper-external quadrant of the left breast, classified as ACR BIRADS 4 on echomammography, the tru-cut needle biopsy concluded to a nonspecific invasive breast carcinoma grade III SBR with positive hormone receptors, with pleural and parenchymal, hepatic, splenic and diffuse osteomedullary involvement in the extension work-up. The rest of the laboratory work- up showed hypercalcemia at 113 mg/l, a positive Coombs test, biological signs of hemolysis (elevated LDH and bilirubin and collapsed haptoglobin) and a CA 15-3 at 10 times normal. After correcting her hypercalcemia, the patient was transferred to oncology, where she died before receiving chemotherapy.
Case report
Autoimmune hemolytic anemia (AIHA) results from the production of antibodies against the patient's red blood cells, inducing excessive, uncompensated hemolysis. Typically, these antibodies are immunoglobulins G (IgG), which can fix the complement, sometimes immunoglobulins M (IgM), and more rarely immunoglobulins A (IgA). The temperature at which antibodies fix to erythrocytes subdivides AIHA into warm (most often IgG), cold or mixed forms.
50% of AIHA cases are idiopathic. Mature B-cell lymphoproliferative diseases, autoimmune diseases and drugs are the most frequent causes of secondary AIHA [1]. Associated oncological diseases are listed in Table 1.
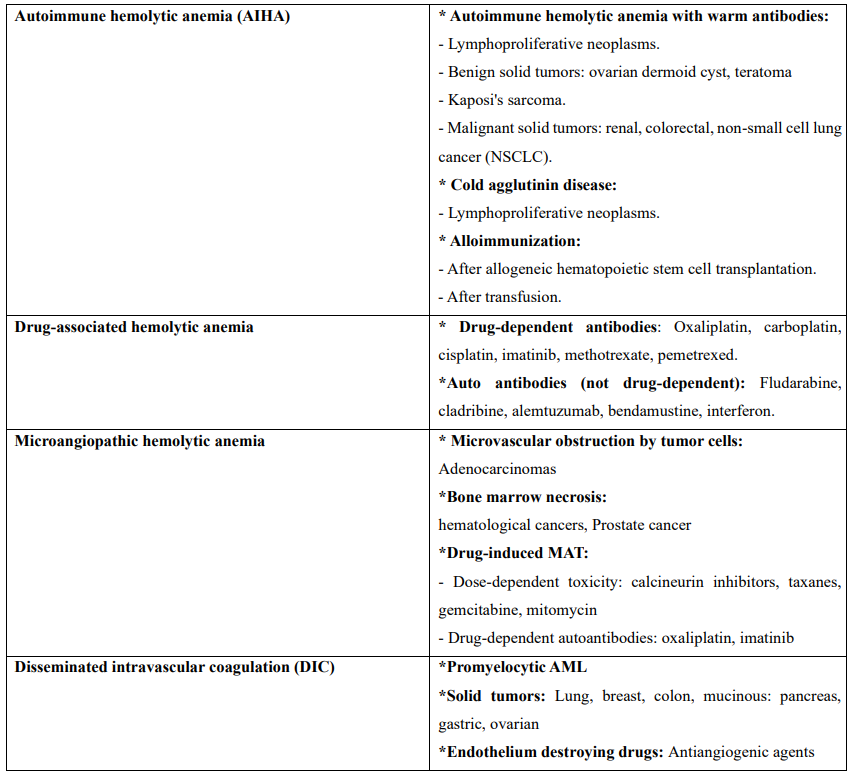
Table 1. Types of hemolytic anemia in oncology [2,3]
AIHA may appear before, during or after the management of an oncological disease, including during complete remission; it may also be a sign of recurrence. The diagnosis of AIHA is made After exclusion of an alternative cause of hemolysis (transfusion reaction, drug reaction, alloimmunization After hematopoietic stem cell transplantation).
There are 2 reported cases in the literature that show an associated malignant mesothelioma solid tumor with AIHA [4]. There are only a few reported cases of malignant solid breast cancer with AIHA [5,6].
In view of the frequent association of AIHA with oncological diseases, it is reasonable to perform a work-up for lymphoproliferative disease with thoraco-abdomino-pelvic CT-scan and/or bone marrow biopsy in patients with new-onset AIHA.
Treatment of the AIHA depends on the characteristics of the concurrent solid tumor. In the event of AIHA, general measures should be applied, such as the administration of folic acid, thromboprophylaxis according to the parent’s individual risk, and the prevention of cortico-induced osteoporosis and gastrointestinal bleeding in patients treated with corticosteroids. Erythrocyte transfusion may be necessary in the presence of severe, life threatening anemia, and effective treatment of the underlying pathology can often correct hemolysis. Empirical administration of corticosteroids remains the first-line treatment. The usual dose is 1-1.5 mg/kg daily for two weeks, until hemoglobin > 120 g/l. This dose is then reduced by 20 mg per week to a dose of 20 mg/day, followed by a slower progressive reduction over 4 to 8 weeks [1].
Splenectomy may be less effective in refractory cases.
Conclusion
Hemolytic anemia is generally a rare paraneoplastic phenomenon with an abrupt onset and rapidly severe course. This is a rare case of breast cancer with a solid mass, revealed by AIHA Mechanisms underlying associations between solid tumors and AIHA are unclear. However, correlating hemolytic activity with disease progression or recurrence could be potentially useful in disease monitoring [7]. A more detailed study of patients with breast cancer and AIHA will provide more information on the underlying etiological mechanisms.
Mortality in patients with paraneoplastic hemolytic anemia remains very high. Initiation of appropriate chemotherapy can lead to resolution.
References
- Go R, Winters J, Kay N. (2017) How I treat autoimmune hemolytic anemia. Blood. 129: 2971-2979. [Ref.]
- Puthenparambil J, Lechner K, Kornek G. (2010) Autoimmune hemolytic anemia as a paraneoplastic phenomenon in solid tumors: a critical analysis of 52 cases reported in the literature. Wien Klin Wochenschr. 122: 229-236. [PubMed.]
- GarraFy G, Arndt PA. (2014) Drugs that have been shown to cause drug-induced immune hemolytic anemia or positive direct antiglobulin tests: some interesting findings since 2007. Immunohematol. 30: 66-79. [PubMed.]
- Selleslag DL, Geraghty RJ, Ganesan TS, Slevin ML, Wrigley PF, et al. (1989) Autoimmune hemolytic anaemia associated with malignant peritoneal mesothelioma. Acta Clin Belg. 44: 199-201. [PubMed.]
- Calderoni A, AltermaF HJ, Pirovino M. (1994) Autoimmune processes as paraneoplastic manifestations in familial breast carcinoma [in German]. Dtsch Med Wochenschr. 119: 1194-1198. [PubMed.]
- Adorno G, Girelli G, Perrone MP, et al. (1991) A metastatic breast carcinoma presenting as autoimmune hemolytic anemia. Tumori. 77: 447-448. [PubMed.]
- Loh KP, Kansagra A, Asik A, Ali A, Dahiya S. (2015) Paraneoplastic autoimmune hemolytic anemia in ovarian cancer: a marker of disease. Rare Tumors. 7: 5598. [PubMed.]