>Corresponding Author : Omali H
>Article Type : Case Report
>Volume : 3 | Issue : 9
>Received Date : 03 Dec, 2023
>Accepted Date : 15 Dec, 2023
>Published Date : 20 Dec, 2023
>DOI : https://doi.org/10.54289/JCRMH2300143
>Citation : Omali H, Barakat L, Benzakour M, Echchilali K, Moudatir M, et al. (2023) Association of Sarcoidosis and Primary Biliary Cirrhosis: A New Observation. J Case Rep Med Hist 3(9): doi https://doi.org/10.54289/JCRMH2300143
>Copyright : © 2023 Omali H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access
Department of Internal Medicine, CHU IBN ROCHD, Casablanca
*Corresponding author: Omali H, Department of Internal Medicine, CHU IBN ROCHD, Casablanca
Introduction
Sarcoidosis is a systemic disease of unknown etiology. It is characterized by the presence of noncaseating granulomatous lesions in the affected organs. Primary biliary cirrhosis (PBC) is a chronic autoimmune cholestatic hepatopathy characterized by destruction of the bile ducts and the presence of M2-type anti-mitochondrial antibodies [1]. The association of sarcoidosis and primary biliary cirrhosis reported here is rare. It poses a problem of histological differential diagnosis and raises the hypothesis of an etiopathogenic link between the two conditions [2]. We report the clinical case of a patient hospitalized in the internal medicine department of chu ibno rochd casablanca, who was diagnosed with a combination of sarcoidosis and primary biliary cirrhosis.
Clinical case
This is a 49-year-old patient admitted for etiological assessment of bilateral granulomatous uveitis, who has been presenting with inflammatory arthralgias involving both knees, both ankles, both elbows and both wrists for 5 years, the two elbows and the two wrists associated with an ocular involvement made of a bilateral granulomatous uveitis and a dry syndrome the symptomatology was enriched two months later by the appearance of a dyspnea stage II with in the thoracic CT a diffuse interstitial pneumopathy and the appearance of a pruritus ²generalized the whole evolving in a context of conservation of the general state. An etiological work-up was carried out, and serologies came back negative (HIV, syphilis, hepatitis B and C, toxoplasmosis, herpes, CMV EBV), the conversion enzyme assay came back high at 111 U/L, labial biopsy revealed a granuloma; overall, the diagnosis of sarcoidosis with pulmonary and ocular involvement was made on the basis of elevated ACE, the presence of a granuloma on labial biopsy and the granulomatous nature of the uveitis, In terms of treatment, the patient was put on high-dose oral corticosteroids with degression associated with methotrexate at a rate of 15 mg/week. The evolution was marked by regression of the signs of uveitis, with the appearance of cytolysis and a biological cholestasis greater than 3 times normal, methotrexate was incriminated, which necessitated stopping methotrexate for a week, but the cytolysis persisted. A liver immunoassay was then performed, which showed positive anti-Mi2 antibodies. Overall, the diagnosis of a combination of sarcoidosis and primary biliary cirrhosis was accepted.
Therapeutically, the patient was put on high-dose corticosteroids with tapering off, combined with azathioprine 150 mg/day and ursodeoxycholic acid 200 mg 2 capsules/day with good progression, including negativation of cytolysis and cholestasis.
Discussion
Sarcoidosis is a systemic disease of unknown etiology [3], primarily affecting the respiratory and lymphatic systems, and characterized by the formation of immune granulomas in the affected organs [4-6].
Hepatic granuloma is encountered in sarcoidosis in 15-65% of patients, and is characterized by a concentric, well-demarcated, numerous structure localized in the portal and periportal zone. Whereas granulomas in PBC are characterized by their small number, they are poorly defined and associated with a lymphocytic infiltrate adjacent to the biliary lesions. The lymphocytic infiltrate of granulomas in both diseases shows an accumulation of CD4 (helper) T cells in the center of the granuloma. Whereas CD8 (cytotoxic) T cells are seen at the periphery of sarcoidosis granulomas and near the bile ducts in PBC [7,8].
Primary biliary cirrhosis (PBC) is an autoimmune disease with an estimated annual incidence of 10-20/100,000. It is most often diagnosed in women in their fourth or fifth decade. Its prevalence in families of patients with PBC is 4% [9].
The detection of anti-mitochondrial antibodies (AMA) is important in the diagnosis of PBC, with a sensitivity of 90% and specificity of 95%, while anti-mitochondrial antibodies type M2 have a specificity of 100% [3]. Other immunological abnormalities have been described, notably the detection of antinuclear antibodies and increased immunoglobulins (IGM) [1].
Liver biopsy, which is not compulsory for the diagnosis of
PBC, is essentially used to staging the disease and to show the characteristic lesions of this condition on histology, namely nonsuppurative cholangitis affecting the interlobular and septal bile ducts. The inflammatory infiltrate is composed mainly of lymphocytes and mononuclear cells in direct contact with the basement membrane of necrotic cholangiocytes. Portal inflammation may take the form of epithelioid granulomas [1,10].
In our case, the diagnosis of sarcoidosis was based on the clinico-biological, radiological and histological presentation. The diagnosis of PBC was based on the presence of cholestasis and the positivity of anti-mitochondria type M2 antibodies. Kishor et al had recently reported 17 patients with sarcoidosis and PBC and suggested that a common pathway contributes to granuloma formation in both conditions. One explanation for the apparent association between these conditions is that both share the same defect in cell-mediated immunity [1,11].
The association of systemic sarcoidosis with PBC remains rare. Twenty well-documented cases have been reported in the literature (Table 1). These are two hepatic granulomatoses whose differential diagnosis is sometimes very difficult to establish in practice. However, certain clinical, biological, immunological and histological parameters help to guide the clinician (Table 2) [1]. In our case, the diagnosis of primary biliary cirrhosis was revealed clinically by pruritus and biologically by a cholestasis syndrome.
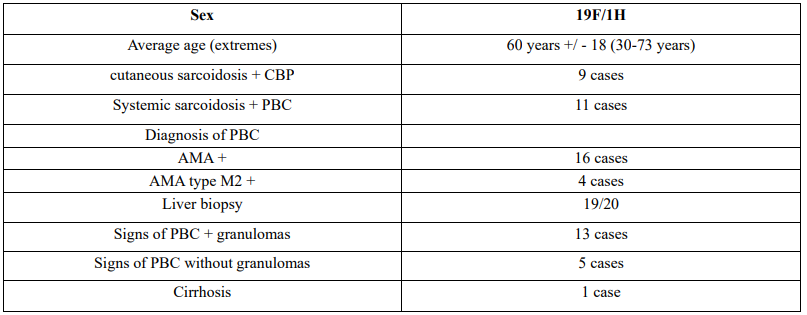
Table 1. Epidemiological characteristics of cases reported in the literature associating primary biliary cirrhosis and sarcoidosis (20 well-documented cases).
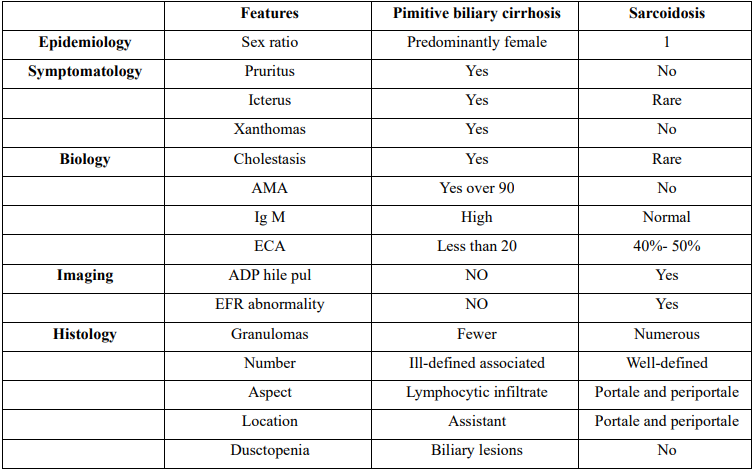
Table 2. Comparative table of characteristics of primary biliary cirrhosis and sarcoidosis
Conclusion
PBC and sarcoidosis share certain clinical, biological and histomorphological features. Their etiology remains unknown. However, their association suggests a common origin of the granuloma [1,12]. Sarcoidosis and PBC can occur concomitantly in the same patient, presenting a real diagnostic challenge. Prognosis depends on early diagnosis and treatment [13].
References
- Nourdin Aqodad, Bouchra Loukili, Salim Gallouj, Taoufik Harmouch, Afaf Amarti, et al. (2014) Association of sarcoidosis and primary biliary cirrhosis: report of a new case. Pan Afr Med J. 18: 279. [PubMed.]
- Fatima zahra aghrabi et al. (2020) Association sarcoidose et cirhose biliaire primitive: une nouvelle observation. PAMJ- Clinical medicine. 2: 13. [Ref.]
- Willis C, Maddrey Jefferson. (1983) Sarcoidosis and primary biliary cirrhosis associated disorders. Medical college philadelphia. PA 19107. N Engl J Med. 308(10): 588-590. [PubMed.]
- Baughman RP, Lower EE, du Bois R. (2003) Sarcoidosis. Lancet. 361(9363): 1111-1118. [PubMed.]
- Hriz, Moez Jallouli, Yosra Cherif, Zouhir Bahloul. (2015) Association sarcoïdose et maladie de Horton: à propos d’un cas Service de Médecine Interne, CHU 3029 Sfax,Tunisie Pan African Medical Journal. 20: 98. [Ref.]
- Sowmya Kishor, Maria L Turner, Brian B Borg, David E Kleiner and Edward W. (2008) Cutaneous sarcoidosis and primary biliary cirrhosis: A chance association or related diseases? Cowen, MD, MHScb Norfolk, Virginia) Bethesda, Maryland) and St Louis, Missouri Am Acad Dermatol. 58: 2. [Ref.]
- Kishor S, Turner ML, Borg BB, Kleiner DE, Cowen EW. (2008) Cutaneous sarcoidosis and primary biliary cirrhosis: A chance association or related diseases? Journal of the American Academy of Dermatology. 58(2): 326-335. [PubMed.]
- Jardine DL, Chambers ST, Hart DJ, Chapman BA. (1994) Primary biliary cirrhosis presenting with granulomatous skin lesions. Gut. 35(4): 564-566. [PubMed.]
- Poupon R. (2014) Cirrhose biliaire primitive. EM consulte. [Ref.]
- Lindor KD, Gershwin ME, Poupon R, Kaplan M, et al. (2009) Primary biliary cirrhosis. Hepatology (Baltimore, Md). 50(1): 291-308. [PubMed.]
- Mrabet D, Meddeb N, Sahli H, Ajlani H, Sellami S. (2006) Association cirrhose biliaire primitive et polyarthrite rhumatoïde: A propos d'une observation avec revue de la littérature. Revue du Rhumatisme. 73(10-11): 1090-1090. [Ref.]
- E B Keeffe. (1987) Sarcoidosis and primary biliary cirrhosis. Literature review and illustrative case. Am J Med. 83(5): 977-980. [PubMed.]
- Medaoud, Dj Hakem, Boudjelida H, A Hamadène, Djenane, et al. Sarcoïdose et cirrhose biliaire primitive: à propos de deux observations S. Service de médecine interne, hôpital Mohamed Lamine Debaghine, BabElOued, Alger, Algérie. [Ref.]