>Corresponding Author : Bellamine Hind
>Article Type : Case Report
>Volume : 3 | Issue : 10
>Received Date : 06 Dec, 2023
>Accepted Date : 18 Dec, 2023
>Published Date : 22 Dec, 2023
>DOI : https://doi.org/10.54289/JCRMH2300146
>Citation : Hind B, Mehdi B, Leila B, Meryem B, Mina M, et al. (2023) Myocardial Infarction During Behcet's Disease: A Case Report. J Case Rep Med Hist 3(10): doi https://doi.org/10.54289/JCRMH2300146
>Copyright : © 2023 Hind B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access
Department of internal medicine, university hospital center, Casablanca, Morocco
*Corresponding author: Bellamine Hind, Department of internal medicine, university hospital center, Casablanca, Morocco
Abstract
Behcet's disease is a multi-systemic inflammatory vasculitis of unknown etiology. Its diagnosis is based on a clinical score (international criteria’s) including oral and genital aphthosis, neurological, ophthalmological, and vascular involvement.
Cardiac involvement is a rare complication and can affect all three tunics. Coronary involvement is exceptional and can be life threatening.
We report the observation of a 38-year-old man suffering from Behcet's disease who presented a myocardial infarction related to the occlusion of the proximal anterior interventricular artery.
Keywords: Myocardial Infarction; Behcet’s Disease; Immunosuppressive Therapy; Cardiovascular Diseases; Risk Factors; Vasculitis
Introduction
Behcet's disease is a multi-systemic inflammatory vasculitis of unknown etiology, probably multifactorial, characterized by recurrent acute inflammatory attacks. Its diagnosis is based on a clinical score based on international criteria of BD including oral and genital aphthosis, neurological, ophthalmological, and vascular attacks, which are the most frequent and those that most condition the vital and functional prognosis of patients. It occurs most often in young adults and is predominantly male. It can affect vessels of all sizes (small, medium and large caliber arteries, venules, veins) in multiple organs, with a venous tropism.
Cardiac involvement during behçet's disease is a rare complication (1-6%), which can sometimes be inaugural (33%), it can concern the three tunics, and of variable expression, it can occur in the form of intracardiac thrombus, endocarditis, myocarditis, pericarditis, endomyocardial fibrosis, coronary arteritis, valvular disease and myocardial infarction. The latter is considered rare or even exceptional, the prognosis is poor, it can be life threatening, the mortality is estimated at 20%, mainly due to cardiovascular complications.
We report the case of a young patient suffering from juvenile onset Behcet's disease, who presented a myocardial infarction related to occlusion of the proximal anterior interventricular artery.
Case report
This is a 38 year old patient, with a chronic smoking habit (5 packs /year) as a cardiovascular risk factor, BMI: 23, the patient has been diagnosed with a Behçet's disease at the age of 30, which was retained in view of the presence of international clinical criteria (bipolar aphthosis that first occurred at the age of 14, pseudofolliculitis at the age of 20, bilateral posterior uveitis at the age of 30). Admitted to the emergency room on day 2 of an incapacitating infarct chest pain, an EKG was performed urgently which showed: SRR at 60 HB/min with the presence of anteroseptal and lateral ST-segment shift with a Q wave of necrosis (figure1). The diagnosis of ST+ ACS was retained, a transthoracic echocardiography was carried out systematically and showed a dilated cardiomyopathy of probably ischemic origin with segmental kinetic disorders such as akinesia, involving the territory of the anterior interventricular AIV (LVEF at 35%). A diagnostic coronary angiography had shown an acute occlusion of the proximal AIV (figure2). Blood tests showed elevated troponins (1162ng/l). The search for risk factors of atherosclerosis was negative: GAJ: 0.96g/l, lipid profile: normal (total cholesterol: 1.6g/l, HDL: 0.5g/l, LDL: 1g/l, TG: 0.66g/l). Tests for constitutional and acquired thrombophilia including antiphospholipid antibodies, protein S, protein C, antithrombin III, Factor V and Factor II were negative, the hemostasis parameters were normal, as well as the search for a immunological disorders was negative, the tests for infectious etiologies including syphilitic serology, HIV, viral hepatitis and Tuberculosis were negative. The treatment of myocardial infarction in acute phase was quickly instituted, the patient benefited from a conventional treatment of his ischemic cardiopathy with installation of a stent, oral BASIC treatment (Beta blockers, platelet antiaggregant, statins and calcium channel blockers and anticoagulation), associated with the treatment of Behçet deseas consisting of corticotherapy (methylprednisolon) in infusion 1g/d for 3 days, an immunosuppressive type azathioprine at dose of 150mg/d was also administered, colchicine for the bipolar aphtosis at a dose of 1mg/d and the tobacco withdrawal. The evolution was good, notably a stability of the vasculitis, after the treatment the patient remained asymptomatic on the cardiac functional level. We retained the diagnosis of myocardial infarction linked to Behçet's disease.
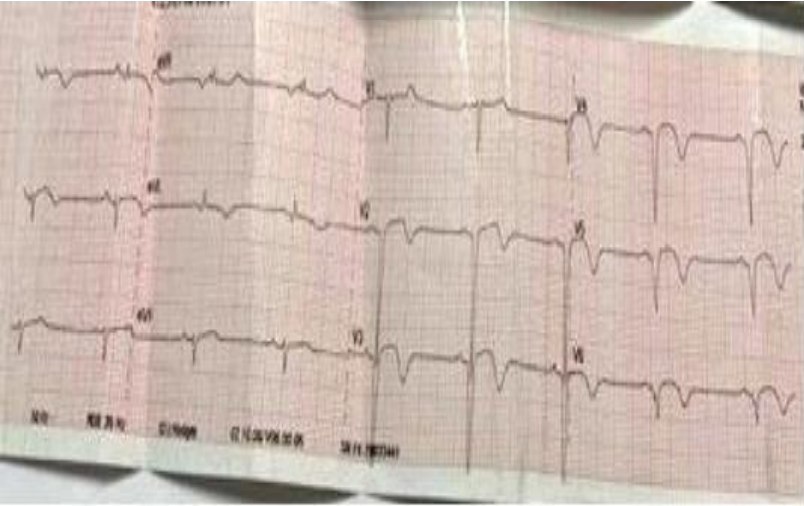
Figure 1. SRR at 60 HB/min with the presence of anteroseptal and lateral ST-segment shift with a Q wave of necrosis.

Figure 2. coronary angiography showing complete occlusion of the anterior interventricular artery.
Discussion
Cardiac involvement in Behçet's disease is one of the rarest, accounting for around 6% of cases in different series; it can affect all three tunics, dominated by pericarditis, and rarely myocardial infarction, the last being a rare and fatal complication of Behçet's disease [1]. On average, some thirty cases have been reported in the literature [2].
Pathophysiologically, Behcet's disease is distinct from other vasculitides in that arteries and veins of different calibres are involved. Arteries are affected by the perivascular and endovascular inflammatory process, resulting in a unique spectrum of stenosis, thrombotic obstruction, bleeding and aneurysms. Cardiac involvement manifests principally by coronary arteritis, myocardial infarction and aortic insufficiency. On the other hand, fibrous intimal thickening can cause acute myocardial infarction despite angiographically normal coronary arteries. And some literature data suggest that such altered microvascular function is the cause of coronary events in these patients.
Its prevalence varies from < 0.5% to 2% of cases according to the different behçet series, it is rarely inaugural, and occurs after an estimated average delay of 4.7 years from the onset of the disease [3]. In our patient, coronary involvement occurred 24 years after the onset of the disease, which is not in accordance with the data in the literature.
Coronary disease most often affects young subjects with no cardiovascular risk factors other than smoking, and can manifest as myocardial infarction or angina, as in our patient's case. Coronary angiography may reveal stenosis, occlusion or aneurysm without associated atheromatous lesions [1].
In one cohort, 85% of coronary patients were symptomatic, as was the case with our patient who presented with disabling infarct pain. Coronary involvement in Behcet's disease is frequently monotruncular and proximal, and particularly affects the AIV [4]. Our patient's profile is perfectly in accord with this literature.
Atherosclerosis is the leading cause of myocardial infarction, but Behcet's disease remains one of the etiologies classified as a non-atheromatous cause [5]. In our patient, the absence of atheromatous lesions, both coronary and extracoronary, suggests the potential role of Behcet's disease in the genesis of the coronary damage responsible for myocardial infarction.
The therapeutic management of coronary arterial lesions remains singularly problematic, as it confronts the clinician with a double challenge with two essential facets that are inseparable and complementary: Ensuring adequate, rapid and aggressive treatment in the acute phase of the coronary syndrome, and proposing a pathophysiological fundamental treatment of the causing disease, the only guarantee of effective prevention of recurrences. In practice, the 2018 EULAR recommendations clearly established the systematic use of immunosuppressive agents as first-line treatment in combination with glucocorticoids in severe arterial disease in Behçet's disease, in order to limit the progression of this veritable inflammatory coronary disease; Combined with double platelet anti-aggregation, based on acetylsalicylic acid and clopidogrel, which should be maintained for as long as possible in the coronary patient [6-8].
In our patient, we initiated intravenous boluses of corticosteroid therapy, followed by oral relay, combined with azathioprine.
As for prognosis, arterial and cardiac involvement is undeniably poor prognostic factors associated with an increased risk of mortality [9].
The remission rate is higher in patients with pericarditis, while myocardial infarction is a poor prognostic factor. And in order to improve it, this requires early diagnosis and intensive treatment to avoid fatal evolution. A comparative univariate study based on the various observations published in the literature showed that the evolution was better in the group of patients who received corticosteroid therapy and immunosuppressive agents. These findings support the use of these two therapeutic classes in the coronary involvement of Behçet's disease [5].
Conclusion
Myocardial infarction is a rare but serious complication of Behcet's disease, and should be considered in all young, symptomatic patients with no cardiovascular risk factors. Asymptomatic forms of the disease may also be possible, prompting screening for primary prevention of coronary damage in Behcet's disease. Corticosteroid therapy combined with immunosuppressive agents is the cornerstone of treatment for coronary damage in Behcet's disease, in addition to conventional treatment of coronary artery disease, and keep in mind the strict adherence to treatment.
No Conflict of interest.
References
- AC Desbois, B Wechsler, P Cluzel. (2014) Atteintes cardiovasculaires de la maladie de Behçet. 12: 2. [Ref.]
- Sarica, et al. (2006) Vascular involvement in Behçet's disease: a retrospective analysis of 2319 cases. Int J Dermatol. 45(8): 919-921. [PubMed.]
- Unsal Vural, Mehmet Kizilay, and Ahmet Arif Aglar. (2019) Coronary Involvement in Behçet's Disease: what are its Risks and Prognosis? (Rare Cases and Literature Review). 34(6): 749-758. [Ref.]
- Chen H, Zhang Y, Li C, Wu W, Liu J, et al. (2019) Coronary involvement in patients with Behçet's disease. Clin Rheumatol. 38(10): 2835-2841. [PubMed.]
- FA Benaich, A Ben, El Mekkki, H Benjelloun, Z Lakhal. (2015) Infarctus Du Myocarde Revelant La Maladie De Behçet. A Propos D’un Cas, Journal Marocain des Sciences Médicales Tome XX) N. [Ref.]
- Hatemi G, Christensen R, Bang D, Bodaghi B, Celik AF, et al. (2018) update of the EULAR recommendations for the management of Behçet's syndrome. Ann Rheum Dis. 77(6): 808-818. [PubMed.]
- Selami Demirelli. (2015) Husnu Degirmenci Sinan Inci and Arif Arisoy: Cardiac manifestations in Behcet's disease. 4(2): 70-75. [Ref.]
- F Othmani. (2009) Behçet’s disease: new therapeutics. The journal of internal medicine. 30: 243-252. [PubMed.]
- Saadoun D, Wechsler B, Desseaux K, Le Thi Huong D, Amoura Z, et al. (2010) Mortality in Behcet’s disease. Arthritis Rheum. 62: 2806-2812. [PubMed.]