>Corresponding Author : Mehdi Belhakim
>Article Type : Case Report
>Volume : 4 | Issue : 1
>Received Date : 22 Dec, 2023
>Accepted Date : 09 Jan, 2024
>Published Date : 12 Jan, 2024
>DOI : https://doi.org/10.54289/JCRMH2400103
>Citation : Ettagmouti Y, Belhakim M, Ettachfini T and Habbal R. (2024) Thrombotic Recurrence Under New Oral Anticoagulants Revealing Antiphospholipid Antibody Syndrome: Case Report. J Case Rep Med Hist 4(1): doi https://doi.org/10.54289/JCRMH2400103
>Copyright : © 2024 Ettagmouti Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access
Cardiology department, University Hospital Ibn Rochd, University Hassan II, Casablanca, Morocco
*Corresponding author: Mehdi Belhakim, Cardiology department, University Hospital Ibn Rochd, University Hassan II, Casablanca, Morocco
Abstract
Introduction and importance: Non-vitamin K antagonist Oral Anti-Coagulants (NOACs) have emerged as an effective treatment for thromboembolic events with a reduced bleeding risk compared to traditional anti-vitamin K drugs. However, their role in managing antiphospholipid antibody syndrome remains a subject of debate.
Case presentation: We present the case of a 48-year-old man with a history of pulmonary embolism and a right cavitary thrombus, who was receiving treatment with a new-generation anticoagulant. Despite this treatment, he exhibited resistance, prompting further investigation that led to the diagnosis of antiphospholipid antibody syndrome.
Clinical discussion: Our clinical case highlights the importance of routinely screening for antiphospholipid syndrome, especially when it coexists with lupus, due to the potential ineffectiveness of NOACs.
Conclusion: This case underscores the necessity of considering alternative treatment strategies in individuals with antiphospholipid antibody syndrome, particularly when traditional anticoagulants prove inadequate, even when lupus is concurrent.
Keywords: Non-Vitamin K Antagonist Oral Anti-Coagulants; Antiphospholipid Antibody Syndrome; Thrombotic Recurrence; Case Report
Abbreviations: NOAC: Antagonist Oral Anti-Coagulants, APS: Antiphospholipid Antibody Syndrome, INR: Index National Ratio, LV: Left Ventricle
Introduction
Non-vitamin k antagonist Oral Anti-Coagulants (NOACs) represent a new class of anticoagulants that offer patients a simpler daily life with less complicated monitoring [1]. They have demonstrated their efficacy in the treatment and prevention of thromboembolic events while decreasing the risk of bleeding compared to anti-vitamin K (VKA) drugs [2]. Patients with venous thromboembolic disease secondary to antiphospholipid antibody syndrome (APS) require lifelong treatment with wafarin with an index national ratio(INR) target of 2 to 3. The hope of a therapeutic alternative has recently increased with the arrival of NOACs, however several clinical cases reported in the literature have objectified a thrombotic recurrence in patients treated with NOACs in the context of APS.
This is a case of a 48-year-old Moroccan man, followed for pulmonary embolism under well-conducted NOACs treatment, who developed a right atrial thrombus revealing a secondary APS.
Patient and observation
We report a case of a 48-year-old Moroccan patient, followed for a scleroderma-lupus overlap syndrome complicated by pulmonary fibrosis for 3 years on mycophenolate mofetil. The patient presented a pulmonary embolism for 2 months treated with rivaroxaban 20mg/day with good compliance. He was admitted to the emergency room with right heart failure and oedemato-ascitic syndrome that had been evolving for 1 month prior to his admission, in a context of apyrexia and preservation of his general condition. The clinical examination on admission revealed a patient with respiratory distress, respiratory rate of 30cpm and saturation of 88% in free air, bilateral lower limb oedema reaching the ankles and moderate ascites with jugular vein turgor. He was hemodynamically stable with an arterial pressure of 110/70 mmHg and a heart rate of 95beats per minutes. The rest of the clinical examination showed signs in favor of his overlap syndrome. The EKG performed shows a complete right bundle block with S1Q3 and secondary repolarization disorders (Figure 1).
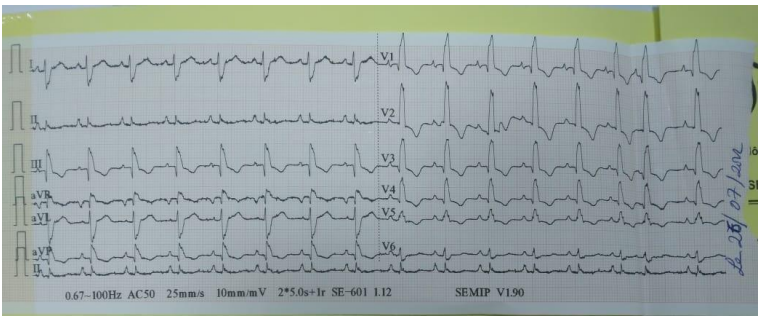
Figure 1. Complete right bundle block on EKG
On echocardiography, we found a very dilated right ventricle (basal diameter = 51 mm, right ventricle/left ventricle (LV) ratio >1), crushing the LV, hypertrophied (free wall = 7mm) in longitudinal systolic dysfunction (systolic excursion of the tricuspid annulus at 14mm). The right atrium was dilated, with echogenic material attached to its floor, serpiginous, very mobile (Figure 2).

Figure 2. Arrow represent mobile serpiginous thrombus in the right atrium
Severe tricuspid insufficiency due to coaptation failure of the tricuspid cusps, estimating systolic pulmonary arterial pressures at 60mmHg. The biological workup showed positive ultrasensitive troponins at 132ng/l, the ionogram and the blood count were without particularities. The SAPL workup showed the presence of circulating lupus-type anticoagulant antibodies, and the level of anti-cardiolopin and anti-B2 glycoprotein antibodies was high.
Management was hospitalization in a cardiac intensive care unit, oxygen therapy weaned after 3 days. The NOACs were stopped and replaced by low-molecular-weight heparin at a curative dose of 0.6, 1 subcutaneous injection twice a day. Treatment with VKAs was started as soon as APS was confirmed, combined with a low dose of loop diuretics. Immunosuppressive therapy was continued.
Evolution after one week was favorable, clinically by regression of edema, ascites and improvement of respiratory function and echographically by improvement of right ventricular systolic function (systolic excursion of the tricuspid annulus to 18mm) and a decrease of pulmonary arterial pressure values to 30 mmHg. The patient was declared discharged with follow-up in the cardiology department and internal medicine. At the last check-up 2 months after the pulmonary embolism, there was a disappearance of the intracavitarythrombus which responded well to VKA treatment.
Discussion
APS is an autoimmune disease characterized by the occurrence of venous or arterial thromboembolic events and/or obstetrical complications (repeated miscarriages and/or later complications of pregnancy), and the presence, on at least two occasions, three months apart, of antibodies called antiphospholipid antibodies (lupus-type circulating anticoagulant, anti-beta2-glycoprotein antibodies, anticardiolipin antibodies) [3]. VKAs represent the mainstay of long-term anticoagulant treatment of thromboembolic events secondary to APS with an INR target of 2 to 3 [4]. The new oral anticoagulants include dabigatran, rivaroxaban, apixaban and edoxaban . These agents have the advantage of few erdietary and drug interactions than wafarin, which facilitates patient monitoring, in addition to their efficacy, which has been demonstrated in large clinical trials [5,6]. However, the use of OADs in this indication has been questioned following several cases of therapeutic failure and thromboembolic recurrence [7]. In a review of the literature published by Dufrostin 2016, out of 122 cases of APS under NOACs, 19 developed thrombotic recurrences, particularly in cases of positivity of the three antibodies [8]. Signorelli also published a series of 8 cases of thrombotic recurrence in patients put on rivaroxaban following an APS, concluding that NOACs should not be recommended for patients with APS [9]. Win and Rodgers reported 3 cases of thrombotic recurrence on rivaroxaban and dabigatran following an APS.
These studies are consistent with the case of our patient who presented an embolic recurrence with an intra-OD thrombus under well-conducted NOAC treatment with a positive lupus circulating anticoagulant in the SAPL work-up.
In contrast, the RAPS clinical trial comparing rivaroxaban with VKA in thrombotic events secondary to APS with or without systemic lupus erythematosus concluded that rivaroxaban was not inferior to VKA [11]. This study was criticized by Dufrost because the number of patients did not allow for statistically significant results and also because there were not enough high-risk patients defined by the positivity of the three antibodies, the presence of arterial thrombosis, or recurrent venous thrombosis.
The ineffectiveness of NOACs compared to VKAs in this indication may be explained by the fact that VKAs work by inhibiting several factors in the coagulation cascade, and in patients with APS who have triplepositive antibodies or very high concentrations of antibodies, inhibition of a single factor may not be effective [7].
Conclusion
The use of direct oral anticoagulants in the treatment of thromboembolic events in patients with APS should be avoided, given the number of thrombotic recurrences reported in the literature. Our clinical case supports these results, and also to remind the interest of systematically searching for APS in lupus patients with thrombotic disease.
Declarations
Ethical approval: Written informed consent was obtained from the patient described in this article.
Funding: No funding has been received to carry out the work described in this manuscript.
Disclaimers or conflict of interest: None
References
- Darius H. (2017) NOAK: Real-life-Daten und Therapie von Blutungen mit Antidots. Medizinische Klinik-Intensivmedizin und Notfallmedizin. 2(112): 99‑104. [Ref.]
- Altiok E, Marx N. (2018) Oral Anticoagulation: Update on Anticoagulation With Vitamin K Antagonists and Non–Vitamin K–Dependent Oral Anticoagulants. Deutsches Ärzteblatt International. 115(46): 776-783. [Ref.]
- Miyakis S, Lockshin MD, Atsumi T, Branch DW, Brey RL, et al. (2006) International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). Journal of thrombosis and haemostasis. 4(2): 295‑306. [PubMed.]
- Kearon C, Akl EA, Comerota AJ, Prandoni P, Bounameaux H, et al. (2012) Antithrombotic therapy for VTE disease: antithrombotic therapy and prevention of thrombosis: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 141(2): e419S-e496S. [PubMed.]
- Khoo CW, Lip GY. (2009) Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 361: 1139-1151. [PubMed.]
- Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, et al. (2011) Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. New England Journal of Medicine. 365(10): 883‑891. [PubMed.]
- Joshi A, Hong J, Siva C. Recurrent thrombosis in patients with antiphospholipid syndrome receiving newer oral anticoagulants: a case report and review of literature. Clinical Medicine & Research. (2017) 15(1‑2): 41‑44. [Ref.]
- Dufrost V, Risse J, Zuily S, Wahl D. (2016) Direct oral anticoagulants use in antiphospholipid syndrome: are these drugs an effective and safe alternative to warfarin? A systematic review of the literature. Current rheumatology reports. 18: 1‑8. [PubMed.]
- Signorelli F, Nogueira F, Domingues V, Mariz HA, Levy RA. (2016) Thrombotic events in patients with antiphospholipid syndrome treated with rivaroxaban: a series of eight cases. Clinical rheumatology. 35: 801‑805. [PubMed.]
- Win K, Rodgers GM. (2014) New oral anticoagulants may not be effective to prevent venous thromboembolism in patients with antiphospholipid syndrome. American Journal of Hematology. 89(10): 1017‑1017. [PubMed.]
- Cohen H, Hunt BJ, Efthymiou M, Arachchillage DR, Mackie IJ, et al. (2016) Rivaroxaban versus warfarin to treat patients with thrombotic antiphospholipid syndrome, with or without systemic lupus erythematosus (RAPS): a randomised, controlled, open-label, phase 2/3, non-inferiority trial. The Lancet Haematology. 3(9): e426‑436. [PubMed.]