>Corresponding Author : Apoorva Kumar Pandey
>Article Type : Case Report
>Volume : 4 | Issue : 2
>Received Date : 09 Jan, 2024
>Accepted Date : 19 Jan, 2024
>Published Date : 24 Jan, 2024
>DOI : https://doi.org/10.54289/JCRMH2400107
>Citation : Manhas A, Pandey AK, Ahmed S, Bhardwaj A and Anjum F. (2024) Successful Preservation of the Facial Nerve in Parotid Surgery for Huge Pleomorphic Adenoma of the Deep Lobe. A Case Report. J Case Rep Med Hist 4(2): doi https://doi.org/10.54289/JCRMH2400107
>Copyright : © 2024 Manhas AN, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access
1Senior Resident, Department of ENT and Head-Neck surgery, Sri Guru Ram Rai Institute of Medical and Health Sciences, Patel Nagar, Dehradun, 248001, Uttarakhand, India
2Professor, Department of ENT and Head-Neck Surgery, Sri Guru Ram Rai Institute of Medical and Health Sciences, Patel Nagar, Dehradun, 248001, Uttarakhand, India
3Assistant professor, Department of Pathology, Sri Guru Ram Rai Institute of Medical and Health Sciences, Patel Nagar, Dehradun, 248001, Uttarakhand, India
4Professor, Department of Pathology, Sri Guru Ram Rai Institute of Medical and Health Sciences, Patel Nagar, Dehradun, 248001, Uttarakhand, India
*Corresponding author: Apoorva Kumar Pandey, Professor, Department of ENT and Head-Neck Surgery, Sri Guru Ram Rai Institute of Medical and Health Sciences, Patel Nagar, Dehradun, 248001, Uttarakhand, India
Abstract
Pleomorphic adenoma, also known as benign mixed salivary gland tumor, is the most common salivary gland tumor accounting for about 50-74 percent of all parotid neoplasms that has a slight female predilection in the 4th to 5th decade of life. The treatment of choice for this tumor is complete surgical removal. When the tumor arises from the superficial lobe of the parotid gland, superficial parotidectomy is recommended with facial nerve preservation and if the tumor involves the deep lobe, in that case, it may be necessary to perform total parotidectomy with identification and preservation of the facial nerve. Here we are presenting a case of parotid (deep lobe) pleomorphic adenoma where we successfully preserved and identified the facial nerve with the complete removal of the tumor.
Keywords: Pleomorphic Adenoma; Deep Lobe of Parotid Gland; Parotidectomy; Facial Nerve
Abbreviations: CT: Computed Tomography
Introduction
Salivary gland tumors are not so common, they represent less than 4 percent of head and neck neoplasms [1]. Pleomorphic adenoma also known as benign mixed salivary gland tumor is the most commonly encountered tumor which affects the salivary glands accounting for about 50-74 percent of all parotid neoplasms [2]. They mostly arise in the superficial lobe but rarely also involve the deep lobe of the parotid gland. Its incidence is reported to be 2.4-3.05/1 lakh annually and it has a slight female predilection [3]. Even in children also pleomorphic adenoma is the most common salivary gland tumor. During deep lobe surgery, it is of paramount importance to correctly identify and preserve the facial nerve to achieve better outcomes. The facial nerve is prone to get affected not only due to inadvertent transection but also due to stretching, use of cautery in nearby space, and also for unknown reasons. The sound knowledge of facial nerve course and the ways to localise, identify and preserve it forms the basis of a successful parotid surgery which is nonetheless a learning curve for all surgeons. Here we are presenting a case of deep lobe surgery where the facial nerve was beautifully preserved.
Case Report
A 40-year-old female patient was reported with the chief complaint of painless swelling on the right side of the face just below the right ear for the last 5 years. It was insidious in onset with slowly increasing in size. There was a history of mild discomfort to palpation. There was no history of difficulty in chewing, difficulty in opening mouth, fever, weight loss, or symptoms like ear pain.
On local examination, there was an external swelling around 6 x 5 cm in size extending from just in front of the tragus up to 1 cm below the angle of the mandible inferiorly and from the anterior border of sternocleidomastoid muscle posteriorly to 2 cm in front of angle of mandible over the mandibular ramus anteriorly. Facial symmetry was present and facial nerve examination was normal. On palpation, the swelling was firm in consistency, non-tender, mobile and non-fluctuant. Intraoral examination was normal. Bilateral level II lymph nodes were palpable. Fine needle aspiration cytology revealed pleomorphic adenoma of the right parotid gland.
Contrast-enhanced CT of the neck revealed approximately 59 (AP) x 36 ( TR) x 55 (CC) mm sized heterogeneously enhancing iso- to mildly hyperdense space-occupying lesion in right parotid gland involving superficial as well as deep lobe likely suggestive of pleomorphic adenoma. The lesion was confined within the gland capsule with no extra glandular extension (Figure no 1).
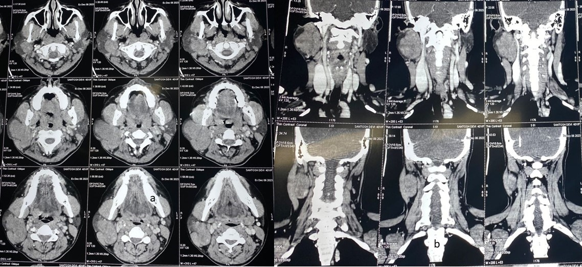
Figure 1. CECT [a (axial ) & b (coronal) cuts] showing heterogeneously enhancing iso- to a mildly hyperdense lesion in the right parotid gland involving superficial and deep lobes and the swelling is confined within the gland capsule.
Based on the above findings surgical planning of total conservative parotidectomy by transcervical approach was made. Under General Anesthesia, a modified Blair’s incision was given, and the greater auricular nerve was identified and sacrificed. Superficial parotidectomy was done first with localization, identification and delineation of the facial nerve branches, and then by mobilizing the facial nerve branches, the tumor of the deep lobe of the parotid gland was dissected and removed (Figure no 2(a-d).
Hemostasis was achieved and irrigation of the surgical wound was done. Suturing was done in 2 layers. Facial nerve examination was done immediately after the patient was extubated which revealed House Brackmann Grade II facial nerve palsy with slight mouth deviation and the patient was put on intravenous steroid (Figure no 3).
Sutures were removed on the 8th postoperative day. Histological analysis showed pleomorphic adenoma of the parotid gland (Figure no 4). After one-month post-operative follow-up patient’s facial function improved but still, some weakness on mouth opening is there. She is taught to do facial exercises for recovery.

Figure 2. a)Image showing swelling of parotid gland after elevating SMAS flap. b) localization of facial nerve trunk. c) after elevating superficial lobe and retracting facial nerve, tumour involving deep lobe is visible. d) excision of superficial lobe and deep lobe tumour. Facial nerve branching pattern is visible.

Figure 3. a) Immediate postoperative period (grade II H& B). b&c) after one month, complete eye closure and slight mouth deviation on smiling.
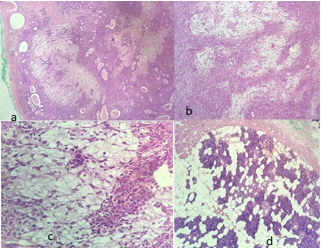
Figure 4. a) well-circumscribed encapsulated multinodular lesion showing proliferation of both epithelial and stromal components (H&E, X10), b) sheets, nests and cords of epithelial cells admixed with myoepithelial cells separated by myxoid stroma (H&E, X10), c) Round to oval epithelial cells admixed with spindle to plasmacytoid myoepithelial cells with intervening myxoid stroma (H&E, X40), d) surrounding normal salivary gland parenchyma (H&E, X10).
Discussion
Pleomorphic adenoma is the most frequent benign neoplasm involving the parotid gland. It involves the right-sided gland more commonly than the left side with female preponderance (female to male ratio of 2:1) [4]. It can affect all age groups but occurs more commonly in the 4th to 5th decade of life [5].
The clinical case described in our study validates the epidemiological profile of the patients reported in the literature. Pleomorphic adenoma less commonly involves the submandibular gland accounting for 10 percent and very rarely the sublingual glands accounting for only 1 percent [6].
It is mandatory to do diagnostic imaging such as computed tomography (CT) or an MRI of the patient. An ultrasound (USG) can also be useful as it helps in the assessment of the consistency of the lesion but in these cases, MRI is preferred because of its better delineation of the soft tissues and precise information about tumor margins as well as the relationship of the tumor with the surrounding structures [7]. The deep lobe can be easily assessed with CT as it can be seen as a part of the parotid which lies deep to the retromandibular vein [8]. FNAC should be done after the diagnostic imaging as it helps in choosing the better surgical approach and to exclude a vascular lesion [9].
Despite being the most common benign neoplasm of the parotid gland, it has a high recurrence rate because of the few symptoms complained by the patient and its extension into the parapharyngeal space where it grows for a long time before a diagnosis is made [10]. Recurrence is mainly seen in those patients where there is focal absence of the capsule that often surrounds the tumors, with microscopic projections of the tumor into the surrounding parotid gland or where there occurs rupture of the capsule during surgery of the tumor [11]. Simple enucleation thus increases the chances of recurrence as these projections can be left behind during the procedure. Removal of the affected lobe is thus necessary [12]. The treatment of choice for this tumor is complete surgical removal. When the tumor arises from the superficial lobe of the parotid gland, superficial parotidectomy is recommended with facial nerve preservation and if the tumor involves the deep lobe, in that case it may be necessary to perform total parotidectomy [13]. The patients need to be informed about the risk of the facial nerve injury during surgery since lesions of one or both lobes require more manipulation which can lead to injury of the facial nerve. Because of significant morbidity due to facial nerve paresis, it is pertinent to provide patients with the best possible information preoperatively. Another complication that can be seen is Frey’s syndrome which presents as sweating and redness in the parotid region where secretomotor fibers of the auriculotemporal nerve join with the greater auricular nerve and reach sweat glands of facial skin [14].
As there are rare chances of pleomorphic adenoma to turn into a malignancy, it occurs more frequently in patients with long-standing masses. The risk of transformation to malignancy within the first 5 years is 1.5% which increases to 10% if the tumor remains there for more than 15 years [15]. Although this is a benign tumor but periodic monitoring and evaluation for a postoperative period of 5 years is important due to its recurrence [16]. As of now the patient is in a month post-operative period with no signs of any significant morbidity.
Conclusion
Pleomorphic adenomas though rare, most commonly occur in the parotid gland. A definite diagnostic plan should be made for its proper diagnosis and management. Identification of the parotid tumors with the help of ultrasound and ruling out deep lobe involvement with a CT or MRI should be done for better preoperative planning of surgical removal of the tumor and reduction in the chances of postoperative complications and recurrence. A correct and methodical approach toward localization, identification and preservation of facial nerve is warranted for better surgical outcomes. Complete removal, identification and preservation of facial nerve, and preventing recurrences in the long term are the cornerstones of benign parotid tumor surgery.
Declarations
Funding: none
Compliance with ethical standards: Yes
Conflict of interest/competing interests: All authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics approval: All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to participate: Informed consent was obtained from all individual participants in the study.
Consent for publication: Yes
Author’s contributions
A K Pandey - concept, literature search, manuscript preparation, and editing
Arun N Manhas, Fatma Anjum- manuscript writing, acquisition of data
Aparna Bhardwaj, Saqib Ahmed - Pathological correlate, manuscript review
All authors read and approved the final manuscript.
Acknowledgement: None
References
- Datarkar AN, Deshpande A. (2015) Giant Parapharyngeal Space Pleomorphic Adenoma of the Deep Lobe of Parotid Presenting as Obstructive Sleep Apnoea: A Case Report & Review of the Diagnostic and Therapeutic Approaches. J Maxillofac Oral Surg. 14(3): 532-537. [PubMed.]
- Auclair PL, Eillis GL, Gnepp DR, et al. (1991) Salivary gland neoplasms: General considerations. In: Ellis GL, Auclair PL, editors. Surgical pathology of the salivary glands, 1st ed. Philadelphia, PA: Saunders. 135-164. [Ref.]
- Barnes L, Eveson JW, Reichart P, et al. (2005) Pathology and genetics of head and neck tumours. Lyon: IARC. [Ref.]
- Silva SJ, Costa GT, Brant AC, et al. (2006) Metachronous bilateral pleomorphic adenoma of the parotid gland. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 101(3): 333-338. [PubMed.]
- Kizil Y, Aydil U, Ekinci O, et al. (2013) Salivary gland tumors in Turkey: demographic features and histopathological distribution of 510 patients. Indian J Otolaryngol Head Neck Surg. 65(Suppl 1): 112-120. [PubMed.]
- Hakeem AH, Hazarika B, Pradhan SA, et al. (2009) Primary pleomorphic adenoma of minor salivary gland in the parapharyngeal space. World J Surg Oncol. 7: 85. [Ref.]
- Seok J, Hyun SJ, Jeong WJ, et al. (2019) The Difference in the Clinical Features Between Carcinoma ex Pleomorphic Adenoma and Pleomorphic Adenoma. Ear Nose Throat J. 98(8): 504-509. [PubMed.]
- Gozzi G, Di Bonito, Bazzouli M. (1990) Malignant tumors clinical use of Computed tomography. J Computed Assisted tomography. 20: 444-447. [Ref.]
- Sergi B, Contucci AM, Corina L, et al. (2004) Value of fine-needle aspiration cytology of parotid gland masses. Laryngoscope. 114(4): 789. [PubMed.]
- Izzo L, Frati R, Cianfrone F, et al. (2004) Parotid gland cancer: a case report of a primitive adenocarcinoma arising from a multirecurrent pleomorphic adenoma. J Exp Clin Cancer Res. 23: 153-156. [PubMed.]
- Mantsopoulos K, Muller S, Agaimy A, et al. (2017) Extracapsular dissection in the parapharyngeal space: benefits and potential pitfalls. Br J Oral Maxillofac Surg. 55(7): 709-713. [PubMed.]
- Ayoub OM, Bhatia K, Mal RK. (2002) Pleomorphic adenoma of the parotid gland: is long-term follow-up needed? Auris Nasus Larynx. 29(3): 283-285. [PubMed.]
- Dombrowski ND, Wolter NE, Irace AL, et al. (2019) Pleomorphic adenoma of the head and neck in children: presentation and management. Laryngoscope. 129(11): 2603-2609. [PubMed.]
- Bonavolonta P, Orabona G, Maglitto F, et al. (2019) Postoperative complications after removal of pleomorphic adenoma from the parotid gland: A long-term follow up of 297 patients from 2002 to 2016 and a review of publications. Br J Oral Maxillofac Surg. 57(10): 998-1002. [PubMed.]
- Seifert G. (1992) Histopathology of malignant salivary gland tumours. Eur J Cancer B Oral Oncol. 28B(1): 49-56. [PubMed.]
- Pereira DA, Campos E, Bonatto M, et al. (2021) Conservative Surgical Approach to Pleomorphic Adenoma in Parotid Gland: Case Report. J. Health Sci. 23(2): 121-125. [Ref.]