>Corresponding Author : Mohammad Pishgahi
>Article Type : Original Research Article
>Volume : 4 | Issue : 4
>Received Date : 12 Feb, 2024
>Accepted Date : 23 Feb, 2024
>Published Date : 27 Feb, 2024
>DOI : https://doi.org/10.54289/JCRMH2400117
>Citation : Yazd H, Ohadi L, Abdolmaleki M, Farsi Y and Pishgahi M. (2024) The Effect of Pharmacist Interventions on the Antimicrobial Prevention Pattern in Vascular and Gastrointestinal Surgeries: A Prospective Study. J Case Rep Med Hist 4(4): doi https://doi.org/10.54289/JCRMH2400117
>Copyright : © 2024 Yazd H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Research Article | Open Access
1School of Pharmacy, Shahid Beheshti University of Medical Sciences, Tehran, Iran
2School of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran
3Department of General Surgery, Taleghani Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran
*Corresponding author: Mohammad Pishgahi, Department of General Surgery, Taleghani Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Abstract
Introduction: Surgical site infections (SSIs) are common postoperative complications, necessitating effective preventive strategies such as pharmacist interventions. This study explores the impact of pharmacist interventions on the antimicrobial prophylaxis model in vascular and gastrointestinal surgeries.
Methods: We enrolled 200 adult postoperative patients, dividing them into two groups of 100 each. Initially, both groups received antibiotics based on surgeons' recommendations. Subsequently, all participants underwent pharmacist consultations. The first group continued antibiotics per surgeons' guidance, while the second group followed pharmacists' recommendations. We then compared SSI incidence between the two groups, recording data in an SPSS file.
Results: Initially, surgeons prescribed prophylactic antibiotics for 71% of the first group and all of the second group. Pharmacist interventions revealed inaccuracies in antibiotic type, dosage, or duration in 80% and 88% of cases, respectively. The second group better adhered to recommended guidelines for treatment duration (P=0.007), accurate dosage (P=0.0001), and re-administration necessity. Moreover, SSI occurrence significantly decreased in the second group (P=0.0001).
Conclusion: Pharmacist interventions play a critical role in reducing SSI incidence. Further research is needed to elucidate pharmacists' roles in decreasing postoperative infections and complications and establishing guidelines for their presence in surgical wards.
Keywords: Surgical Site Infection (SSI); Pharmacist Intervention; Pharmacology; Prophylaxis; Antibiotic
Abbreviations: SSI: Surgical Site Infection, CMS: Centers for Medicare and Medicaid Services, CDC: Centers for Disease Control and Prevention, ICC: Interclass Correlation Coefficient, AVF: Arteriovenous Fistula
Introduction
Surgical site infection (SSI) is one of the most widespread nosocomial infections induced by various types of surgeries with the incidence rate of 500,000 annually [1]. This complication typically occurs within the first 30 days following any surgical procedures and increases the length of hospital stay, costing the healthcare system nearly $2 billion annually [1,2]. As a result, the demand for preventing this type of infection became crucial [1]. Therefore, in 2002, the Centers for Medicare and Medicaid Services (CMS), in collaboration with the Centers for Disease Control and Prevention (CDC), designed and executed the SSI prevention initiative. Their goal was to offer evidence-based practical measures for selecting the most appropriate type of prophylactic antibiotic, dosage, and avoidance of unnecessary antibiotic administration in patients undergoing clean-contaminated surgery. Then, the Surgical Care Improvement Project (SCIP) was created in 2003 by the CMS, CDC, and ten other national organizations in the United States to minimize the SSI incidence by prescribing preoperative antibiotics [3,4]. This project recommended administering prophylactic antibiotics within half to one hour before the first incision and discontinuing antibiotics within 24 hours of surgery (within 48 hours for cardiac surgery) [5]. Despite all of these recommendations, several studies demonstrated that CDC-approved procedures which aim to reduce the incidence of SSI, are not routinely implemented. Based on these studies, only 55.7% of the operated patients receive prophylactic antibiotics within half to one hour before the initial surgical incision, and only 40.7% of them completed antibiotics regimen within 24 hours following the surgery [6]. Other studies revealed that about 80 to 90% of patients who have undergone surgery have had antimicrobial prophylaxis, but only 25 to 50% of them have the proper antimicrobial regimen, accurate time of administration, suitable duration of prophylaxis, or the precise dose of medication [7,8].
Therefore, other novel guidelines were formed to avoid this significant adverse effect including skin preparation before surgery, using surgical film on the skin of the surgical site, the norms of proper sanitation of the environment, dressing the surgical site, and the presence of the clinical pharmacist in surgical wards [9,10,11].
As SSI inflict significant financial and human resource harm and the death of many patients, in this study, we investigated the impact of pharmacist interventions as a controlling pathway on the pattern of antimicrobial prophylaxis in vascular or gastrointestinal surgery at a medical and educational hospital. We aim to recommend rules for the presence of pharmacists in surgical departments.
Methods
Study design and patients
A prospective study was designed and conducted in collaboration with Ayatollah Taleghani Medical and Educational Hospital (Tehran, Iran). We explained the aim and steps of the study for all eligible patients and obtained a written informed consent for study participation and publications from them. Ethic approval was taken by the research ethics committee of Shahid Beheshti University of Medical Sciences (approval code: IR.SBMU.PHARMACY.REC.1398.235).
In this study, we included all adult patients (over the age of 18) who underwent gastrointestinal or cardiovascular surgery between the beginning of April 2021 and the end of June 2021. Additionally, we considered the exclusion criteria as patients who did not complete the follow up period.
Measurements
The participants were split into two groups, each consisting of 100 patients. Both groups were comparable in terms of average age, medication usage, type of surgery, and other medical conditions. Initially, both groups were prescribed antibiotics based on the surgeons' recommendations. A pharmacist consultation was conducted for all participants simultaneously. Subsequently, the first group continued to follow the antibiotic regimen suggested by the surgeons, while the second group received antibiotics based on the recommendations provided by the pharmacists.
In the first group, the pharmacist did not interfere in the treatment process and only observed patients from the beginning of the admission until discharge. On the other hand, in the second cluster, pharmacological advice in order to prescribing proper prophylactic antibiotic, dosage, the duration of treatment and the time of starting its administration according to the type of surgery and patients' condition was done and a written pharmacological consultation paper placed in the patients' records.
Recommendations for selecting a prophylactic antibiotic based on the type of surgery are illustrated in Table 1.
A descriptive questionnaire designed by Ayatollah Taleghani Medical and Educational Hospital was used to record patients' information and medical data such as gender, age, type of surgery, type of prophylactic antibiotic, antibiotic dosage, prescription period and postoperative infection. All medical data were kept as a computerized database.
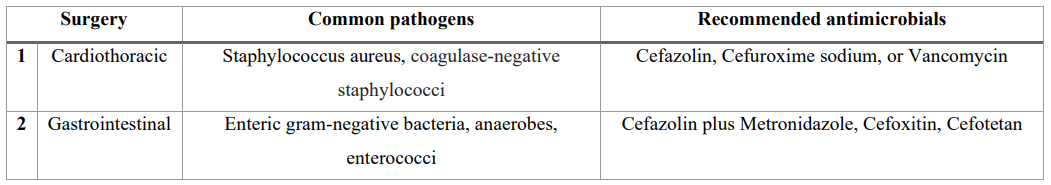
Table 1: Antibiotic prophylaxis for the prevention of SSI based on UpToDate (1)
Statistical analysis
All data were analyzed using descriptive statistics (mean and standard deviation) as well as analytical statistics. SPSS software was used to examine the data (IBM version 90, SPSS, Statistics, Chicago, IL, USA). The Kolmogorov-Smirnov test was used to evaluate data distribution, and if normal, parametric tests were used; otherwise, non-parametric equivalents of the same tests were used. The data were analyzed using the paired t-test and the Chi-square test. The observer error was calculated using the Interclass Correlation Coefficient (ICC) and the Pearson test. Significant levels were defined as values less than 0.05.
Results
Two hundred patients who underwent gastrointestinal or cardiovascular surgery and were admitted between April and June 2021, were enrolled in this study.
They were divided into two groups (100 patients in each) including 32 and 50 females in the first group and second group, respectively. The difference in the number of the female genders was statistically significant (P=0.047) between these two clusters. In addition, 38% of patients had no underlying disease and only 11% of them had hypertension in the first group. In the second cluster, 51 cases had no underlying disease and 12% had hypertension with diabetes mellitus. There was no significant difference between these groups.
We identified that most surgeries performed in the first group were linked to colectomy (29%). On the other hand, cholecystectomy (28%) was the most common surgical procedure in the second group. The types of surgeries in each group are demonstrated in Table 2.
Prophylactic antibiotics were considered for 71 patients in the first group, whereas in the second group, antibiotics were prescribed for all individuals. According to the guidelines, the requirement for prophylactic antibiotics, based on clinical condition and type of surgery, was 78% and 84% in these two groups, respectively.
Moreover, in terms of choosing the best type of prophylactic antibiotic, antibiotic dosage, or period of use, this decision was incorrect in 80% of cases in the first group. Furthermore, in the second group of the study, initially without pharmacist intervention, all cases received inappropriate antibiotics, Specifically, in terms of dosage, duration of use or the proper choice of antibiotics, and following the pharmacist's recommendation, this rate decreased to 88%.
Proper prophylactic antibiotics according to the type of antibiotic, dosage, and duration were prescribed for 12 patients after pharmacological consultation. Except for those 12 cases, pharmacist intervention resulted in the correction of 27.2% of prophylactic antibiotics dosage (P=0.000) and 43.1% of prophylactic antibiotics duration (P=0.007).
In the first group of the study, there were 6 cases of surgical site infection, including 3 cases of infection following hernia surgery, one case of infection following colectomy surgery, one case following angiography, and one case following permcath placement. On the other hand, there was no report of SSI in the second group.
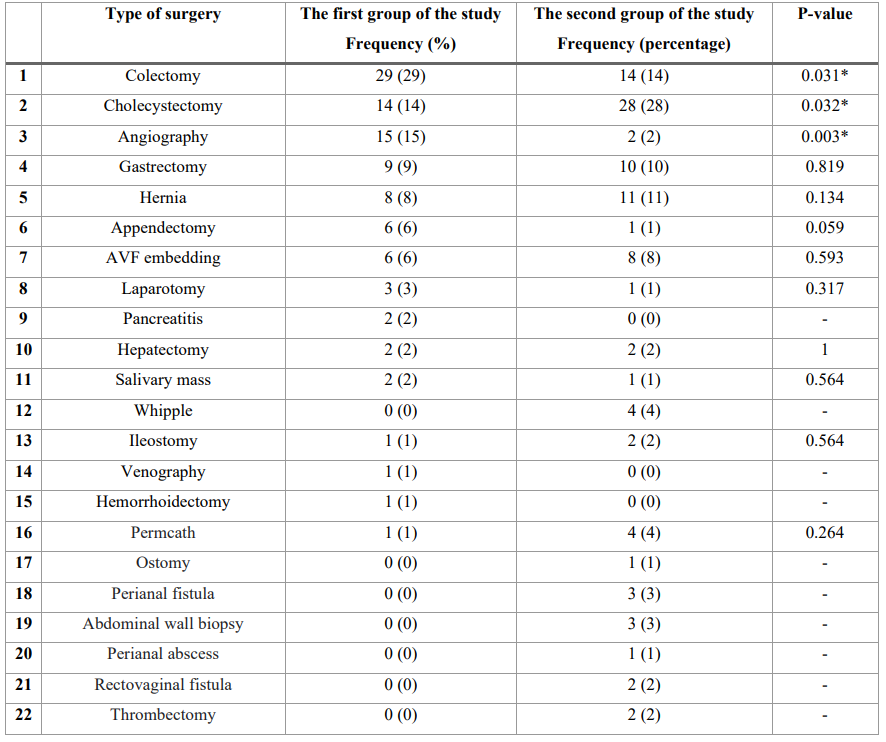
Table 2: Specifications of the type of surgery performed in the first and second group of the study.
In both groups of the study, the compliance of antimicrobial prophylaxis was assessed using several criteria, and the findings are given in Table 3.
Table 4 This highlights the pharmacist's involvement, which includes assessing potential drug interactions between the prescribed prophylactic antibiotics and the patient's other medications, as well as determining the appropriate dosage of prophylactic antibiotics based on the patient's hepatic/renal function. In this study, there was only a case of drug interaction in the first group. These issues can cause serious problems in patients showing the importance of existing clinical pharmacists in surgical wards.
Additionally, the following were the most common errors in
choosing prophylactic antibiotics:
1. Considering Cefazolin ampule (1g) instead of Cefazolin ampule (2g).
2. Considering Ceftriaxone ampule (1g) or Ciprofloxacin ampule (400mg) instead of Cefazolin ampule (2g) in colorectal surgeries.
Excluding the prescription of Metronidazole ampule (500mg) in colorectal surgeries.
Discussion
The present study has collected comprehensive data on the pharmacist interventions in prescribing proper antimicrobial medications and reducing the rate of SSI. Our study identified that pharmacist consultation was correlated with lower rate of SSI. Also, it can improve the amount of administration of appropriate antibiotics according to the type, dosage and duration.
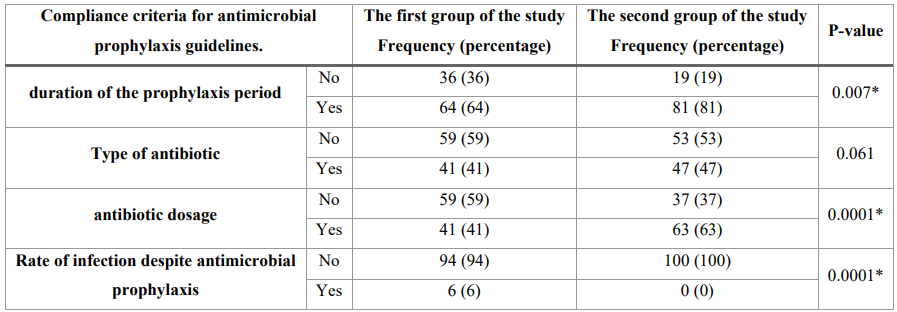
Table 3: Different criteria for Compatibility of prescribed antibiotics with consensus guidelines
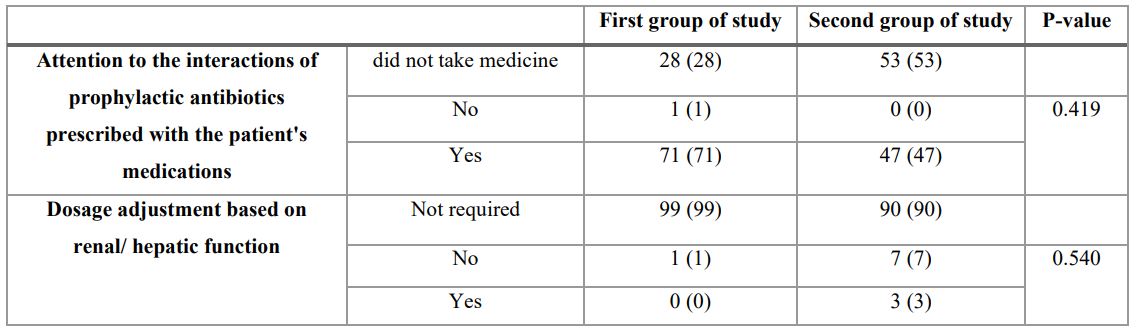
Table 4: Areas in which a pharmacist intervention can be impactful.
In the current study, infection rate was calculated as 6% in the first group that was higher in comparison with the second group (0%), causing a return to the hospital, increasing hospitalization rate and health care cost, almost similar to a previous study that revealed pharmacist intervention can reduce the length of hospital stay and admission cost [12]. Similar to our result, Gonzales et al. demonstrated that using pharmacist intervention is associated with less hospitalizations and infection [13]. In contrast with these findings, Holland et al. displayed that Pharmacist-led medication interventions may not reliably reduce hospital admissions or mortality rates in older individuals. While they can enhance drug knowledge and adherence, there is insufficient evidence of a positive impact on quality of life and Current trials are limited in size and lack consistent benefits [14].
Consistent with prior findings, the improper selection of prophylactic antibiotic type, dosage, and duration reduces the effectiveness of surgical antimicrobial prophylaxis and increases the risk of SSI [15]. On the other hand, Prolonged antimicrobial prophylaxis is frequently practiced after surgery, but it does not necessarily decrease the risk of surgical site infections (SSI) and increases the likelihood of developing antibiotic resistance. The improper administration of prophylactic antibiotics may result from misconceptions. Therefore, it is crucial to ensure proper antibiotic administration and address concerns regarding resistance. [16].
Concerning the research findings, the duration of the prophylactic period, the selection of the prescribed medication dosage, the requirement for re-administration, and the period of usage were considerably more in line with the guidelines in the second group of the study. Similar to our findings, Hailu et al. showed that the presence of clinical pharmacist decreases drug related problems such as inappropriate drug and dose selection [17]. This outcome has vital effects on multidisciplinary teams and participating clinical pharmacist as a part of this team reduces the SSI and simplifies choosing the proper prophylactic regimen.
Similar to previous study [17], our result revealed the existence of a clinical pharmacist in surgical wards plays an important role in achieving the proper duration of the prophylaxis (P=0.007). Moreover, the selection of the prescribed drug dosage upgraded with pharmacological consultation as well (P=0.0001). Additionally, the requirement for re-administration decreased in the second group of the study which pharmacist intervention resulted in drug reordering and total compliance to the guidelines in 12% of patients.
Clinical pharmacists with up-to-date knowledge play a vital role in multidisciplinary teams alongside physicians and nurses. Working together, they can reduce the risk of SSI and improve the selection of the most suitable pre- and postoperative regimens. Their involvement contributes to a comprehensive approach and enhances patient care.
Conclusion
To conclude, the presence of pharmacists in surgical wards is pivotal in order to prescribing prophylactic antibiotics according to the guidelines. Moreover, the pharmacist intervention can decrease the incidence of SSI by adjusting the duration of antibiotic prophylaxis and antibiotic dosage selection. Further studies are required to reveal the role of pharmacists in decreasing postoperative infections and other postoperative complications, prescribing appropriate antimicrobial medications and establishing rules for the presence of pharmacists in surgical departments.
Acknowledgements: Not applicable
Funding: No additional funding for the execution of the present study was received.
Availability of data and materials: The data and materials used in the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate: The study was approved by the institutional ethics committee and written informed consent was obtained from all participants.
Consent for publication: Written informed consent was obtained from the patient's family for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests: The authors declare that they have no competing or conflict of interests.
References
- Salkind AR, Rao KC. (2011) Antiobiotic prophylaxis to prevent surgical site infections. American family physician. 83(5): 585-590. [PubMed.]
- Jeys L, Grimer R, Carter S, Tillman R, Abudu A. (2007) Post operative infection and increased survival in osteosarcoma patients: are they associated? Annals of surgical oncology. 14(10): 2887-2895. [PubMed.]
- Lajiness MJ. (2009) Antibiotic prophylaxis: what is it? Why do we care? Urologic Nursing. 29(3): 199-203. [PubMed.]
- Crader MF, Varacallo M. (2017) Preoperative antibiotic prophylaxis. 28723061 [PubMed.]
- Stulberg JJ, Delaney CP, Neuhauser DV, Aron DC, Fu P, et al. (2010) Adherence to surgical care improvement project measures and the association with postoperative infections. Jama. 303(24): 2479-2485. [PubMed.]
- Van Kasteren ME, Mannien J, Ott A, Kullberg B-J, de Boer AS, et al. (2007) Antibiotic prophylaxis and the risk of surgical site infections following total hip arthroplasty: timely administration is the most important factor. Clinical Infectious Diseases. 44(7): 921-927. [PubMed.]
- Steinberg JP, Braun BI, Hellinger WC, Kusek L, Bozikis MR, et al. (2009) Timing of antimicrobial prophylaxis and the risk of surgical site infections: results from the Trial to Reduce Antimicrobial Prophylaxis Errors. Annals of surgery. 250(1): 10-16. [PubMed.]
- Brown J, Doloresco III F, Mylotte JM. (2009) “Never events”: not every hospital-acquired infection ispreventable. Clinical Infectious Diseases. 49(5): 743-746. [Ref.]
- Berríos-Torres SI, Umscheid CA, Bratzler DW, Leas B, Stone EC, et al. (2017) Centers for disease control and prevention guideline for the prevention of surgical site infection, 2017. JAMA surgery. 152(8): 784-791. [PubMed.]
- Fésüs A, Benkő R, Matuz M, Kungler-Gorácz O, Fésüs MÁ, et al. (2021) The Effect of Pharmacist-Led Intervention on Surgical Antibacterial Prophylaxis (SAP) at an Orthopedic Unit. Antibiotics. 10(12): 1509. [Ref.]
- Zhou L, Ma J, Gao J, Chen S, Bao J. (2016) Optimizing prophylactic antibiotic practice for cardiothoracic surgery by pharmacists’ effects. Medicine. 95(9). [PubMed.]
- Shen J, Sun Q, Zhou X, Wei Y, Qi Y, et al. (2011) Pharmacist interventions on antibiotic use in inpatients with respiratory tract infections in a Chinese hospital. International journal of clinical pharmacy. 33(6): 929-933. [PubMed.]
- Gonzales HM, Fleming JN, Gebregziabher M, Posadas-Salas MA, Su Z, et al. (2021) Pharmacist-led mobile health intervention and transplant medication safety: A randomized controlled clinical trial. Clinical Journal of the American Society of Nephrology. 16(5): 776-784. [PubMed.]
- Holland R, Desborough J, Goodyer L, Hall S, Wright D, et al. (2008) Does pharmacist‐led medication review help to reduce hospital admissions and deaths in older people? A systematic review and meta‐analysis. British journal of clinical pharmacology. 65(3): 303-316. [PubMed.]
- Montes CV, Vilar-Compte D, Velazquez C, Golzarri MF, Cornejo-Juarez P, et al. (2014) Risk factors for extended spectrum β-lactamase-producing Escherichia coli versus susceptible E. coli in surgical site infections among cancer patients in Mexico. Surgical infections. 15(5): 627-634. [PubMed.]
- Harbarth S, Samore MH, Lichtenberg D, Carmeli Y. (2000) Prolonged antibiotic prophylaxis after cardiovascular surgery and its effect on surgical site infections and antimicrobial resistance. Circulation. 101(25): 2916-2921. [PubMed.]
- Hailu BY, Berhe DF, Gudina EK, Gidey K, Getachew M. (2020) Drug related problems in admitted geriatric patients: the impact of clinical pharmacist interventions. BMC geriatrics. 20(1): 1-8. [Ref.]