>Corresponding Author : S Zahri
>Article Type : Case Report
>Volume : 4 | Issue : 4
>Received Date : 12 Feb, 2024
>Accepted Date : 23 Feb, 2024
>Published Date : 27 Feb, 2024
>DOI : https://doi.org/10.54289/JCRMH2400118
>Citation : Zahri S, Bennani G, Charkaoui I, Ovaga BE, Haboub M, et al. (2024) Navigating the Triad: Large Pericardial Effusion, Pulmonary Embolism, and CMV Seropositivity in a Challenging Clinical Scenario- A Case Report. J Case Rep Med Hist 4(4): doi https://doi.org/10.54289/JCRMH2400118
>Copyright : © 2024 Zahri S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access
Cardiology department UHC Ibn Rochd, University Hospital Center Ibn Rochd, Hospital Street, 20360 Casablanca, Morocco
*Corresponding author: Zahri Soukaina, Cardiology department UHC Ibn Rochd, University Hospital Center Ibn Rochd, Hospital Street, 20360 Casablanca, Morocco
Abstract
This case study highlights the unusual coexistence of a large pericardial effusion, pulmonary embolism, and Cytomegalovirus (CMV) seropositivity in a 52-year-old active smoker. The complex interplay between cardiovascular and infectious etiologies in this triad poses diagnostic and therapeutic challenges. Through systematic analysis, this report aims to add valuable insights to the limited literature on this complex clinical scenario.
Keywords: Pericardial Effusion; Pulmonary Embolism; Cytomegalovirus
Abbreviations: CMV: Cytomegalovirus
Introduction
The coexistence of a large pericardial effusion, pulmonary embolism, and Cytomegalovirus (CMV) seropositivity represents a rare and challenging clinical scenario. This triad, though infrequently reported in the literature, highlights the complex interplay between cardiovascular and infectious aetiologies.
Pericardial effusion, a recognised manifestation of several systemic conditions, has been associated with compromised hemodynamics and multiple aetiologies, including infectious and neoplastic origins [1]. Pulmonary embolism, a well-established cardiovascular emergency, is a known contributor to pericardial effusion, emphasising the importance of thorough investigation [2]. In addition, the overlap of CMV seropositivity introduces an immunocompromised dimension, that may influence the clinical course [3].
In this case study, we present the clinical details of a 52-year-old man, an active smoker, admitted with this triad, navigating the complexities of diagnosis and management. Through a systematic analysis, we aim to contribute to the limited existing literature on the coexistence of these entities and the implications for patient care.
Case Presentation
We report the case of a 52-year-old man, an active smoker with no particular pathological history, admitted to the cardiology department of CHU IBN ROCHD CASABLANCA for a large pericardial effusion with poor hemodynamic tolerance, punctured with the removal of one liter of serum fluid; symptomatology dating back 1 week, with the onset of exertional dyspnea; becoming at rest 4 days before admission, associated with a hacking cough; with no notion of chest pain, all evolving in a context of preserved general condition.
Physical examination revealed a dyspneic patient at rest (NYHA stage 4), with arterial hypotension at 90/50mmHg, tachycardia at 104 bpm, respiratory rate at 18 cycles per minute, O2 saturation at 94% on free air, with turgidity of the jugular veins and hepatalgia; cardiovascular auscultation revealed muffled heart sounds.
The electrocardiogram showed peripheral microvoltage and right bundle branch block (figure 1).
Transthoracic echocardiography revealed an abundant pericardial effusion, compressing the right cavities in proto-diastole, with significant flow variation (figure2).
27 mm >> OD.
32 mm >> RV.
26 mm >> LV.
16 mm >> OG.
26 mm >> Apex.
Inferior vena cava dilated to 23 mm;(figure3).
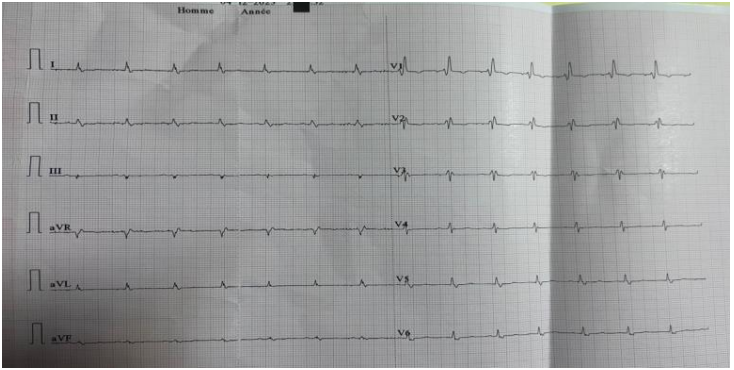
Figure 1: diffuse low voltage with right bundle branch block
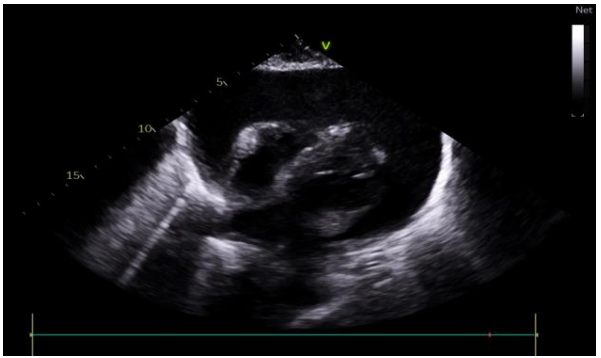
Figure 2: subcostal view showing a large pericardial effusion
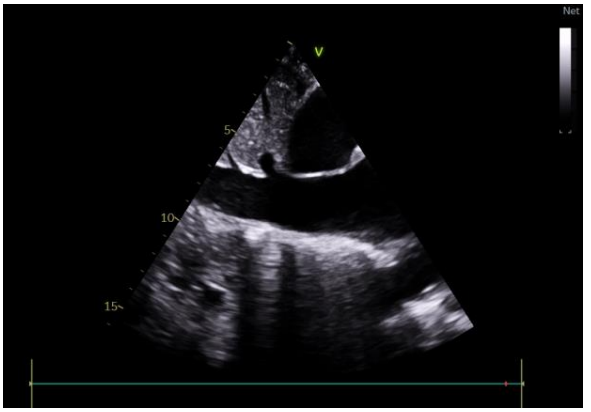
Figure 3: subcostal view showing the dilation of the inferior vena cava
Biological workup:
Hb was correct at 12.4 gr/dl, leukocyte count correct at 7130/mm3, PNN count at 4930; platelet count at 298,000, SV high at 39 mm/1st hour, CRP slightly elevated at 35, with D-dimer level removed at 3720;
Renal function was correct: urea 0.40 g/L, creatinine 7.8 mg/L, estimating glomerular filtration rate according to MDRD at 101 ml/min/1.73m2, a slight increase in transaminases with ASAT at 69 and ALAT 107;
As part of an etiological work-up, we completed the following:
- Pericardial puncture fluid showed an exudative fluid, bacteriological study negative, with absence of BAAR, ADA limit at 52 for a normal < 50, Gene expert negative; Anapath in progress.
- ECBE: negative.
- Tumour markers negative.
- Viral serologies: CMV positive with: AC-anti-CMV IgM + a 1,21 (< 0,85) and AC-anti-IgG + a 217 AU/ml (<6), the rest of the serologies were negative: HIV 1,2, HBV, HCV, EBV Syphilitic serology: negative.
Angio Thoracic CT showing :(figure4)
- multisegmented pulmonary embolism (IO=40%), dilation of cardiac cavities + reflux cave: acute pulmonary heart;
- bilateral and pericardial pleural fluid effusion of moderate abundance;
Therapeutic treatment:
The patient was initially treated with prophylactic antibiotics based on a combination of Amox-acid-clavulanic acid and 500 cc saline after pericardial puncture. The evolution was marked by a recurrence of the effusion on several occasions of low to medium abundance.
After confirming pulmonary embolism and positive CMV serology, antiviral treatment was initiated with oral ganciclovir 500 mg 2cp * 3 / day for 3 weeks; as well as aspirin 1g 1 s * 3 /d and colchicine 0.5 mg 1cp * 2 /d, with curative anticoagulation based on LMWH 0.6 IU 1 inj* 2 /d; switched on discharge to oral anticoagulation with rivaroxaban.
The evolution was spectacular; marked during the first 3 days by regression of the pericardial effusion until the drying of the pericardium (figure5).
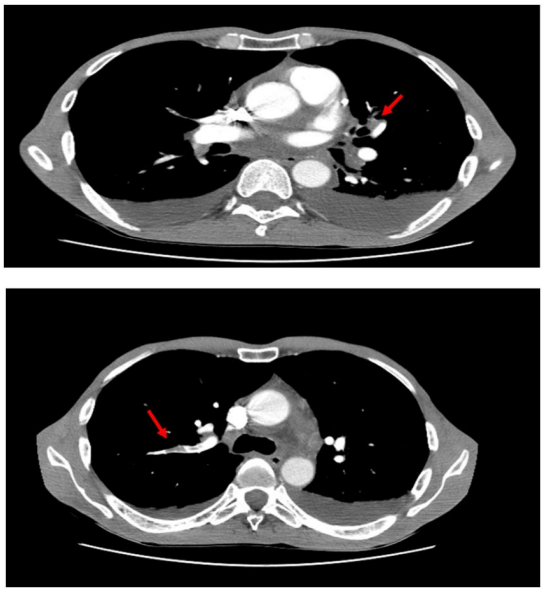
Figure 4: chest CT angiography showing bilateral segmental and subsegmental pulmonary embolism and pleural effusion
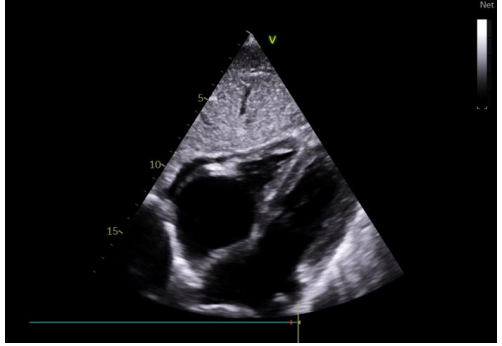
Figure 5: total regression of pericardial effusion
Discussion
The presented case involves a complex interplay of a large pericardial effusion, pulmonary embolism, and Cytomegalovirus (CMV) seropositivity, which is a rare clinical scenario. Each component of this triad introduces unique challenges, and their simultaneous occurrence in a patient warrants a comprehensive discussion.
Pericardial Effusion
Pericardial effusion is a recognized manifestation of various systemic conditions and can arise from infectious, neoplastic, or inflammatory origins [1].
Compromised hemodynamics due to pericardial effusion underscores the importance of prompt diagnosis and management [1].
The association of pericardial effusion with pulmonary embolism in this case emphasizes the need for a thorough investigation into the underlying etiologies [2].
Pulmonary Embolism
Pulmonary embolism is a well-established cardiovascular emergency that can contribute to pericardial effusion, as seen in this case [2].
The acute presentation of multisegmental pulmonary embolism with concurrent dilation of cardiac cavities and reflux cave highlights the severity of the cardiovascular compromise.
Prompt recognition and management of pulmonary embolism are crucial to prevent further complications.
Cytomegalovirus (CMV) Seropositivity
CMV is a member of the herpesvirus family and can cause opportunistic infections in immunocompromised individuals [3].
The positive CMV serology in this case introduces an immunocompromised dimension, potentially influencing the clinical course [4].
Immunocompromised states, such as CMV seropositivity, may exacerbate the severity of infectious and cardiovascular conditions.
CMV (cytomegalovirus) infection is a common infection that can be complicated, not exceptionally, by venous thromboembolic events [5].
Diagnostic Challenges
The diagnostic challenge in this case stems from the complexity of simultaneously addressing pericardial effusion, pulmonary embolism, and CMV infection.
Echocardiography, laboratory studies, and imaging modalities, including CT angiography, played pivotal roles in confirming the diagnoses and guiding the treatment plan.
Management Strategies
The initial management involved pericardial puncture and drainage, addressing the acute cardiovascular compromise associated with the pericardial effusion.
Antiviral treatment with oral ganciclovir and curative anticoagulation was initiated after confirming pulmonary embolism and positive CMV serology.
The subsequent transition to oral anticoagulation with rivaroxaban and the patient's remarkable improvement highlight the efficacy of the chosen therapeutic strategies.
Multidisciplinary Approach
The successful outcome of this case underscores the importance of a multidisciplinary approach involving cardiology, infectious disease, and hematology specialists.
Collaboration among various specialties facilitated timely interventions and optimized patient care.
Conclusion
This case emphasizes the successful management of a challenging clinical scenario involving pericardial effusion, pulmonary embolism, and CMV infection. Timely intervention and a multidisciplinary approach contributed to the favorable outcome. Further studies are needed to elucidate the relationship between these conditions and optimal therapeutic strategies.
Declarations Consent for publication:
Written informed consent was obtained from the patients for publication of this case report and any accompanying images. Availability of data and material: All data analysed during this study are included in this published article.
Competing interests: The authors declare that they have no competing interests.
Author contributions:
Zahri Soukaina: writing paper
Bennani Ghali: study concept literature
Charkaoui Ibtissam: interpretation and analysis
Ovaga Brigitte Esther: Interpretation and analysis
References
- Maisch B, Seferović PM, Ristić AD, et al. (2004) Guidelines on the diagnosis and management of pericardial diseases executive summary) The Task force on the diagnosis and management of pericardial diseases of the European Society of Cardiology. Eur Heart J. 25(7): 587-610. [PubMed.]
- Konstantinides SV, Meyer G, Becattini C, et al. (2020) 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur Heart J. 41(4): 543-603. [PubMed.]
- Cannon MJ, Schmid DS, Hyde TB. (2010) Review of cytomegalovirus seroprevalence and demographic characteristics associated with infection. Rev Med Virol. 20(4): 202-213 [PubMed.]
- Justo D, Finn T, Atzmony L, Guy N, Steinvil A. (2011) Thrombosis associated with acute cytomegalovirus infection: a meta-analysis. Eur J Intern Med. 22(2): 195-199. [PubMed.]
- Kelkar AH, Jacob KS, Yousif EB, Farrell JJ. (2017) Venous thromboembolism related to cytomegalovirus infection: a case report and literature review. Medicine. 96(51): e9336. [Ref.]