Aisha A*, Aswin Kumar, Indu Sasikumar and Iswarya S Nair
Department of Radiation Oncology, Regional Cancer Centre, Thiruvananthapuram
*Corresponding author:
Aisha A, Department of Radiation Oncology, Regional Cancer Centre, Thiruvananthapuram
Abbreviations: FTGCT: Familial Testicular Germ Cell Tumours, TGCT: Testicular Germ Cell Tumours, GCNIS: Germ Cell Neoplasia in Situ
Introduction
Familial testicular germ cell tumours (FTGCT) are testicular germ cell tumours (TGCT) diagnosed in at least two blood relatives and account for 1-2% of all cases of TGCT. Brothers and fathers of TGCT patients have an 8-10 and 4-6-fold increased risk of TGCT, respectively. We report a case of testicular germ cell tumour in two siblings.
Case Report
Case 1
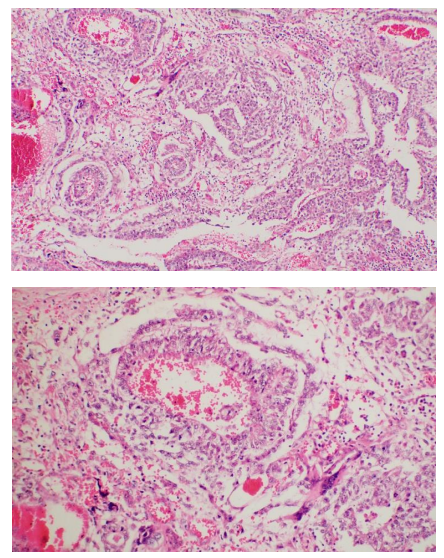
A forty-year-old young gentleman was referred to our centre with complaints of right scrotal swelling. There was no family history of testicular cancer or any other malignancy or cryptorchidism. He was detected to have a right testicular tumour and underwent high inguinal orchiectomy. The histopathological examination revealed seminoma with no lymphovascular emboli and was staged as pT1 disease. He received adjuvant radiation to the paraaortic nodal region to a dose of 20 Gy in 10 fractions 2 Gray per fraction 5 days a week for 2 weeks. He has been on regular follow-ups at our centre with clinical examination, serum tumour markers, and imaging for the past 11 years, and he is disease-free.
Case 2
His younger brother was evaluated at our centre three years later, with complaints of right testicular swelling at the age of thirty-seven years. Ultrasound examination of the scrotum showed a lesion measuring 2x1.6 cm with mild hypoechoic echotexture in the right testis. Tumour markers were not elevated. He underwent a high inguinal orchidectomy. Histopathological examination revealed a malignant mixed germ cell tumour with embryonal carcinoma, yolk sac tumour, seminoma and choriocarcinomatous components with no lymphovascular emboli. Imaging did not reveal evidence of disease elsewhere. Since he had stage I disease without any risk factors, he was advised active surveillance. He has since completed the active surveillance programme. He was disease-free at the time of the last follow-up visit.
Discussion
Testicular tumours are uncommon in Asia, with an incidence of testicular tumours of 0.4 per 100,000 population. Familial germ cell tumours comprise 2–5% of all testicular cancer cases. Approximately 1.4% of newly diagnosed TGCT patients have a positive family history of TGCT. Patients with familial tumours are diagnosed earlier than those with sporadic tumours. Sons and siblings of TGCT patients have four- to sixfold and eight- to tenfold increases in TGCT risk, respectively.
There are multiple risk factors for TGCT. Contralateral testicular cancer, cryptorchidism, persistent Mullerian duct syndrome, testicular dysgenesis, infertility, testicular atrophy, testicular intraepithelial neoplasia, mixed gonadal dysgenesis, Klinefelter's syndrome and testicular microlithiasis are more solidly established. Other putative factors include inguinal hernia and hydrocele, polythelia, in-utero exposure to diethylstilbesterol, gynecomastia and occupational exposure to polyvinyl chloride.
Family history, cryptorchidism and testicular microlithiasis are the most substantial known risk factors, but no robust environmental risk factors have been identified. Despite the high heritability of TGCT, estimated at 37–49%, pathogenic variants of CHEK2 are the only moderate penetrance genes associated with an increased risk of TGCT.
Y chromosome gr/gr deletion and PDE11A gene mutations have been implicated as genetic modifiers of FTGCT risk. Two genome-wide association studies of predominantly sporadic cases of TGCT have implicated the KIT-ligand, SPRY4, and BAK1 genes as TGCT risk modifiers. All five loci are involved in normal testicular development or male infertility. These genetic data provide a novel insight into the genetic basis of FTGCT and are an invaluable guide to future TGCT research [1].
In 2021, the International Testicular Cancer Linkage Consortium reported the 22 susceptibility gene loci associated with testicular germ cell tumours. Most risk variants map to loci containing genes encoding proteins implicated in critical pathways for male germ cell development, chromosomal segregation, sex determination, and DNA maintenance. Biologically, these findings complement the current understanding of disease pathogenesis involving in utero transformation of fetal germ cells into germ cell neoplasia in situ (GCNIS), the common precursor of TGCT [2].
Conclusion
Testicular self-examination is recommended for family members of a person with TGCT. A definite genetic abnormality of a familial variant of TGCT has not been identified. Genes are not the only factors of a familial variant of TGCT. Diets, similar environmental and occupational exposures, and analogous patterns of reproductive decision-making might be similar in a given family. Thus, further research on the genetic predisposition in testicular cancer is necessary.
References
-
Kratz CP, Mai PL, Greene MH. (2010) Familial testicular germ cell tumours. Best Pract Res Clin Endocrinol Metab. 24(3): 503-513.
[Ref.]
-
Pluta J, Pyle LC, Nead KT, et al. (2021) Identification of 22 susceptibility loci associated with testicular germ cell tumors. Nat Commun. 12: 4487.
[Ref.]