>Corresponding Author : Laura Cano
>Article Type : Case Report
>Volume : 4 | Issue : 6
>Received Date : 12 March, 2024
>Accepted Date : 23 March, 2024
>Published Date : 27 March, 2024
>DOI : https://doi.org/10.54289/JCRMH2400126
>Citation : Cano L, López A, Morales D and Bonilla I. (2024) Myocardial Injury in Hip Fracture: When to Operate? J Case Rep Med Hist 4(6): doi https://doi.org/10.54289/JCRMH2400126
>Copyright : © 2024 Cano L, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access
1Internist and Geriatrician, Universidad de Caldas, Fundación Santa Fe de Bogotá, Colombia
2Geronnthrology and Geriatrics Research Group, Universidad de Caldas, Colombia
3Medicine Student, Universidad de Caldas, Colombia
*Corresponding author: Laura María Cano Méndez, Internist and Geriatrician, Universidad de Caldas, Fundación Santa Fe de Bogotá, Colombia
Introduction
Fragility Hip Fracture [Fragility Hip Fracture (FHF)] could be considered an urgency since delay in hip surgery greater than 48 hours leads to significant increases in mortality and major complications. Troponin I [Troponin I (cTn I)] for diagnosis of acute myocardial infarction [acute myocardial infarction (AMI)] is a tool that has been losing specificity due to the use of highly sensitive laboratory assays, which can lead to false positives results. The presence of FHF and elevated cTn I is a challenge for treating physicians, since confirming the diagnosis of AMI could delay surgical intervention and, take to hip surgery an infarcted patient, represents a very high risk. The scientific evidence in this regard is still not conclusive about how to proceed in this scenario. Two illustrative clinical cases and a review of the available evidence are presented here to help to guide decision-making.
Keywords: Osteoporosis; Hip Fracture; Myocardial Injury; Troponin I
Abbreviations: FHF: Fragility Hip Fracture, Tn: Troponin, AMI: Acute Myocardial Infarction, ECG: Electrocardiogram, HR: Hazzard Ratio
Case 1
Ninety-three-year-old woman with a history of atrial fibrillation, ischemic cardiomyopathy, heart failure mildly reduced ejection fraction, high blood pressure, chronic obstructive pulmonary disease, with 50-point Barthel index before admission, 4-point Lawton scale, and no cognitive impairment. She was admitted to emergency room due to a fall from her own height resulting in an intertrochanteric fracture of the right femur. She reported dizziness after admission and laboratory tests were collected (see Table 1). The electrocardiogram [electrocardiogram (ECG)] showed atrial fibrillation rhythm with controlled ventricular response, the echocardiogram evidenced concentric remodeling of the left ventricle, hypokinesia of the basal septum and the inferior wall of the ventricle and 49% ejection fraction. She never presented thoracic pain, dyspnea, diaphoresis, or hemodynamic instability. It was unclear if echocardiographic changes were new or old and the patient rejected all types of coronary stratification. Together her family and physicians decided to take her into hip surgery after 22 hours of admission. She died during anesthetic induction.
Case 2
Eighty-four-year-old woman with a history of high blood pressure, prediabetes, lumbar spinal stenosis, 100-point Barthel index prior to admission, 8- point Lawton scale, no cognitive impairment, who was admitted due to a fall from her own height resulting in an intracapsular fracture of the right femur. The admission ECG showed T-wave inversion in lower leads and ST segment depression in septal and lateral leads. Patient denied symptoms, including thoracic pain, dyspnea, or diaphoresis, and always showed normal vital signs. cTn I was measured (see Table 1), her echocardiogram showed a left ventricle with normal dimensions, no contractility disorders, and 60% ejection fraction. She underwent total hip arthroplasty successfully after 62 hours of admission and stayed in the hospital for seven days.
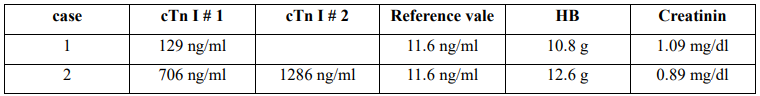
Table 1: cTn I: troponin I
Discussion
Cardiac troponins are components of the myofibrillar apparatus, they are released into circulation after a cardiomyocyte injury, which does not necessarily mean necrosis. With the advent of high-sensitivity laboratory tests, defined as those with the capacity to quantify the level of a cardiac biomarker in at least 50% of healthy people, the specificity of this tool in the diagnosis of AMI has been reduced [1]. According to the Fourth Universal Definition of AMI, besides the presence of myocardial injury, there should also be evidence of myocardial ischemia with at least one of the following findings: 1) symptoms of myocardial ischemia, 2) de novo ischemic changes in the ECG, 3) de novo pathological Q waves, 4) segmental contractility disorders de novo in cardiac images 5) coronary thrombus in the coronary angiogram [2].
In case 1, given its background, it was unclear whether the echocardiographic findings were old injuries, that is why elevated cTn I could be interpreted as a chronic myocardial lesion. However, the possibility of coronary stratification was evaluated within physicians team and was rejected by patient, leading to the decision of take her into surgery as described.
In case 2, if we consider the electrocardiographic changes as new, we would be facing an AMI without symptoms and without echocardiographic changes. Nevertheless, we did not know if the changes were acute or chronic, so there was a possibility of a chronic myocardial injury.
In case 1, even though there was a 50-point Barthel index, multimorbidity, and 93 years, the surgical risk was assumed because, worldwide, more than 95% of patients with hip fractures are treated surgically given that international guidelines suggest that adequate pain treatment requires surgical management even if the patient has a low life expectancy [3]. Mortality rates in FHF patients without surgical management was reported in a meta-analysis, at 30 days, six months, and one year as 36%, 46%, and 60%, respectively [3]. Consequently, this opens the discussion on how to interpret an elevated cTn I value in the context of FHF and, if in case of acute myocardial injury, the correct procedure is to perform a coronary angiography before or after hip surgery.
To answer this question, we reviewed the available scientific literature and found studies like Fisher’s et al., they obtained cTn I within 72 hours of admission of 238 patients with FHF: 23.5% during preoperatory and 76.5% during postoperative. Their objective was to determine if elevated cTn I affected the outcomes of hospital death, length stay, and destination after discharge. They found that 29% of evaluated patients has elevated cTn I during perioperative, 26% of which were measured in the preoperatory. Hospital mortality in patients with elevated cTn I was two times higher than in the control group, and hospital stay was longer, without statistically significant differences for any of outcomes [4].
Rostagno et al. evaluated 1025 patients with FHF, from which 21 had suspected AMI before surgery due to changes in ECG and cTn I elevation. Of those 21 patients, five presented AMI with ST elevation. The other 16 were diagnosed with AMI without ST elevation, and five of them were classified as unacceptable surgical risk after a multidisciplinary evaluation by ASA >3 classification, severe cognitive impairment, and functional decline. They received conservative management and died within one year. In the remaining 11 patients, surgical treatment was carried out under general anesthesia within an average of 3.7 days. One patient died of refractory heart failure in the postoperative, and four patients underwent coronary angiography after hip surgery. These four patients complied with the Mayo Clinic criteria for stress-induced myocardiopathy and none of them had significant coronary injuries in the angiography. At one-year follow-up, 80% were alive [5].
On contrast, another study by Rostagno et al., analyzed a cohort of 1030 patients and found that 92 presented elevated cTn I in the preoperatory, from which 18 underwent coronary angiography within four days after hip surgery. All patients had ≥70% stenosis in two or three major epicardial arteries, and they highlighted that the electrocardiographic and echocardiographic alterations were not significatively more frequent in patients who underwent coronary angiography [6].
In a cohort study by Vallet et al., they evaluated patients admitted with hip fracture between 2009 and 2013 in a geriatric unit, the objective was to evaluate the prognostic value of isolated cTn I elevation. A total of 312 patients were divided into the control group (n=217), the isolated troponin elevation group (n=50), and the acute coronary syndrome group (n=45). The main outcome was mortality after six months and readmission to the hospital. There was no significant difference in postoperative complications between isolated troponin elevation and the control group. In contrast, atrial fibrillation, acute heart failure, hemorrhage, or ICU admission were significatively more frequent in the acute coronary syndrome group.
Likewise, mortality after six months was higher in these group. Of patients who presented with acute coronary syndrome, only six underwent coronary arteriography, showing coronary stenosis in four patients and chronic coronary occlusion in three patients. Among the latter, one had a stent. One patient was diagnosed with Takotsubo syndrome. The authors concluded that isolated troponin elevation in patients with hip fracture was not associated with a significant increase in death or readmission to the hospital after six months [7].
In 2020, Rostagno et al. published another study whose objective was to evaluate the incidence of acute myocardial infarction and hospital myocardial injury in patients that underwent hip fracture surgery and its association with mortality. They evaluated the medical history of 1970 patients, measured cTn I and took an ECG at admission, at 12, 24, and 48 hours after the surgery, they also took an echocardiogram before and within 48 hours after surgery. They found elevated troponin in 40.7% of the study population. The changes in the ECG and the abnormalities in the echocardiogram were more frequent in patients with higher levels of cTn I. A definitive diagnosis of infarction, according to the fourth universal definition, was achieved in 23% of patients after hip surgery, while in 17% the changes in cTn I were not associated with evidence of ischemia. Mortality was significatively higher in both groups with cTn I elevation compared with the control group [8].
Nathan et al., in their multivariate analysis, found that cTn I elevation was associated with a 1.8-times increase in mortality (95% CI, 0.9 to 3.5, P = 0.08) and a 1.5-times increase in major complications (95% CI, 0.8 to 2.6, P = 0.18). It is noteworthy that they used Charlson’s scale for the sensitivity analysis and for each additional comorbidity, it represents a Hazzard Ratio (HR) of 1.2 for mortality (1.2; 95% CI, 1.1 to 1.4, P < 0.001) and for a major complication (HR, 1.2; 95% CI, 1.0 to 2.3, P = 0.006) [9].
Conclusion
The studies we revised here had in common that the patients who more frequently presented elevated cTn I during the preoperatory were 85+ years, had an ASA >3 classification, and cardiovascular history of ischemic cardiopathy or cerebrovascular disease. Nevertheless, in none of the studies this tendency was statistically significant.
The correct procedure when patient has myocardial injury and FHF is still unclear in the current literature, specially, about which is the optimal time to intervene both conditions. It is clear in case of hemodynamic instability and uncontrolled cardiovascular symptoms, the priority is cardiovascular stabilization. It is also clear that FHF patients who are taken into surgery after 48 hours of hospital admission have increased mortality and complications. Elevation of the cTn I during perioperative in these patients is associated with worse outcomes.
Currently, the “HIP-ATTACK 2” study is ongoing (ClinicalTrials.gov Identifier: NCT04743765), which is a multicenter randomized controlled trial to determine if accelerated surgery in patients with acute myocardial injury is superior to standard care; results are expected in 2025.
More studies are necessary to establish the most appropriate procedure in patients with myocardial injury or acute myocardial infarction that require hip surgery.
References
- Alaour B, Liew F, Kaier TE. (2018) Cardiac Troponin - diagnostic problems and impact on cardiovascular disease. Annals of Medicine. Taylor and Francis Ltd. 50: 655-665. [PubMed.]
- Raber I, McCarthy CP, Januzzi JL. (2021) A Test in Context: Interpretation of High Sensitivity Cardiac Troponin Assays in Different Clinical Settings. Journal of the American College of Cardiology. Elsevier Inc. 77: 1357-1367. [PubMed.]
- Loggers SAI, van Lieshout EMM, Joosse P, Verhofstad MHJ, Willems HC. (2020) Prognosis of nonoperative treatment in elderly patients with a hip fracture: A systematic review and meta-analysis. Injury. Elsevier Ltd. 51: 2407-2413. [PubMed.]
- Fisher AA, Southcott EN, Goh SL, et al. (2008) Elevated serum cardiac troponin I in older patients with hip fracture: Incidence and prognostic significance. Arch Orthop Trauma Surg. 128: 1073-1079. [PubMed.]
- Rostagno C, Cammilli A, di Cristo A, et al. (2016) Acute coronary syndromes with significant troponin increase in patients with hip fracture prior to surgical repair: differential diagnosis and clinical implications. Intern Emerg Med. 11: 219-224. [PubMed.]
- Rostagno C, Peris A, Polidori GL, et al. (2019) Perioperative myocardial infarction in elderly patients with hip fracture. Is there a role for early coronary angiography? Int J Cardiol. 284: 1-5. [PubMed.]
- Vallet H, Breining A, Le Manach Y, et al. (2017) Isolated cardiac troponin rise does not modify the prognosis in elderly patients with hip fracture. Medicine (Baltimore). 96: 61-69 [Ref.]
- Rostagno C, Cartei A, Rubbieri G, et al. (2020) Perioperative Myocardial Infarction/Myocardial Injury Is Associated with High Hospital Mortality in Elderly Patients Undergoing Hip Fracture Surgery. J Clin Med. 9: 40-43. [PubMed.]
- O’Hara NN, Wu J, Rolle N, et al. (2022) Hip Fracture with Elevated Troponin: Harbinger of Mortality or Need for Accelerated Surgery? J Orthop Trauma. 36: 604-609. [PubMed.]