>Corresponding Author : Wissal Bencherifi
>Article Type : Case Report
>Volume : 4 | Issue : 6
>Received Date : 24 April, 2024
>Accepted Date : 08 May, 2024
>Published Date : 13 May, 2024
>DOI : https://doi.org/10.54289/JCRMH2400129
>Citation : Bencherifi W, Badi H, Ouladlahsen A, Ihbibane F, Sodqi M, et al. (2024) Listeria Rhombencephalitis: A Case of an Immunocompetent Adult. J Case Rep Med Hist 4(6): doi https://doi.org/10.54289/JCRMH2400129
>Copyright : © 2024 Bencherifi W, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access
Department of Infectious Diseases, CHU Ibn Rochd – Casablanca, Morocco
*Corresponding author: Wissal Bencherifi, Department of Infectious Diseases, CHU Ibn Rochd – Casablanca, Morocco
Abstract
Listeriosis is one of the most important foodborne diseases, caused by a Gram-positive facultative anaerobic intracellular bacterium found in food and the environment, Listeria monocytogenes. It causes one of the most life-threatening bacterial infections of the central nervous system (CNS). Meningoencephalitis and rhomboencephalitis are the most common forms and immunosuppression represents the main risk factor. In this article, we report a case of severe, invasive Listeria monocytogenes rhombencephalitis in a healthy middle-aged man, admitted to our hospital with meningeal syndrome associated with left VI nerve palsy. No apparent abnormality was found in a head CT and brain magnetic resonance imaging. Following the preliminary LP results, a diagnosis of bacterial meningitis was suspected and empirical antibiotic and antiviral therapy was initiated. Because of the lack of any significant improvement in his clinical status, on day 2 of his admission, a genetic identification of CSF pathogens by high-throughput genome sequencing was performed and identified L. monocytogenes. The Clinical status improved with complete recovery after appropriate antibiotic treatment with sulfamethoxazole-trimethoprim. In conclusion, in an infectious context, pontine involvement should systematically evoke the diagnosis of listeriosis.
Keywords: Rhomboencephalitis; Listeriosis; Neurolisteriosis; Listeria Monocytogenes; Meningitis
Abbreviations: CNS: Central Nervous System, CRP: C-Reactive Protein
Introduction
Listeriosis is an anthropozoonosis which commonly manifests in adults as septicemia and leads to damage to the central nervous system (CNS) in almost three quarters of cases [1]. Meningoencephalitis is the most common form of CNS infection with Listeria monocytogenes, as well as brainstem involvement or rhombencephalitis. This complication occurs particularly in weakened subjects such as newborns, pregnant women, people aged over 60 and the immunocompromised, but in rare cases neurolisteriosis can also affect immunocompetent subjects [2]. The objective of our article is to report the case of L. monocytogenes rhombencephalitis in a young immunocompetent man.
Case Presentation
A 28-year-old man, without any notable pathological history, hospitalized in the infectious diseases department for meningeal syndrome with fever at 40.8°C, evolving for three days with converging strabismus of the left eye and difficulty of vigilance. On clinical examination, the Glasgow score was 13, the initial neurological examination revealed clear meningeal stiffness, Kernig and Brudzinski signs were positive, left VI nerve palsy, with no other sensory or motor deficit. The rest of the clinical examination was normal. The blood test on admission showed an inflammatory syndrome with leukocytosis of 13,800, predominantly neutrophilic, a high fibrinogen level of 8.56 g/l and a C-reactive protein (CRP) of 178 mg/l. The blood ionogram, liver and kidney tests were normal. The CSF was crystal clear with hyperproteinemia at 1.84 g/l, hypoglycemia at 0.20g/l (ratio at 13%) and elevated white cell count of 350 cells/mm3 including 90% lymphocytes, with no germ present on direct examination or after culture. Blood cultures were sterile.
The emergency brain CT scan with injection was normal, as well as a brain MRI done two days after his hospitalization, which returned without abnormalities.
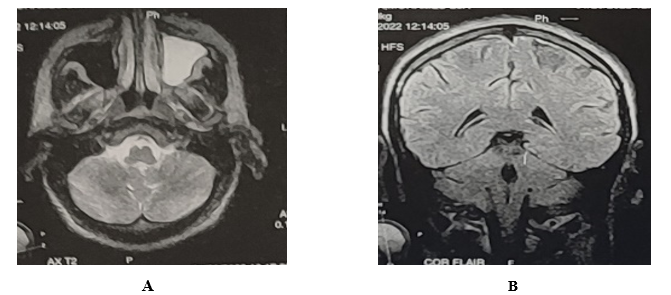
MRI: axial (A) and sagittal (B) T1 sequences with gadolinium injection showing no abnormality.
All of these elements made it possible to make the diagnosis of acute meningoencephalitis in an immunocompetent subject; the patient was treated with probabilistic antibiotic therapy consisting of ceftriaxone 100 mg/kg/day and acyclovir 10 mg/kg/8 hours. 48 hours later, and given the patient's non-improvement, a multiplex PCR was carried out detecting the presence of listeria monocytogenes, requiring a change in treatment with sulfamethoxazole-trimethoprim (160 mg/800 mg) 6 tablets per day in 3 doses, due to the unavailability of the injectable form of amoxicillin.
The evolution was favorable with rapid neurological improvement and apyrexia achieved within 72 hours. The biological inflammatory syndrome was rapidly decreasing, and the patient was hospitalized for 21 days; the damage to the left VI nerve with convergent strabismus persisted upon discharge, with good progress after orthoptic rehabilitation. The assessment for acquired or innate immunosuppression was negative.
Discussion
Listeria monocytogenes infection is transmitted through contaminated food and occurs in sporadic cases. There are risk factors that may suggest an invasive Listeria infection, such as pregnancy, particularly in the third trimester, extreme ages of life, innate or acquired natural immunosuppression, immunosuppressive treatment, hemodialysis patients, chronic alcohol patients. or with chronic liver failure, but Listeria monocytogenes is a virulent bacterium also affecting immunocompetent subjects [1,2]. The main route of transmission of L. monocytogenes is the digestive tract, the bacteria crosses the digestive barrier, and is disseminated by the lymphatic route then through the bloodstream via monocyte-macrophages. However, as in this case, a history of ingestion of contaminated food is often not found [3]. In immunocompetent patients, in more than 90% of cases, the infection remains asymptomatic except in a few rare cases such as in our patient [1,2]. Meningoencephalitis is the predominant clinical form of central nervous system infection. Damage to the brain parenchyma, usually associated with meningitis, is classically localized in the brainstem, giving rise to rhombencephalitis with cranial nerve involvement, but this presentation remains rare with less than 20% of neurolisterioses [4]. The first descriptions of cases of rhombencephalitis were always fatal and reported necrotico-inflammatory microabscesses with perivascular lymphocytic linings [5]. Neurolisteriosis is confirmed by lumbar puncture which usually finds cellular fluid, polymorphic with hyperproteinarachia. Hypoglycorachia is only found in 30 to 50% of cases, and direct examination of cerebrospinal fluid only comes back positive in approximately a third of cases [6], which is comparable to the case we report or lumbar puncture. found pleocytosis with hyperproteinaxia, hypoglycaemia and a negative direct examination, which shows the importance of multiplex PCR which made it possible to make the diagnosis. First-line treatment includes a combination of amoxicillin and gentamicin [7,8]. Listeria monocytogenes is naturally resistant to cephalosporins. In case of allergy to beta-lactams, it is recommended to use the trimethoprim–sulfamethoxazole combination due to its very good diffusion in the central nervous system as well as in the intracellular compartment [9,10]. In our case, given the unavailability of the injectable form of amoxicillin, we used the trimethoprim-sulfamethoxazole combination as an alternative. This case of Listeria monocytogenes rhombencephalitis in an immunocompetent middle-aged man demonstrated that the disease can be easily misdiagnosed in this population. And highlight the importance of multiplex PCR which makes it possible to quickly distinguish viral infections from bacterial infections, thus favoring the implementation of a targeted therapeutic strategy with consequently low selection pressure on antibiotics and a better prognosis for the patient.
Conclusion
In conclusion, although Listeria meningitis is rare in immunocompetent individuals, it should be considered in the differential diagnosis, particularly in those who do not improve with cephalosporin-based antibiotic treatment. Rhombencephalitis develops rapidly and prompt diagnosis of L. monocytogenes is essential so that adequate antibiotic treatment can be initiated and better outcomes achieved.
References
- Schlech WF. (2019) Epidemiology and Clinical Manifestations of Listeria monocytogenes Infection. Microbiol Spectr. 7(3). [PubMed.]
- Charlier C, Perrodeau É, Leclercq A, Cazenave B, Pilmis B, et al. (2017) Clinical features and prognostic factors of listeriosis: the MONALISA national prospective cohort study. Lancet Infect Dis. 17(5): 510-519. [PubMed.]
- Mailles A, Lecuit M, Goulet V, Leclercq A, Stahl JP. (2011) National Study on Listeriosis Encephalitis Steering Committee. Listeria monocytogenes encephalitis in France. Med Mal Infect. 41(11): 594-601. [PubMed.]
- Magiar O, Vulpie S, Musuroi C, Marincu I, Murariu A, et al. (2022) Listeria Monocytogenes Meningitis in an Immunocompetent Patient. Infect Drug Resist. 15: 989-994. [PubMed.]
- Ashraf VV, Salam KA. (2021) Listeria Rhombencephalitis. J Neurosci Rural Pract. 12(2): 443-444. [PubMed.]
- Czupryna P, Zajkowska A, Garkowski A, et al. (2014) Listeria rhombencephalitis in an immunocompetent woman. Case Rep Neurol Med. 2014: 674321. [Ref.]
- Décard BF, Thöne J, Haghikia A, et al. (2017) Listeria rhombencephalitis mimicking a demyelinating event in an immunocompetent young patient. Mult Scler. 23: 123-125. [PubMed.]
- Zhang Y, Zang GQ, Tang ZH, et al. (2012) Listeria monocytogenes meningitis in an immunocompetent adult: a case report. Rev Soc Bras Med Trop. 45: 410-411. [PubMed.]
- Jubelt B, Mihai C, Li TM, Veerapaneni P. (2011) Rhombencephalitis / brainstem encephalitis. Curr Neurol Neurosci Rep. 11(6): 543-552. [PubMed.]
- Ricard D, Sallansonnet-Froment M, Defuentes G, de Greslan T, Bounolleau P, et al. (2008) Listeria monocytogenes abscess of the brain. Rev Neurol (Paris). 164(4): 388-393. [PubMed.]