>Corresponding Author : Ambadas Rathod
>Article Type : Case Report
>Volume : 4 | Issue : 6
>Received Date : 02 May, 2024
>Accepted Date : 16 May, 2024
>Published Date : 20 May, 2024
>DOI : https://doi.org/10.54289/JCRMH2400130
>Citation : Rathod A, Mann S, Bharadwaj N, Sandeep VS, Narendra S, et al (2024) Progressive Multifocal Leukoencephalopathy in HIV Patient– A Rare Case Report in India. J Case Rep Med Hist 4(6): doi https://doi.org/10.54289/JCRMH2400130
>Copyright : © 2024 Rathod A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access
1Junior Resident, Department of General Medicine, GMCH, Chandigarh
2Associate Professor, Department of General Medicine, GMCH, Chandigarh
3Senior Resident, Department of General Medicine, GMCH, Chandigarh
*Corresponding author: Ambadas Rathod, Junior Resident, Department of General Medicine, GMCH, Chandigarh
Abstract
PML is a rare opportunistic infection of the central nervous system in the PLHIV Patient. Here, we document a case report where a HIV-positive individual developed Progressive Multifocal Leukoencephalopathy (PML), caused by the reactivation of the John Cunningham virus (JCV) (which leads to the infection of the oligodendrocytes in the brain), Who presented to us with the complaint of the progressive decline in both consciousness and movement. Magnetic resonance imaging (MRI) revealed multiple irregular white-matter lesions in various brain regions which raise the suspicion of PML and the presence of JC viral DNA via the RTPCR in the cerebrospinal fluid (CSF) confirmed the diagnosis of PML. Hence, we suggest considering PML in these type of presentation as described above in HIV patients. While it is uncommon, Progressive Multifocal Leukoencephalopathy (PML) can occasionally be the initial sign of AIDS.
Abbreviations: PML: Progressive Multifocal Leukoencephalopathy, JCV: John Cunningham Virus, MRI: Magnetic Resonance Imaging, CSF: Cerebrospinal Fluid, CNS: Central Nervous System, HAART: Highly Active Antiretroviral Therapy
Introduction
Progressive Multifocal Leukoencephalopathy (PML) is a rare, severe, and often fatal demyelinating illness of the Central Nervous System (CNS) caused by the JC virus (JCV). The JC virus is a tiny, non-enveloped, double-stranded DNA polyomavirus belonging to the Polyoma viridae family. Its occurrence has notably increased during the AIDS epidemic. PML arises when the latent JC virus is reactivated in individuals with compromised immune systems [1]. Immunosuppressed people are susceptible to this virus, and the majority of them have advanced HIV infection. Sarcoidosis, autoimmune diseases, congenital immunological deficiencies, haematological and solid organ cancers, are the conditions that cause PML when HIV infection is not present. The most common symptoms include limb paresis, coordination issues, cognitive dysfunction, imbalanced gait, and sexual issues. In this condition, the optic nerves and spinal cord of the central nervous system are typically spared [2]. Around 85% of PML cases are linked to HIV. In developed countries before highly active antiretroviral therapy (HAART), PML was diagnosed in 2%–4% of HIV-infected patients. Despite the decline in other central nervous system diseases with HAART, PML incidence has decreased less significantly. PML occurrences in HIV patients are rare in developing nations like India. However, despite the start of the HAART, PML patients carry a poor prognosis and have high 6 month mortality, so it is crucial to consider PML in HIV-infected patients showing focal neurological impairments [1]. Presenting PML as the initial sign of AIDS is exceedingly rare in Indian literature, to the best of our knowledge.
Case Report
A 21 year old man was hospitalized in the male medical ward who was a reformed opioid {chitta} abuser since 6 months via iv route and the inhalational route for 9 months and a newly diagnosed PLHIV from the outside hospital, not on any treatment, presented to us with the complaint of the weakness of bilateral lower limbs since 15 days which was sub-acute in onset and progressive in nature, to such extent that he was not able to stand, bedridden for 10 days and associated with the bowel and bladder incontinence. He did not report any sensory loss, fever, vomiting, headache, loss of consciousness, head injury, seizures or ear discharge. Both parents (mother and father) of the patient are PLHIV. On examination the patient was afebrile, pulse rate was 88/minute{regular}, blood pressure was 100/60 mmHg on right arm, spo2 was 98 % on room air, random blood sugar was 83 mg/dl and respiratory rate was 16 cycles/ minute. He was conscious and oriented to time and person with GCS of E4V5M6. Bilateral pupils were equal and reactive to light. MMSE score was 17 and cranial nerve examination, sensory examination was within normal limits. On motor examination, increased tone in both upper and lower limbs and a power of 4/5 with hyperreflexia {+3} in all four limbs. Plantars were extensor bilaterally. There was no neck rigidity or meningeal signs and rest other systemic examination was within normal limits.
On presentation, the lab investigations revealed a normal biochemistry and hemogram. Patient’s HHH serology was s/o HIV-1 and HIV -2 positive by ELISA and hepatitis B and C were negative. CD4 count was 102/micro litre. Lumbar puncture was done for Cerebrospinal fluid (CSF) analysis which was acellular, total proteins-75 gm, glucose-74, ADA- nil. CSF for cryptococcal antigen, India ink, acid fast bacilli was negative. NCCT head was suggestive of hypo dense lesions in bilateral frontal lobes in the white matter of brain. CEMRI brain with whole spine screening revealed multifocal confluent and discrete areas of T2/FLAIR hyper intensity involving bilateral cerebral white matter with the involvement of subcortical U- fibres at places, midbrain, pons and medulla without diffusion restriction/blooming/enhancement. CSF was found to be positive for John Cunningham VIRUS (JCV) using JCV DNA PCR. Based on the patient’s clinical features, imaging findings, and JCV DNA PCR a diagnosis of PLHIV related Progressive multifocal leukoencephalopathy was made. Patient was started on ART regimen {Tenofovir/Dolutegrevir/Lamivudine} i.e. TLD regimen under NACO guidelines one tablet /day.
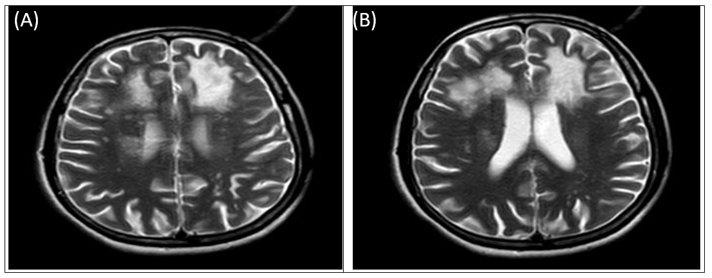
Figure 1 Magnetic Resonance Imaging results.
T2/FLAIR: Multifocal confluent discrete areas of hyperintensity involving B/L cerebral white matter.
Discussion
We report a case of a PLHIV patient who presented to us with the complaint of the progressive weakness and disturbance of the consciousness. Initially the weakness was in the bilateral lower limbs and bowel and bladder were also involved. Because of the history and NCCT head s/o hypo densities in bilateral frontal lobes, so the possibility of the tubercular meningitis with vasculitic infarct was kept. A negative CSF CBNAAT and the characteristic CEMRI brain finding of the T2/FLAIR hyper intensity in the white matter only raised the suspicion and positive CSF JC VIRUS PCR confirmed the diagnosis of the PML.
Since the emergence of the AIDS epidemics in 1981, the occurrence of PML has notably risen. In India, with over 5 million people living with HIV/AIDS, would seemingly have a notably high expected occurrence of PML within its HIV-infected population. Nevertheless, PML remains uncommon in India. Limited literature exists regarding HIV/AIDS with PML in developing nations like India. According to a study conducted at the All India Institute of Medical Sciences in Delhi, PML was found in 1.2% of patients visiting the ART clinic. This occurrence is less frequent in comparison to developed countries, where it has been documented in up to 5% of patients. The non-AIDS population affected by PML typically consists of middle-aged individuals who often have an underlying lymphoproliferative, myeloproliferative, or granulomatous disorder or are undergoing immunosuppressive therapy [1]. This is the first case registered under ART centre of GMCH Chandigarh.
The neurological manifestations of PML arise from the viral destruction of oligodendrocytes, responsible for producing myelin in the central nervous system. The primary pathological characteristics include atypical astrocytes with enlarged, multilobulated nuclei, and intranuclear inclusions in oligodendrocytes, identified as JC virus particles through in situ hybridization. Clinical symptoms involve progressive focal neurological dysfunction, commonly presenting as aphasia/dysarthria, monoparesis, hemiparesis, ataxia, cortical blindness, or visual field defects [3]. Most common initial manifestations are gait disturbances and cognitive impairment. Mental status changes like confusion, dementia, and in severe cases, coma, can occur. Seizures are rare (occurring in less than 10% of cases). Notably, there are no clinical signs of increased intracranial pressure or systemic infection [4].
MRIs of the brain have a high diagnostic value for PML. Single or multiple abnormal signals, round or sector-shaped, can be seen in the periventricular or subcortical white matter, which can be fused with one another and distributed asymmetrically. T2-weighted images and FLAIR reveal hyper intense areas, whereas T1-weighted images reveal hypo intense areas devoid of mass and enhancement. Lesions that extend to the subcortical/juxtacortical white matter are frequently seen on diffusion-weighted images, with peripheral patchy diffusion restriction [5]. Although histopathological evidence is the gold standard for PML diagnosis, the diagnosis is usually suggested by MRI and confirmed by CSF PCR for JCV DNA [6].
The majority of PML patients die within 6 months of clinical onset, and survivors are typically left with severe neurological sequelae [7]. Due to the lack of a specific treatment with proven efficacy, immune reconstitution remains the primary strategy. In PLHIV patients, ART should be started right away, and the regimen should be changed to optimise immune recovery and normalise CD4 counts. Other reported therapeutic strategies include recombinant IL-2, checkpoint inhibitors, and adoptive immunotherapy using virus-specific T cells [8].
In conclusion, for patients with AIDS who have hemiplegia, aphasia, and other CNS dysfunctions, comprehensive examination along with MRI brain and CSF analysis should be performed as soon as possible. When multiple asymmetric white matter lesions are found on MRI, and diffusion-weighted images show lesions extending to subcortical/juxta cortical white matter with peripheral patchy diffusion restriction, PML should be considered in differential diagnosis.
References
- Choudhary S, Parashar MK, Parashar N, Ratre S. (2018) AIDS-related progressive multifocal leukoencephalopathy-really rare in India: A case report and review of literature. Indian J Sex Transm Dis AIDS. 39(1): 55-58. [PubMed.]
- Hakamifard A, Shayganfar A, Khorvash F, Shaygannejad V, Tayeri K, et al. (2020) Progressive Multifocal Leukoencephalopathy as the First Manifestation of AIDS: A Rare Case Report. Arch Clin Infect Dis. 15(1): e85447. [Ref.]
- Saji AM, Gupta V. (2023) Progressive Multifocal Leukoencephalopathy. In: StatPearls Treasure Island (FL): StatPearls Publishing. [Ref.]
- Aksamit AJ. (2012) Progressive multifocal leukoencephalopathy. Continuum (Minneap Minn). 18(6 Infectious Disease): 1374-1391. [PubMed.]
- Shah R, Bag AK, Chapman PR, Curé JK. (2010) Imaging manifestations of progressive multifocal leukoencephalopathy. Clin Radiol. 65(6): 431-439. [PubMed.]
- McGuire D, Barhite S, Hollander H, Miles M. (1995) JC virus DNA in cerebrospinal fluid of human immunodeficiency virus-infected patients: predictive value for progressive multifocal leukoencephalopathy. Ann Neurol. 37(3): 395-399. [PubMed.]
- Anand P, Hotan GC, Vogel A, Venna N, Mateen FJ. (2019) Progressive multifocal leukoencephalopathy: A 25-year retrospective cohort study. Neurol Neuroimmunol Neuroinflamm. 6(6): e618. [PubMed.]
- Cortese I, Reich DS, Nath A. (2021) Progressive multifocal leukoencephalopathy and the spectrum of JC virus-related disease. Nat Rev Neurol. 17(1): 37-51. [PubMed.]