>Corresponding Author : Ziad Imane
>Article Type : Case Report
>Volume : 4 | Issue : 8
>Received Date : 09 May, 2024
>Accepted Date : 20 May, 2024
>Published Date : 30 May, 2024
>DOI : https://doi.org/10.54289/JCRMH2400137
>Citation : Younes B, Doha EK, Imane Z, Sara T, Mustapha B, et al. (2024) Radiation-Induced Breast Angiosarcoma Associated with Homolateral Axillary Recurrence: A Case Report. J Case Rep Med Hist 4(8): doi https://doi.org/10.54289/JCRMH2400137
>Copyright : © 2024 Younes B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access
1Professor in the Department of Gynecology and Obstetrics at the Ibno Rochd University Hospital in Casablanca, Morocco
2Resident Physician, Department of Gynecology and Obstetrics, at Ibno Rochd University Hospital, Casablanca, Morocco
*Corresponding author: Ziad Imane, Resident Physician, Department of Gynecology and Obstetrics, at Ibno Rochd University Hospital, Casablanca, Morocco
Abstract
Breast angiosarcoma is a rare aggressive tumor that develops from connective tissue of vascular origin with a tendency towards rapid recurrence and the appearance of visceral metastases. It occurs either as a primary tumor in young women or as a secondary tumor following breast irradiation. We report a case of breast angiosarcoma associated with homolateral axillary recurrence in a 45-year-old woman treated for bilateral breast cancer.
Keywords: Breast Angiosarcoma; Radiotherapy; Radiation-Induced Tumour
Abbreviations: MRI: Magnetic Resonance Imaging
Introduction
Breast angiosarcoma is a rare tumor, accounting for less than 1% of all soft tissue tumors of the breast [1]. that develops from connective tissue of vascular origin. It occurs either as a primary tumor in young women aged 30 to 40, or as a secondary tumor following breast irradiation as part of conservative treatment of breast cancer in older women [2].
Angiosarcoma is an aggressive tumor with a tendency towards rapid recurrence and the appearance of visceral metastases. Histological diagnosis is based on rigorous analysis of excisional specimens [1].
We report a case of breast angiosarcoma associated with homolateral axillary recurrence in a 45-year-old woman treated for bilateral breast cancer in the onco-gynecology department of the Ibn Rochd University Hospital, Casablanca. In this case, we describe the epidemiological, diagnostic and therapeutic aspects of this type of tumor.
Case Report
This is a 45-year-old female patient, nulligravida, nulliparous, who had presented at the age of 35 with bilateral infiltrating ductal carcinoma, she initially presented in the right breast: two well-limited lesions in the inferolateral quadrant measuring 14.5 x 10mm and 10 x 5 mm and a lesion in the superolateral quadrant measuring 15 x 10 mm with homolateral axillary adenopathy and, in the left breast: a lesion at the junction of the lower quadrants measuring 20 x 15mm with irregular contours. The extension work-up did not reveal any secondary metastatic location. The patient had undergone an initial right mastectomy with axillary lymphadenectomy, with the following anatomopathological report : healthy excision limits, RE +, RP +, HER2 (-) , 0 N+/13 N , (pT2N0M0), and a left lumpectomy with axillary lymphadenectomy, with the following anatomopathological report: healthy excision limits, RE +, RP +, HER2 (-), 0N+/10 N ,(pT2N0M0), followed by 6 courses of adjuvant chemotherapy consisting of 3 sessions of AC60 (Adriamycin / Cyclo-phosphamide), then 3 sessions of Taxane.
In order to complete the treatment, external radiotherapy was indicated (50 Gy over the mammary gland, internal mammary chain and the right and left supra-clavian region, with 15 Gy superimposed on the left tumor bed). Anti-estrogen hormone therapy was prescribed for 5 years, due to the positivity of hormone receptors.
The patient was monitored regularly. Ten years after conservative locoregional treatment, the patient presented with a self-examination of a mass in the left breast that was progressively increasing in volume, with inflammatory signs in the irradiated breast. Clinical examination of the irradiated breast revealed a large, hard mass in the upper and lower quadrants, with signs of inflammation (Figure 1). An echomammography revealed a solid-cystic mass covering the entire left breast (Figure 2). A breast MRI revealed a highly suspicious left breast mass measuring 7 x 5cm, and an ultrasound-guided biopsy led to the diagnosis of angiosarcoma.
The extension work-up found no distant secondary lesions. The patient received neoadjuvant chemotherapy with 3 courses of AI (Anthracycline and Isofosfamide), followed by radical mastectomy with exploration of the the axilla. Pathological analysis (Figure 3) confirmed the diagnosis of high-grade breast angiosarcoma according to Donnel's grading, with a tumor size of 11.5 x 8 cm and no infiltration at the base of the nipple. The resection margins were greater than 1cm with a 1N+/2N compatible with regional recurrence of invasive breast carcinoma, SBR II, luminal B, HER2 (-).
Post-operative follow-up was simple, and adjuvant chemotherapy based on Anthracycline and Isofosfamide was indicated at a multidisciplinary consultation meeting. The patient is currently still undergoing chemotherapy and is regularly monitored in our training center.

Figure 1. A mass covering the whole breast, mobile/deep level, fixed/superficial level

Figure 2. Echomammographic appearance of the mass
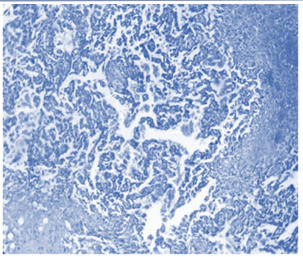
Figure 3. Vascular cavities of variable size, irregularly anastomosed and filled with red blood cells (arrows) (haematein-eosin stain)
Discussion
Angiosarcoma of the breast has also been called hemangiosarcoma, haemangioendotheliosarcoma, hemangioblastoma, angioblastoma, malignant hemangioendothelioma [1]. It is a rare tumor representing 0.04% of all malignant breast tumors and 8-10% of breast sarcomas, and may be either primary or secondary as an exceptional complication of radiotherapy [3].
Primary angiosarcoma generally presents as a palpable mass that progressively increases in volume, and may be associated with hemorrhagic manifestations of Kasabach-Merrit syndrome [4]. Secondary angiosarcoma may present as a large mass, generally between 2 and 11 cm in size, with an average of 5.3 cm [5], with a purplish, angiomatous appearance of the skin around the tumor, as seen in our case, or a painless, often multifocal ecchymosis, eczematous rash or hematoma-like swelling.
An echomammography does not show the pathognomonic features of adenocarcinoma in angiosarcoma, and nodules, particularly in young women, may be misclassified as benign. Although there is evidence that mammographic findings may raise suspicion of this diagnosis [6], on ultrasound these nodules may appear heterogeneously echostructured with both hyper- and hypoechogenic areas, with low attenuation of the ultrasound beam as reported in our cases. The contribution of color Doppler is more interesting because it highlights the vascular nature of the tumor. It thus replaces the more invasive arteriography, whose only interest remains preoperative embolization to reduce the significant risk of hemorrhage in large tumors. Numerous studies have demonstrated the ability of magnetic resonance imaging (MRI) to identify patterns of malignancy in angiosarcoma.
The diagnosis is often made by histopathological analysis of the lesions, which reveals irregular vascular formations and irregular, hyperchromatic nuclei. Immunohistochemistry is a valuable aid, confirming the vascular nature of the proliferation with CD31, CD34 and factor VIII antibodies, and the negativity of cytokeratin. However, these vascular markers may be absent in poorly differentiated forms [7].
The metastatic spread of angiosarcoma is thought to be primarily haematogenous; however, cases of lymphatic spread have also been reported [8].
Surgery remains the optimal treatment for angiosarcoma. Breast-conserving therapy has been used, but is only recommended for small lesions with healthy margins (a margin of >2 cm). Total mastectomy alone or with axillary dissection is the optimal surgical treatment. The need for axillary lymph node dissection is currently unclear, as lymph node metastases are not common in angiosarcomas. In our case, surgical exploration of the axilla revealed a palpable lymph node, which on anatomopathological examination came back in favor of a regional recurrence of invasive breast carcinoma. Some studies suggest that treatment with anthracycline-based chemotherapy may improve both disease-free survival and overall survival. Radiotherapy has been used in the adjuvant treatment of breast sarcoma to improve locoregional control after surgical excision and survival [9].
The prognosis of angiosarcoma depends on the grade of the tumor and the surgical margins. The local recurrence rate was 92% and the median survival time for patients who underwent complete or incomplete excision was 42 and 6 months respectively [10].
Conclusion
Angiosarcoma of the breast is a rare malignant tumor, but a fearsome one after radiotherapy during conservative treatment. It is diagnosed histologically on the entire surgical specimen. Its prognosis is very poor, and only early surgery with or without axillary lymph node dissection offers hope of longer survival. The role of chemotherapy and radiotherapy remains to be demonstrated.
Patient's consent: Written informed consent was obtained from the patient for publication and any accompanying images.
References
- Bobin Y, Dolbeau B, Bernard C, Mignotte H, Rivoire M, et al. (1991) Angiosarcome du sein: à propos de quatre cas avec revue de la littérature. Bull Cancer. 78: 1037-1044. [PubMed.]
- De Bree E, Van Coevorden F, Peterse JL, Russel NS, Rutgers EJT. (2002) Bilateral angiosarcoma of the breast after conservative treatment of bilateral invasive carcinoma: genetic predisposition? Eur J Surg Oncol. 28: 392-395. [PubMed.]
- Chouchou L, et al. (2003) Les angiosarcomes du sein: à propos de trois observations. Ann Chir. 128: 43-48. [Ref.]
- Ernathova M, Jaschke W, Pechlahner C, et al. (2006) Primary angiosarcoma of the breast associated Kasabach-Merritt syndrome during pregnancy. Breast. 15: 255-258. [PubMed.]
- Antman KW, Corson J, Greenberger J, Wilson R. (1982) Multimoda- lity therapy in the management of angiosarcoma of the breast. Cancer. 50: 2000-2003. [PubMed.]
- Moore A, Hendon A, Hester M, et al. (2008) Secondary angiosarcoma of the breast: can imaging findings aid in the diagnosis? Breast J. 14: 293-298. [PubMed.]
- Antman KW, Corson J, Greenberger J, Wilson R. (1982) Multimodality therapy in the management of angiosarcoma of the breast. Cancer. 50: 2020-2023. [PubMed.]
- Losanoff JE, Jaber S, Esuba M, et al. (2006) Primary angiosarcoma of the breast: do enlarged axillary nodes matter? Breast J. 12: 371-374. [PubMed.]
- Fodor J, Orosz Z, Szabó E, et al. (2006) Angiosarcoma after conservation treatment for breast carcinoma: our experience and a review of the literature. J Am Acad Dermatol. 54: 499-504. [PubMed.]
- Jallali N, James S, Searle A, et al. (2012) Surgical management of radiation-induced angiosarcoma after breast conservation therapy. Am J Surg. 203: 156-161. [PubMed.]