>Corresponding Author : Sabir Soukaina
>Article Type : Case Report
>Volume : 4 | Issue : 9
>Received Date : 05 June, 2024
>Accepted Date : 21 June, 2024
>Published Date : 24 June, 2024
>DOI : https://doi.org/10.54289/JCRMH2400144
>Citation : Soukaina S, Fadwa A, Hajar E, Imane Z, Asmaa A, et al. (2024) A rare case of necrotic sigmoid volvulus complicating the postpartum period. J Case Rep Med Hist 4(9): doi https://doi.org/10.54289/JCRMH2400144
>Copyright : © 2024 Soukaina S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access
1Resident Physician, Department of Gynecology and Obstetrics, at Ibn Rochd University Hospital, Casablanca, Morocco
2Professor in the Department of Gynecology and Obstetrics at the Ibn Rochd University Hospital in Casablanca, Morocco
*Corresponding author: Sabir Soukaina, Resident Physician, Department of Gynecology and Obstetrics, Ibno Rochd University Hospital, Casablanca, Morocco
Abstract
Sigmoid volvulus is a rare complication of pregnancy and the puerperium. We report a case of sigmoid volvulus complicating the postpartum period in a 35-year-old patient who presented on day 5 postoperative of a cesarean section performed in the EL HAROUCHI maternity at the Ibno Rochd university Hospital of Casablanca, in a table of occlusive syndrome. The diagnosis was made by an abdominopelvic CT. Exploratory laparotomy revealed a necrotic volvulus of the highly distended sigmoid colon. In our case, the sigmoid volvulus was probably precipitated by the rapid change in uterine size after delivery.
Therefore, a surgical evaluation of an acute abdomen in the postpartum period is essential, because the delayed diagnosis and treatment can lead to significant maternal morbidity and mortality.
Keywords: Necrosis, Volvulus, Sigmoid, Postpartum, Surgery
Introduction
The sigmoid volvulus is a rare complication of pregnancy requiring immediate surgical intervention. It is thought to be the second most common cause of volvulus after bridge occlusion. It is difficult to diagnose and its prognosis depends largely on early treatment [1]. Sigmoid volvulus, the leading cause of colonic volvulus, corresponds to torsion of the sigmoid around its meso with a degree of rotation varying from 180 to 360◦ [2], responsible of a mechanical occlusion. We report the case of a 35 years old patient admitted on day 5 after a cesarean section with a table of an occlusive syndrome, with a necrotic sigmoid volvulus complicating the postpartum period.
Case Report
Mrs KA, 35 years old, with no previous pathological history, was admitted on day 5 post caesarean section performed for a non-reassuring foetal condition, giving birth to a female , Apgar 8/10, birth weight 3200g in an unmonitored pregnancy presumed at term, with an occlusive syndrome consisting in diffuse abdominal pain that had been evolving for two days, associated with abdominal distension and an absence of solid matter and gas.
Physical examination revealed an altered general condition with a fever of 38.5°C, blood pressure of 80/60 mm Hg, pulse of 110 beats per minute and respiratory rate of 20 cycles per minute. Abdominal examination revealed significant meteorism with tympany and diffuse abdominal tenderness. On rectal examination, the rectal ampulla was empty. The gynaecological examination revealed a clean caesarean section scar, minimal lochia, and a uterus that was difficult to assess due to abdominal distension. The unprepared abdomen (UA) showed very significant colic distension with a double gas arch (Figure 1).
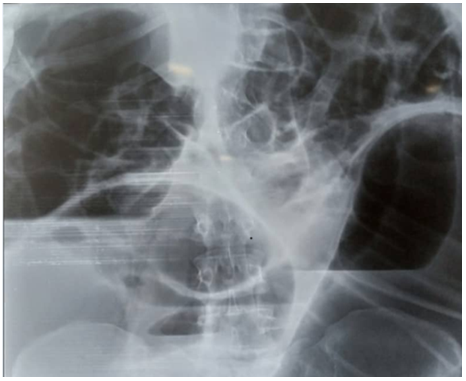
Figure 1. Unprepared abdomen showing the ‘inverted U’ image
Abdominopelvic CT scan with injection of contrast medium showed significant distension of the ascending and transverse colon, with hydroaerosic levels upstream of a transitional level, creating a beak-like appearance with visualization of a turn of spiral in the mesentery, and the descending colon and gallbladder coves collapsed (Figure 2).
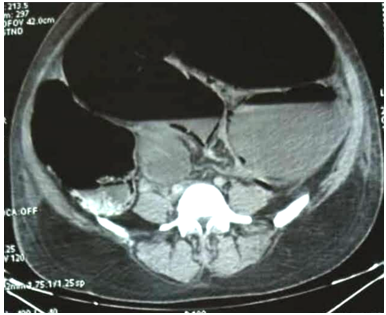
Figure 2. an axial scan demonstrating a ‘bird's beak’ appearance
Biological results showed a hyperleukocytosis of 28950 elements/mm3 and a CRP of 320 elements. The diagnosis of mechanical colonic obstruction due to organo-axial sigmoid volvulus was accepted, and surgical exploration was required. After a midline laparotomy and aspiration of 300 ml of fetid brownish fluid, the investigation revealed enormous colonic distension (Figure 3) with a mesenteric-axial sigmoid volvulus with clockwise rotation, sigmoidal necrosis (Figure 4) and the presence of a few false membranes between the ossicles. We performed a sigmoidectomy, removing the necrotic sigmoid (Figure 5 A and B), closing the rectal tip and performing a Hartmann left colostomy.
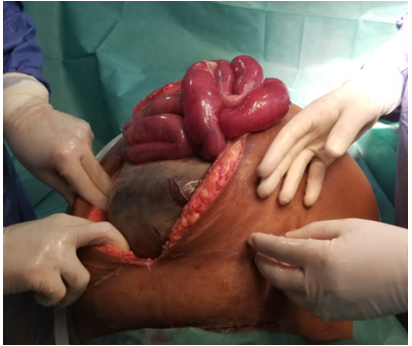
Figure 3. Enormous gallbladder and colic distension
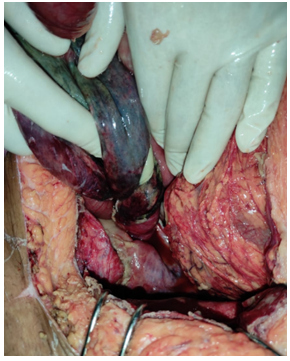
Figure 4. Clockwise rotation with sigmoid necrosis
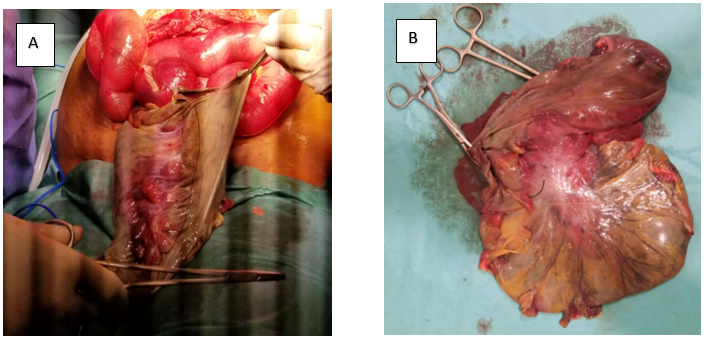
Figure 5A: A sigmoidectomy removing the necrotic sigmoid.
Figure 5B: A sigmoidectomy specimen
Discussion
Volvulus of the sigmoid represents the most common aetiology of antepartum bowel obstruction [3,4]. Volvulus in the postpartum period, as in our case, is extremely rare, but the risk is thought to be increased by colonic distortion resulting from rapid change in uterine size after delivery [5]. Circumferential torsion of an intestinal segment around its mesenteric origin, if left untreated, can progress to intestinal ischaemia and perforation [3].
The aetiology of colonic volvulus is probably multifactorial. Certain factors are common to the location of the volvulus, such as chronic constipation, a high-fibre diet, frequent use of laxatives, a history of laparotomy and anatomical predispositions; for example, the dolicho-sigmoid is the factor most often cited as predisposing to sigmoid volvulus [6].
In sigmoid volvulus, a torsion of the mesosigmoid of less than 180◦ is considered physiological. In around 2% of cases, the volvulus reduces spontaneously. Beyond this angle of torsion, complications arise leading to occlusion, ischaemia or even colonic necrosis and perforation. For unknown reasons, in 70% of cases the torsion is counter-clockwise [7].
In the case of a sigmoid volvulus, colonic distension leads to an increase in intra-luminal pressure, which in turn leads to a reduction in digestive capillary perfusion, aggravated by mechanical phenomena of compression and axial rotation (‘twisting’) of the mesosigmoid vessels [8] .This early colonic mucosal ischaemia encourages bacterial translocation, which increases colonic distension and toxic phenomena. This creates a vicious circle which, if untwisting or not carried out early, leads to colonic necrosis, inducing ischaemia [9].
The clinical presentation is that of a distal colonic obstruction, with sudden abdominal pain predominating in the left iliac fossa, early cessation of bowel movements and gas with meteorism , sometimes masked by diarrhoeal stools due to emptying of the distal segment , nausea and vomiting are delayed [10]. However, these symptoms are common in the post-partum period, especially after a caesarean section, and are not specific. The uterus, cervix and adnexa share the same visceral innervations as the terminal ileum, sigmoid, colon and rectum, so differentiating between a gynaecological or gastrointestinal origin of the pain can be difficult [11]. In addition, abdominal distension may be a late and unreliable finding in postpartum volvulus; associated abdominal tenderness and, if detected, may be interpreted as fundal tenderness as the obstructed bowel is usually posterior to the enlarged uterus [12]. The clinical picture may be confused with postpartum endometritis, but signs of peritonitis and sepsis suggest ischaemia of the volvular segment. The symptoms suggestive of severity include dehydration, shock and cardiorespiratory decompensation [10].
Biological tests do not point to a diagnosis. They merely reflect the occlusive syndrome and any infectious syndrome: fluid and electrolyte disorders (hypokalaemia, functional renal failure), hyperleukocytosis, inflammatory syndrome, and even haemostasis disorders in necrotic forms [6]. The standard radiograph (unprepared abdomen), with visualisation of the classic ‘inverted U’ image, is no longer indicated; it was performed in our case given the postoperative context to rule out an ogilvie syndrome. The French National Authority for Health recommends an abdominopelvic CT scan as a first-line procedure as soon as possible [13]. It has a sensitivity of close to 100% and a specificity of over 90% for the positive, topographical and aetiological diagnosis of occlusion [14,15].
A portal abdominopelvic CT scan with injection of contrast product confirms the diagnosis with the presence of a U-shaped loop, the two legs of which converge towards the point of torsion, giving a ‘coffee bean’ shape on frontal reconstructions, with a ‘whirl sign’ corresponding to the mesocolon wrapping around the point of torsion, visible on axial and coronal sections [16]. It can also be used to show indirect signs so as the dilatation of the upstream colon or even the small intestine, distal colon and non-aerated rectum, identification of the flat loop-dilated loop transition zone and to eliminate the differential diagnoses.
The treatment of the volvulus involves stopping feeding, performing upper gastrointestinal suctioning and restoring fluid and electrolyte balance. As an emergency measure, in the absence of serious signs (digestive perforation, ischaemia), treatment is based on endoscopic detorsion of the volvulated segment, with colonic exsufflation and insertion of a Faucher tube to limit the risk of recurrence in the short term [17].
The type of surgical treatment is controversial [18]. In immediately complicated forms (colonic necrosis, perforation, shock), colonic colectomy and resection, usually without restoration of continuity, is necessary [6].
Mortality associated with sigmoid volvulus is estimated at between 7 and 20% [10]. The most important prognostic factor is the delay in management, as the natural course is towards digestive ischaemia, colonic infarction and peritonitis [19]. In cases of perforation or ischaemia, the postoperative mortality rate is as high as 40% [20].
Conclusion
The Sigmoid volvulus is a medical and surgical emergency, affecting the sigmoid colon in 60-75% of cases. It is difficult to diagnose in the immediate post-partum period. The increased volume of the abdomen and the difficulty in obtaining abdominal signs (due to loss of tone in the abdominal wall) may mask the signs of peritonitis.Abdominopelvic scans are necessary for a proper diagnosis and to assess the severity of the condition . In complicated forms, colonic colectomy and resection, usually without restoration of continuity, are required.
References
- Iwamoto I, Miwa K, Fujino T, Douchi T. Perforated colon volvulus coiling around the uterus in a pregnant woman with a history of severe constipation. J Obstet Gynaecol Res. 2007;33(5):731-3. [PubMed.]
- Bernard C, Lubrano J, Moulin V, et al. Apport du scanner multi-détecteurs dans la prise en charge des volvulus du sigmoïde. J Radiol. 2010;91:213-20. [Ref.]
- Aftab Z, Toro A, Abdelaal A, et al. Endoscopic reduction of a volvulus of the sigmoid colon in pregnancy: case report and a comprehensive review of the literature. World J Emerg Surg. 2014;9:41. [Ref.]
- Khan MR, Rehman S. Sigmoid volvulus in pregnancy and puerperium: a surgical and obstetric catastrophe. Report of a case and review of the world literature. World J Emerg Surg. 2012;7(1):10. [PubMed.]
- Dua RS, Rothnie ND, Gray EA. Sigmoid volvulus in the puerperium. Int J Gynaecol Obstet. 2007;97(3):195. [PubMed.]
- Perrot L, Fohlen A, Alves A, Lubrano J. Volvulus du côlon: quelle prise en charge en 2016? J Chir Visc. 2016;153(3):188-98. [PubMed.]
- Shepherd JJ. The epidemiology and clinical presentation of sigmoid volvulus. Br J Surg. 1969;56:353-9. [PubMed.]
- Altarac S, Glavas M, Drazinic I, et al. Experimental and clinical study in the treatment of sigmoid volvulus. Acta Med Croatica. 2001;55:67-71. [PubMed.]
- Lubrano J, Paquette B, Delabrousse E, Koch S, Mantion G. Volvulus du sigmoïde. EMC Gastroenterol. 2012:1-6. [Ref.]
- Rothmann C, Pierrard O, Schmutz T. Volvulus du sigmoïde: diagnostic et traitement en urgence. J Eur Urg Réanim. 2018;30(1-2):41-5. [Ref.]
- Augustin G, Majerovic M. Non-obstetrical acute abdomen during pregnancy. Eur J Obstet Gynecol Reprod Biol. 2007;131(1):4-12. [PubMed.]
- Atamanalp SS, Kisaoglu A, Ozogul B, et al. Sigmoid volvulus complicating pregnancy: a case report. Eurasian J Med. 2015;47(1):75-6. [Ref.]
- Principales indications et non-indications de la radiographie de l’abdomen sans préparation; 2009. p. 1-28. [Ref.]
- Atamanalp SS. Treatment of sigmoid volvulus: a single-center experience of 952 patients over 46.5 years. Tech Coloproctol. 2013;17:561-9. [PubMed.]
- Atamanalp SS, Ozturk G. Sigmoid volvulus in the elderly: outcomes of a 43-year, 454-patients experience. Surg Today. 2011;41:514-9. [PubMed.]
- Wai CT, Lau G, Khor CJ. Clinics in diagnostic imaging: sigmoid volvulus causing intestinal obstruction, with successful endoscopic decompression. Singapore Med J. 2005;46:483-7. [PubMed.]
- Perrot L, Fohlen A, Alves A, et al. Management of the colonic volvulus in 2016. J Visc Surg. 2016;153:183-92. [PubMed.]
- Kasten K, Marcello P, Roberts P, et al. What are the results of colonic volvulus surgery. Dis Colon Rectum. 2015;58:502-8. [PubMed.]
- Dulger M, Canturk NZ, Utkan NZ, et al. Management of sigmoid colon volvulus. Hepatogastroenterology. 2000;47:1280-3. [PubMed.]
- Raveenthiran V, Madiba TE, Atamanalp SS, et al. Volvulus of the sigmoid colon. Colorectal Dis. 2010;12:712. [PubMed.]