>Corresponding Author : Edgard Michel-Crosato
>Article Type : Research Article
>Volume : 1 | Issue : 2
>Received Date : 6 December, 2021
>Accepted Date : 27 December, 2021
>Published Date : 30 December, 2021
>DOI : https://doi.org/10.54289/JDOE2100110
>Citation : Negreiros RA, Crosato M. (2021) Third Molar: Position, Caries, Periodontal Disease, and Quality of Life. J Dent Oral Epidemiol 1(2): doi https://doi.org/10.54289/JDOE2100110
>Copyright : © 2021 Negreiros RA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Research Article | Open Access
1Postgraduate program in Biophotonics Applied to Health Sciences, University Nove de Julho, UNINOVE, São Paulo, Brazil 2FFO_FOUSP Fundação para o Desenvolvimento Científico e Tecnológico da Odontologia University of São Paulo, FFO-USP, Specialization course in oral maxillofacial surgery São Paulo, Brazil 3Master degree student, program in Biophotonics Applied to Health Sciences, University Nove de Julho, UNINOVE, São Paulo, Brazil 4Dentist in Advanced Geriatrics Center (NAGe), Syrian Lebanese Hospital, São Paulo, Brazil 5Associate professor, Department of Community Dentistry, São Paulo University (FOUSP), São Paulo, Brazil 6Integrated Clinic, Department of Estomatology, São Paulo University (FOUSP), São Paulo, Brazil
*Corresponding author: Crosato M, Department of Community Dentistry, Dentistry School, University of São Paulo (FOUSP), Avenida Professor Lineu Prestes, 2227, Cidade Universitária, CEP 05508-000, São Paulo (SP), Brazil
Abstract
Third molar teeth (3M) can lead to periodontal disease (PD) and caries and can also have a significant impact on oral health-related quality of life (QoL). The aim of this study was to verify associations between QoL, PD, carious lesions, and the position of the mandibular 3M. An observational cross-sectional study was conducted in 116 patients (228 teeth), with the approval of the ethics committee (280084) of the University of São Paulo Dental School and registered on Clinicaltrials.gov (NCT04024644). Caries were assessed by visual tactile examination and PD by probing sites around 3M. The evaluation of QoL was carried out using the Oral Health Impact Profile questionnaire (OHIP-14). The evaluation of the 3M’s position was performed according to the classification of Pell/Gregory and Winter. Data were analyzed according to STATA13.0, with a 95% level of significance; the higher degree of eruption and angulation of the 3M increased the incidence of PD and caries in these teeth. Patients with caries had an impact on domains 1 and 7, and those with PD had an impact on domains 2 and 7. The position of the 3M influences the incidence of caries and PD in 3Ms, with consequent negative impacts on QoL.
Keywords: Teeth, Wisdom, Dental Caries, Periodontal Disease, Health-Related Quality of Life
Abbreviations: PD: Periodontal Disease, QoL: Quality of Life, OHIP-14: Oral Health Impact Profile Questionnaire, 3Ms: Third Molars, 2M: Second Molar, OHRQoL: Oral Health-Related QoL
Introduction
The third molars (3Ms) are teeth with limited function [1] and a high index of associated diseases [2]. Among them, caries, and periodontal disease (PD) are chronic oral cavity conditions that affect most of the young adult population [3]. Caries is a contagious infectious disease associated with the interaction of many risk factors and is considered multifactorial [4]. It is one of the leading causes of dentition loss in the first decades of life [3]. Some factors influence the occurrence of caries, such as education level, oral hygiene level, brushing frequency, water supply, frequency of visits to the dentist [5], and socioeconomic conditions [3]. Diet is also a modifying factor. The position of the 3Ms and the patient’s anatomical profile can lead to the identification of caries risk groups in the 3Ms [6].
Periodontal disease is an inflammatory disorder with a specific localized infection that affects one or more support or protection tissues, including alveolar bone, periodontal ligament, cementum, and/or gingiva [5]. An increased depth of the periodontal pocket is a cause of PD in the 3M region [7], also to the worsening of periodontal condition between the second molar (2M) and 3M [8].
The position, angle, and degree of impaction of the 3Ms can influence the pathological changes in the 3Ms. These factors should be considered when considering extraction [9]. The higher the angulation of the tooth, the greater the difficulty of sanitizing and removing food, consequently facilitating bacterial colonization [10]. Often, the presence of these teeth can lead to a decrease in an individual's oral health, having a significant impact on their quality of life (QoL). Patients may report difficulty relaxing, interruptions in eating, irritability, and tension [11].
The purpose of this study was to verify the possible associations between oral health-related QoL (OHRQoL), the position of the mandibular 3Ms, and the occurrence of caries and PD.
Methods
The study was approved by the ethics committee of the University of São Paulo Dental School (number 280084) and registered at clinicaltrials.gov (number NCT 04024644).
Patients who agreed to participate in this study signed the informed consent form after a verbal and written explanation of the research. We conducted an observational study with 116 healthy patients (228 mandibular 3Ms) of both sexes during the specialization course of oral and maxillofacial surgery at the FFO-University of SãoPaulo, Brazil. Data were collected over 12 months.
Sample Size Calculation
The sample size was calculated (G * Power software version 3.1.9.2) using the t-test for paired groups. The effect size was determined using the formula described below.
The worst scenario was selected, that is, the largest standard deviation between means. The mean values of the control and treated groups, as well as the standard deviation, were taken from one study [12]. The error was set at 5% and the power test at 95%. This value was calculated to provide 95% strength (a = 0.05). According to the result, a sample of 116 patients was necessary to detect differences in QoL [12]. Other factors related to secondary outcomes were statistically analysed.
Inclusion and Exclusion Criteria
Participants in this study were evaluated to meet the eligibility criteria: ASA I patients (negative medical history), with at least one 3M erupted or partially erupted. All participants, regardless of age, sex, cultural level, or socioeconomic status, were allowed to participate in the study.
Patients with the following were excluded: systemically compromised, allergies, pregnancies, and four 3Ms impacted or had already undergone the exodontia of one of them.
Outcome Measures
The outcome measures were sex, age, carious lesions, periodontal disease, 3M position, and OHRQoL.
Sex and age were assessed on a clinical form, including personal and demographic data, reasons that led to seeking care, and the last visit to the dentist. Caries were evaluated by visual tactile examination only on the occlusal surface in the erupted or partially erupted 3Ms (visual tactile examination) and by the image on the panoramic radiograph.
We considered the presence of a caries when cavities or radiolucency were present [13]. Periodontal disease was evaluated by probing the gingival sulcus in 3Ms at two points: mesiobuccal and distobuccal regions. We considered the presence of PD when the pocket was ≥ 4 mm [14]. The position and classification of the mandibular 3Ms were assessed by panoramic radiography, according to the classification of Pell and Gregory (1942) and Winter (1926) [15] performed by the same evaluator, following the criteria of imaginary lines, as proposed by Almendros-Marques, et al. [16] OHRQoL was assessed using the Brazilian version of the OHIP-14 questionnaires [17] (Table 1) and applied as an interview. This instrument consists of 14 items rated on a Likert-type scale that includes the following responses: never (coded 0), hardly ever (coded 1), occasionally (coded 2), fairly often (coded 3), and very often (coded 4). The results of the OHIP-14 questionnaire ranged from 0 to 56, with higher scores indicating poor OHRQoL [18]. The results were also evaluated by domains. The answers were arranged on seven subscales: Domain 1 (functional limitation), domain 2 (physical pain), domain 3 (psychological discomfort), domain 4 (physical disability), domain 5 (psychological disability), domain 6 (social disability), and domain 7 (handicap).
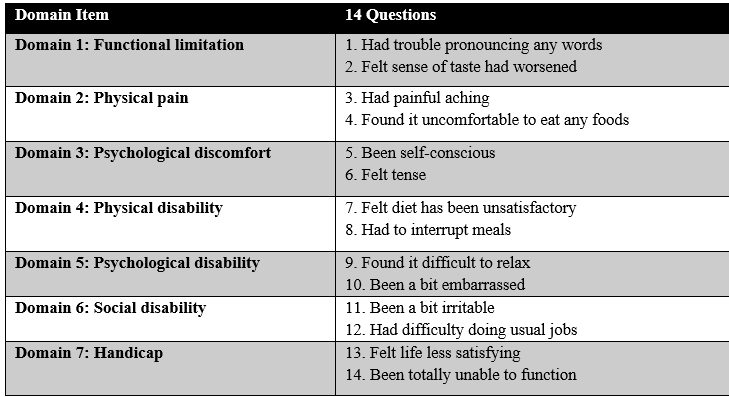
Table 1: Ohip-14 questionnaire and its domains
Data Analysis
Data were treated according to the software program Stata 13.0 (Stata Corp, College Station, TX). Variables were evaluated using split-plot analysis of variance for repeated measures analysis to identify associations between QoL and positions of the mandibular 3M. A 95% significance level was used for all the analyses.
The results of the OHIP-14 questionnaire were evaluated by the domain averages and the impact in each of them, considering the presence of impact when the response was greater than zero.
Results
Sex and Age:
During the study, questionnaires were administered to 117 patients, but one of them was excluded due to incomplete data. The number of patients evaluated was 116, which corresponds to 228 mandibular 3Ms.There were 63 female patients (54.31%) and 53 male patients (45.69%), with a mean age of 25.25 years (SD, 5.06 years).
Carious Lesions and PD:
Upon assessing the presence of caries in the 3Ms of the mandible, it was found that 58.62% had no carious lesions, 1.72% had no anodontia, and 7.76% were enclosed (i.e., partially covered by soft or hard tissue). The presence of carious lesions was detected clinically or radiographically in 28.02% of the samples, and 3.88% of the teeth were obturated, which adds up to 31.9% of the teeth being clinically or radiographically detected (Table 2). Among the 228 3Ms mandibular evaluated in this study, 18.53% had periodontal probing depths deeper than 4 mm (periodontal pocket), 72.41% did not have periodontal pockets, and 7.46% had enclosed teeth (Table 2).
Position:
Among the 228 teeth, 54.74% were partially erupted, 35.78% erupted, and 35.78% were impacted. According to the Winter classification, most teeth were in a vertical position (60.34%), followed by mesioangular (18.97%) and horizontal (14.66%) positions. According to Pell and Gregory’s classification, 183 teeth were in position A (78.87%), followed by position B (17.24%); 100 (43.10%) of the teeth were classified as class II; and 40 (17.24%) as class I (Table 3).
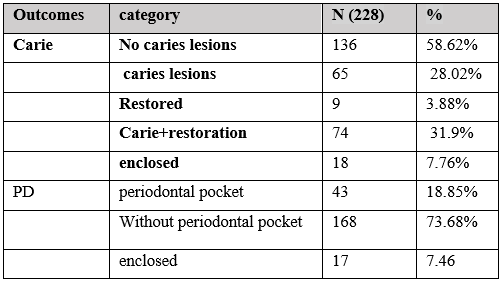
Table 2: Lower 3Ms according to caries lesions presence and PD
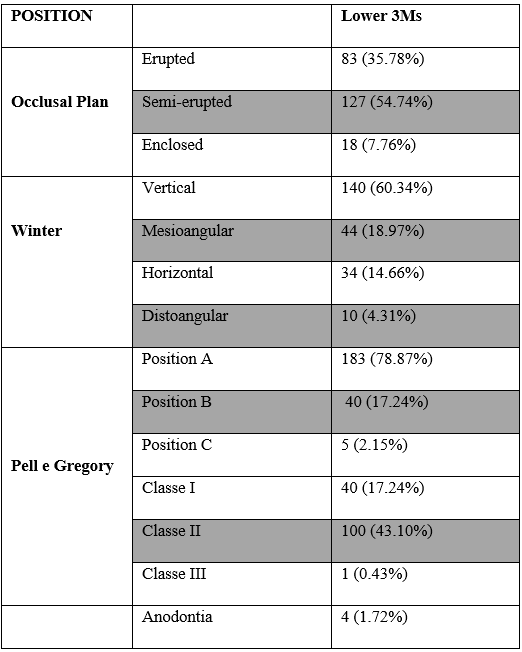
Table 3: Patients distribution according to Winter. Pell e Gregory and occlusion relation.
Caries, PD, Age, and Position:
The older patients had 4% more carious lesions and increased PD, showing statistical significance (p = 0.00 carries and p = 0.01 PD) (Table 4).
Regarding the occlusal plane, the erupted mandibular 3Ms presented two times more carious lesions than partially erupted ones, with statistical significance (p = 0.00). The mandibular 3Ms that erupted had 60% more PD than partially erupted teeth, without a statistically proven relationship (Table 4).
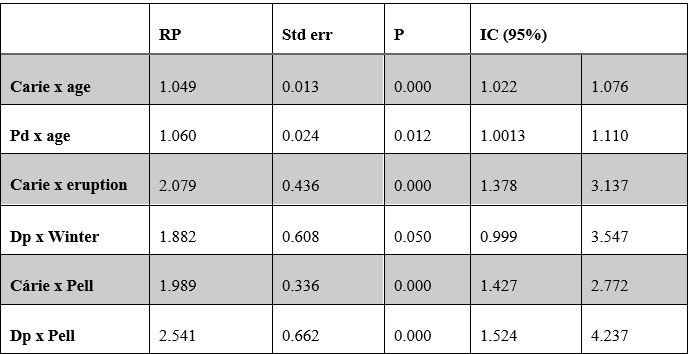
Table 4: Patients distribution according to caries and Pd, age and position.
Regarding Winter´s classification, the mandibular 3Ms in the distoangular position had less caries than the mesioangular ones. The mesioangular teeth had 10% more caries than the vertical teeth, and more caries than the horizontal teeth (p = 0.00) (Table 4). The mandibular 3Ms mesioangular teeth had more PD than the vertical teeth, with a statistically significant difference (p = 0.05) (Table 4).
Regarding Pell and Gregory´s classification (positions A, B, and C), the mandibular 3Ms at position B had twice as many carious lesions as position A; position C had 25% more carious lesions than position A, with statistical significance. Position B had more PD than in position A; position C had more PD than position A, with statistical significance (p = 0.00) (Table 4).
QoL:
Among the 116 patients, the mean total OHIP questionnaire was 12.13 (0-51). Regarding the evaluation of domains, we obtained: domain 1 (functional evaluation) 0.27; domain 2 (physical pain) 1.77, (impact); domain 3 (psychological discomfort) 1.61, (impact); domain 4 (physical disability) 0.75; domain 5 (psychological incapacity) 0.71; domain 6 (social incapacity) 0.85; domain 7 (social disadvantage) 0.34.
The average total OHIP was similar in all patients, in the presence or absence of carious lesions in the mandibular 3Ms. When QoL was evaluated by analysing domains, a relationship was found between caries and QoL in domains 1 (p = 0.04) and 7 (p = 0.00) (Table 5). Patients with PD in 3Ms had more impact in domain 2 (physical pain) (p = 0.03) and domain 7 (handicap) (p = 0.04) than in patients without diseases (Table 5).
Considering the presence of caries or PD, 3Ms with pathological occurrence, patients who have PD or caries had higher scores of OHIP in domain 7 (handicap/social disadvantage) (p = 0.06) (Table 5).
Discussion
The associations between QoL, PD, caries, and position of the mandibular 3Ms were verified in this study.
• The 3M position, such as angulation and degree of eruption, interferes with carious lesion incidence, especially in patients with caries in other teeth.
• The 3M position, such as angulation and degree of eruption, interferes with the incidence of PD, unrelated to PD in other teeth.
• Age is a factor associated with caries and PD that influences OHIP values. OHRQoL worsens with increasing age.
• OHRQoL is negatively influenced by caries and PD.
Caries are infectious and irreversible diseases that cause demineralization of the calcified elements of the tooth, which can affect enamel, dentin, and cementum [19]. The decision to treat carious lesions or to extract 3Ms depends on the experience of each patient and surgeon [6, 19, 20]. Currently, caries is the most common bacterial disease, and when it affects the 3M region, restorative treatment is difficult due to limited access [19]. The presence of caries in 3Ms is associated with caries in other teeth [6, 14], and it is rare that a patient has caries in a 3M without having caries in the other teeth [21, 22, 23].
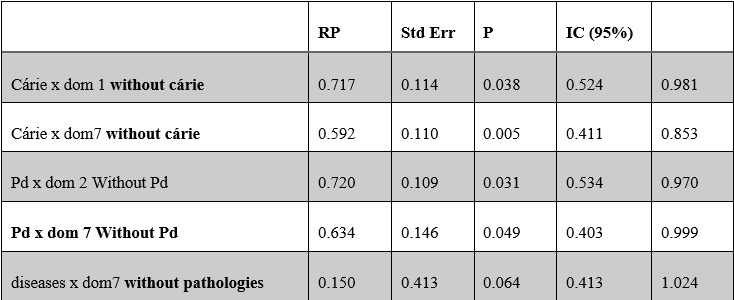
Table 5: Patients distribution according to caries and PD in 3Ms and quality of life.
PD comprises a wide range of inflammatory conditions that affect the supporting structures of the teeth (gingiva, bone, and periodontal ligament). PD develops over time with the accumulation of dental plaque, bacterial dysbiosis, occurrence of periodontal pockets, gum recession, tissue destruction, and alveolar bone loss, and can lead to tooth loss [24]. Some gram-negative anaerobic bacteria are accepted as the etiologic factors of PD [14]. However, the presence of microbial biofilms might not be sufficient for the pathogenesis of PD. Disease occurs when the balance between the microbial biofilm and the host is lost, leading to dysbiosis or immune overreaction of the host to microbial presence. This imbalance is difficult to unravel, as there are variances in both dental plaque and the host genetic and immune system profiles [25].
Renton et al. [26], stated that the main etiological causes of 3M extraction were pericoronitis (64%), caries (31%), and periodontitis (8%). McArdle [28], who obtained similar results, reported as the main causes of 3M removal, pericoronitis (49%), caries (27%), and periodontal disease (5%). In our study, 31.9% of the assessed 3Ms presented with carious lesions and 18.53% presented with PD.
In this clinical observational study with 228 mandibular 3M teeth, carious lesions were added to restored teeth and classified as caries-affected teeth. The teeth were divided into two groups, considering the presence of caries or PD, and naming them with or without pathological occurrence. Another adjustment was to exclude impacted teeth, evaluating only erupted and partially erupted teeth. We analysed only teeth that were present in the oral cavity.
Among the patients in our study, carious lesions and PD were more prevalent in older people. This result is consistent with those of other studies. Blakey et al. [8], Moss et al. [14], Haug et al. [22], Marciani [28], and Jung and Cho [29] reported a higher incidence of carious lesions in 3Ms in patients with a higher age. Blakey et al. [8], Moss et al. [14], and Araujo et al. [30] also observed that the higher prevalence of PD in 3Ms of older patients was also observed by Blakey et al. [8], Moss et al. [14], and Araujo et al. [30]. It is likely that the longer exposure time of the teeth of older patients to etiological factors, such as biofilm, explains the higher incidence of pathological changes in 3Ms. Younger patients have greater potential to cure PD in the 3M region [12], with 3M extraction. (Blakey et al., 2006). This should be considered when indicating the exodontia of 3Ms.
The most prudent age indicated for 3M extraction is before 25 years of age, or before root development is complete [32, 33]. According to Pogrel [35], after root development, there is an increase in the technical difficulty of extraction. Over the years, periodontal ligaments become thicker, ankylosis may appear, the mandible becomes more sclerotic, and hypercementosis becomes more common. In addition, higher age increases the risk of systemic illness and intraoperative or postoperative complications [35].
In this study, the most affected tooth position according to the Winter classification was mesioangular. Carious lesions and PD were more common in this 3M position, the same result reported by Jung and Cho [29]. However, Al Anqudi et al. [36] and Celikoglu et al. [33] described more carious lesions and PD in 3Ms in the horizontal position. Knutsson et al. [38] reported 5 to 12 times more pathologies in distoangular 3Ms. It is known that mesioangular, distoangular, and horizontal 3Ms are positions that increase the accumulation of food and make local brushing difficult. Therefore, in these situations, the occurrence of biofilm accumulation and inflammation can culminate in carious lesions and PD. The greater the angle of the 3M, the greater the food retention and consequently the difficulty in sanitizing. All authors emphasize the idea that angulation eventually leads to a prophylactic indication of extraction to prevent the development of cavities in the mandibular region [10]. Semi-erupted and erupted mesioangular teeth need special attention and should be extracted prophylactically [38].
According to Pell and Gregory´s classification, in our study, the B position had twice as many carious lesions as the A position; position C had 25% more carious lesions than position A. This result agrees with Oderinu et al. [39], who reported a higher risk of carious lesions; the lower the 3Ms were from the cementoenamel limit of the second molar. The more impacted the tooth, more food retention, and, consequently, the greater difficulty in cleaning, increasing the risk of caries and PD. However, Ventä et al. [40] reported that a 3M located deeper in the bone was more likely to be disease-free than a tooth at the occlusal level. This discrepancy may be explained by the different samples that were evaluated. Ventä et al. [40] included the entire population aged 30–98 years, adding up to 5665 3Ms, while our present study assessed 228 3Ms of young adults, with a mean age of 25.25 years.
PD has a high incidence rate in semi-erupted or erupted teeth in this region. Some authors advocate prophylactic extraction of partially erupted mandibular 3Ms due to the possibility of cavities, periodontal disease, or painful symptoms [10]. In corroborating our sample, we also found that erupted and semi-erupted teeth pose a risk for PD.
Due to the bone architecture and poor soft tissue in the 3M region, periodontal problems are more common [31]. The combination of partial eruption in older patients and the anatomical location of 3Ms leads to the accumulation of biofilms colonized by anaerobic pathogens in the region, which are difficult to eradicate [8], increasing the risk of PD [14].
The association of PD in 3M and other molars may exist; however, the study population is extremely limited, as 3M data are often excluded from clinical analysis [8, 12]. The second most common cause of 3M extraction is PD, which is present in 25% of patients older than 25 years [41]. There are many conflicts related to the 3M extraction and periodontal status in the region [42].
The presence of PD or carious lesions in 3Ms suggests that the retention of these teeth in the mouth should be monitored regularly [7, 28, 31, 43]. 3M is the last tooth to develop, erupt, and mineralize in the permanent dentition [43]. Impacted 3Ms are associated with an increased risk of pathology in middle-aged male adults, and the risk of PD is twice as high [45]. Clinically, it is the tooth that is most commonly impacted and responsible for conditions such as periodontitis, pericoronitis, crowding, pain, cysts, etc. [7]. Most 3Ms are extracted due to associated pathologies [14]. Haug et al [22]. and Kaveri and Prakash [46] stated that 3Ms are teeth with no essential function. McCoy [5] stated that 95% of 18-year-old Americans have 3Ms that do not function in chewing. However, 3Ms can have clinical value in some cases; people have benefits in restoring 3Ms when they support fixed or removable prostheses [47]. The longer teeth remain in the mouth, the more vulnerable they are to caries [47].
Patients with asymptomatic 3Ms should be carefully evaluated [12, 28, 22, 43, 32, 48] because caries and PD often do not produce symptoms [21].
The extraction of 3M is considered the most difficult decision faced by oral and maxillofacial surgeons [9, 18, 37]. The indication for prophylactic extraction should be based on risk-benefit. It can be considered a long-term oral health-promoting modality [29], such as caries prevention and PD [33]. Specifically, when talking about some positions, the use of QoL terms and related therapies has increased in the field of oral medicine. OHRQoL is a multidimensional construct that reflects comfort in eating, sleeping, social interaction, self-esteem, and satisfaction with oral health [49].
The OHIP-14 questionnaire is an excellent instrument that measures the impact of oral disease on QoL [50]. Caries and PD can affect the patient’s day-to-day life and OHRQoL, and this concept must be considered when deciding the prophylactic extraction of 3Ms.
Some bias should be considered in our study, such as the subjectivity of the data, based on the perception of the patient. QoL is a subjective measure that is based on a patient's perception, which means different things for each, which can supplement traditional health measures [51, 52].
The presence of carious lesions had an impact on the functional limitation domain and impairment (domains 1 and 7) in our study. The presence of PD had an impact on physical pain and impairment (domains 2 and 7), indicating its influence on the patient’s QoL. Araujo et al. [30], also found an impact of PD on QoL in the functional limitation domain. In another study, domain 2, physical pain, had the greatest impact. All domains, except functional limitations, differed according to the type of PD. PD causes several clinical signs and symptoms, some of which have an impact on QoL [49]. This domain represents physical disability, indicating that pathological changes can make the patient incapable of performing daily tasks.
The prevalence and severity of hip scores were calculated and showed an impact on patients with PD. Patients with PD or caries had higher OHIP scores in domain 7, handicap.
The presence of these teeth can often lead to injury and damage to an individual's oral health, having a significant impact on their QoL, which may include difficulty relaxing, meal interruptions, irritability, and tension, often affecting a person’s ability to work [11]. QoL indices are as important as clinical parameters in the indications for 3M tooth extractions [18].
Acknowledgements
We declare that this study was funded by the researchers. The authors declare no conflict of interest. Individual patient data will remain confidential. The results of this study can be presented at international conferences and published. All data were saved at the University of São Paulo, São Paulo, Brazil. This protocol is registered at clinicaltrials.gov NCT 04024644. We would like to thank Editage (www.editage.com) for English language editing.
Funding: no funding
Authors’ Contributions
Conceptualization: Renata Matalon Negreiros, Edgard Michel-Crosato.
Formal analysis: Edgard Michel-Crosato, Maria Gabriela Haye Biazevic.
Investigation: Renata Matalon Negreiros, Edgard Michel-Crosato.
Methodology: Renata Matalon Negreiros, Maria Gabriela Haye Biazevic.
Project administration: Renata Matalon Negreiros, Edgard Michel-Crosato.
Resources: Renata Matalon Negreiros, Edgard Michel-Crosato.
Supervision: Edgard Michel-Crosato, Waldyr Antonio Jorge.
Validation: Anna Carolina Ratto Tempestini Horliana, Maria Gabriela Haye Biazevic.
Writing – original draft: Tânia Oppido Schalch, Renata Matalon Negreiros.
Writing - review & editing: Renata Matalon Negreiros. Monira Samaan Kallás, Anna Carolina RattoTempestini, Tânia Oppido Schalch, Waldyr Antonio Jorge.
Conflict of Interest: no conflict of interest.
References
- Silvestri AR, Singh I. (2003) The unresolved problem of the third molar: would people be better off without it? J Am Dent Assoc. 134(4): 450-455. [PubMed.]
- Kaveri GS, Prakash S. (2012) Third molars: a threat to periodontal health?? J Maxillofac Oral Surg. 11(2): 220-223. [PubMed.]
- Divaris K, Fisher EL, Shugars DA, White RP Jr. (2012) Risk factors for third molar occlusal caries: a longitudinal clinical investigation. J Oral Maxillofac Surg. 70(8): 1771-1780. [PubMed.]
- Fejerskov O. (2004) Changing paradigms in concepts on dental caries: consequences for oral health care. Caries Res. 38(3): 182-91. [PubMed.]
- McCoy JM. (2012) Complications of retention: pathology associated with retained third molars. Atlas Oral Maxillofac Surg Clin North Am. 20(2): 177-1795. [PubMed.]
- Ahmad N, Gelesko S, Shugars D, White RP Jr, Blakey G, et al. (2008) Caries experience and periodontal pathology in erupting third molars. J Oral Maxillofac Surg. 66(5): 948-953. [PubMed.]
- Chang SW, Shin SY, Kum KY, Hong. (2009) Correlation study between distal caries in the mandibular second molar and the eruption status of the mandibular third molar in the Korean population. J. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 108(6): 838-843. [PubMed.]
- Blakey GH, Gelesko S, Marciani RD, Haug RH, Offenbacher S, et al. (2010) Third molars and periodontal pathology in American adolescents and young adults: a prevalence study. J Oral Maxillofac Surg. 68(2): 325-329. [PubMed.]
- Polat HB, Ozan F, Kara I, Ozdemir H, Ay S. (2008) Prevalence of commonly found pathoses associated with mandibular impacted third molars based on panoramic radiographs in Turkish population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 105(6): e41-47. [PubMed.]
- Falci SGM, de Castro CR, Santos RC, de Souza Lima LD, Ramos-Jorge ML, et al. (2012) Association between the presence of a partially erupted mandibular third molar and the existence of caries in the distal of the second molars. Int J Oral Maxillofac Surg. 41(10): 1270-1274. [PubMed.]
- Slade GD, Foy SP, Shugars DA, Phillips C, White RP. (2004) The impact of third molar symptoms, pain, and swelling on oral health-related quality of life. J Oral MaxillofacSurg. 62(9): 1118-1124.' [PubMed.]
- Fisher EL, Garaas R, Blakley GH, Offenbacher S, Shugars DA, et al. (2012) Changes over the time in the prevalence of caries experience or periodontal pathology on third molars in young adults. J Oral Maxillofac Surg. 70(5): 1016-1022. [PubMed.]
- Abesi F, Mirshekar A, Moudi E, Seyedmajidi M, Haghanifar S, et al. (2012) Diagnostic Accuracy of Digital and Conventional Radiography in the Detection of Non-Cavitated Approximal Dental Caries. Iran J Radiol. 9(1): 17-21. [PubMed.]
- Moss KL, Beck JD, Mauriello SM, Offenbacher S, White RP J. (2007) Third molar periodontal pathology and caries in senior adults. J Oral Maxillofac Surg. 65(1): 103-108. [PubMed.]
- Pell GJ, Gregory GT. (1942) Report on a ten-year study of a tooth division technique for removal of impacted teeth. Ame J Orthod Oral Surg. 28: 660-666. [Ref.]
- Almendros-Marqués N, Berini-Aytés L, Gay-Escoda C. (2008) Evaluation of intraexaminer and interexaminer agreement on classifying lower third molars according to the systems of Pell and Gregory and of Winter. J Oral Maxillofac Surg. 66(5): 893-899. [PubMed.]
- Oliveira BH, Nadanovsky P. (2005) Psycometric properties of the Brazilian version of the oral health impact profile-short form. Com Dent Oral Epidemiol. 33(4): 307-314. [PubMed.]
- Negreiros RM, Biazevic MGH, Jorge WA, Michel-Crosato E. (2012) Relationship between oral health-related quality of life and the position of the lower third molar: postoperative follow-up. J Oral Maxillofac Surg. 70(4): 779-786. [PubMed.]
- Shugars DA, Elter JR, Jacks MT, White RP, Phillips C, et al. (2005) Incidence of occlusal dental caries in asymptomatic third molars. J Oral Maxillofac Surg. 63(3): 341-346. [PubMed.]
- Fisher EL, Moss KL, Offenbacher S, Beck JD, White RP . (2010) Third molar caries experience in middle-aged and older Americans: a prevalence study. J Oral Maxillofac Surg. 68(3): 634-640. [PubMed.]
- White RP, Fisher EL, Phillips C, Tucker M, Moss KL, et al. (2011) Visible third molars as risk indicator for increased periodontal probing depth. J Oral Maxillofac Surg. 69(1): 92-103. [PubMed.]
- Haug RH, Abdul-Majid J, Blakley GH, White RP. (2009) Evidence based decision making: the third molar. Dent Clin North Am. 53(1): 77-96. [Ref.]
- White RP, Proffit WR. (2011) Evaluation and management of asymptomatic third molars: Lack of symptoms does not equate to lack of pathology. Am JOrthod Dentofacial Orthop. 140(1): 10-16. [Ref.]
- Michaud DS, Fu Z, Shi J, Chung M. (2017) Periodontal Disease, Tooth Loss, and Cancer Risk. Epidemiol Rev. 39(1): 49-58. [PubMed.]
- Kinane DF, Stathopoulou PG, Papapanou PN. (2017) Periodontal diseases. Nat Rev Dis Primers. 22(3):17038 [PubMed.]
- Renton T, Al-Haboubi M, Pau A, Shepherd J, Gallagher JE. (2012) What has been the United Kingdom's experience with retention of third molars? J Oral Maxillofac Surg. 70(suppl 1):548-557. [PubMed.]
- McArdle LW, Andiappan M, Khan I, Jones J, McDonald F. (2018) Diseases associated with mandibular third molar teeth. Br Dent J. 224(6): 434-440. [Ref.]
- Marciani RD. (2012) Is there pathology associated with asymptomatic third molars J Oral Maxillofac Surg. 70(1):15-19. [PubMed.]
- Jung YH, Cho BH. (2013) Prevalence of Missing and impacted third molar in adults aged 25 years and above. Imaging Sci Dent. 43(4): 219-225. [PubMed.]
- Araujo AC, Gusmao ES, Batista JE, Cimoes R. (2010) Impact of periodontal disease on quality of Life. Quintessence Int. 41(6): 111-118. [PubMed.]
- Blakey GH, Jacks MT, Offenbacker S, Nance PE, Phillips C, et al. (2006) Progression of periodontal disease in the second/third molar region in subjects with asymptomatic third molars. J Oral Maxillofac Surg. 64(2): 189-193. [PubMed.]
- Rafetto LK, Synan W. (2012) Surgical Management of third molars. Atlas Oral Maxillofac Surg Clin North Am. 20(2): 197-223. [PubMed.]
- Celikoglu M, Miloglu O, Kazanci F. (2010) Frequency of agenesis, impaction, angulation, and related pathologic changes of third molar teeth in orthodontic patients. J Oral Maxillofac Surg. 68(5): 990-995. [PubMed.]
- Pogrel MA. (2012) What is the effect of timing of removal on the incidence and severity of complications J Oral Maxillofac Surg. 70: 37- 40. [PubMed.]
- Shoshani-Dror D, Shilo D, Ginini JG, Emodi O, Rachmiel A. (2018) Controversy regarding the need for prophylactic removal of impacted third molars: An overview. Quintessence Int. 49(8): 653-662. [PubMed.]
- Al-Anqudi SM, Al-Sudairy S, Al-Hosni A, Al-Maniri A. (2014) Prevalence and Pattern of Third Molar Impaction: A retrospective study of radiographs in Oman. Sultan Qaboos Univ Med J. 14(3): e388-392. [PubMed.]
- Knutsson K, Brehmer B, Lyesell L, Rohlin Ml. (1996) Pathoses associated with mandibular third molars subjected to removal. Oral Surg oral med Oral Pathol Oral Radiol Endod. 82(1):10-17. [PubMed.]
- Allen RT, Witherow H, Collyer J, Roper-Hall R, Nazir MA, et al. (2009) The mesioangular third molar--to extract or not to extract? Analysis of 776 consecutive third molars. Br Dent J. 206(11): E23. [Ref.]
- Oderinu OH, Adeyemo WL, Adeyemi MO, Nwathor O, Adeyemi MF. (2012) Distal cervical caries in second molars associated with impacted mandibular third molars: a case-control study. Oral Surg Oral Med Oral Pathol Oral Radiol. pii: S2212-4403(12)00395-00401. [PubMed.]
- Ventä I, Vehkalahti MM, Suominen AL. (2019) What kind of third molars are disease-free in a population aged 30 to 93 years? Clin Oral Investig. 23(3): 1015-1022. [PubMed.]
- Bradshaw S, Faulk J, Blakey GH, Phillips C, Phero JA, et al. (2012) Quality of Life Outcomes After Third Molar Removal in Subjects with Minor Symptoms of Pericoronitis. J Oral Maxillofac Surg. 70(11): 2494-2500. [PubMed.]
- Dicus-Bookes C, Patrick M, Blakey GH, Faulk-Eggleston J, Offenbacher S, et al. (2013) Removal of symptomatic third molar may improve periodontal status of remaining dentition. J Oral Maxillofac Surg. 71(10): 1639-1646. [PubMed.]
- Garaas RN, Moss KL, Fisher EL, Wilson G, Offenbacher S, et al. (2011) Prevalence of visible third molars with caries experience or periodontal pathology in middle-aged and older Americans. Jr.J Oral Maxillofac Surg. 69(2):463-470. [PubMed.]
- Zhang QB, Zhang ZQ. (2012) Early extraction a silver Bullet to avoid nerve injury in lower third molar removal. Int J Oral Maxillofac Surg. 41(10): 1280-1283. [PubMed.]
- Nunn ME, Fish MD, Garcia RI, Kaye EK, Figueroa R, et al. (2014) Response to letter to editor Retained Asymptomatic third molar and risk for second molarpathology. J Dent Res. 93(3): 320-321. [PubMed.]
- Kaveri GS, Prakash S. (2012) Third molars: a threat to periodontal health? J Maxillofac Oral Surg. 11(2): 220-223. [Ref.]
- Mikić IM, Zore IF, Crcić VF, Matijević J, Plancak D, et al. (2013) Prevalence of third molars and pathological changes related to them in dental medicine. Coll Antropol. 37(3): 877-884. [PubMed.]
- Baelum V, Hintze H, Wenzel A, Danielsem B. (2012) Implications of caries diagnostic stategies for clinical management decisions. Community Dent Oral Epidemiol. 40(3): 257-266. [PubMed.]
- Al Habashneh R, Khader YS, Salameh S. (2012) Use of Arabic versison of oral Health Im pacat profile-14 to evaluate the impact of periodontal disease on oral health-related quality of life among Jordanian adults. J Oral Science. 54(11): 113-120. [PubMed.]
- Schalch TO, Palmieri M, Longo PL, Braz-Silva PH, Tortamano IP, et al. (2019) Evaluation of photodynamic therapy in pericoronitis: Protocol of randomized, controlled, double-blind study.Medicine (Baltimore). 98(17): e15312. [PubMed.]
- Locker D, Allen F. (2007) Does self-weighting of items enhance the performance of an oral health-related quality of life questionnaire? Com Dent Oral Epidemiol. 35(1): 35-43. [PubMed.]
- Allen RT, Witherow H, Collyer J, Roper-Hall R, Nazir MA, et al. (2009) The mesioangular third molar--to extract or not to extract? Analysis of 776 consecutive third molars. Br Dent J. 206(11): E23; discussion 586-587. [PubMed.]