>Corresponding Author : Ghada El Hilaly Mohamed Eid
>Article Type : Research Article
>Volume : 1 | Issue : 3
>Received Date : 7 December, 2021
>Accepted Date : 22 December, 2021
>Published Date : 25 December, 2021
>DOI : https://doi.org/10.54289/JDOE2100111
>Citation : Abdelnaby MS, Eid GEM, EI Nabarawi MA. (2021) The Effect of Premedication with Curcumin on Post-Operative Pain in Single Visit Endodontic Treatment of Acute Pulpitis in Mandibular Molars: A Randomized Controlled Trial. J Dent Oral Epidemiol 1(3): doi https://doi.org/10.54289/JDOE2100111
>Copyright : © 2021 Abdelnaby MS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Research Article | Open Access
1Faculty of Dentistry, Department of Endodontics, Cairo University, Egypt 2Faculty of Pharmacy, Department of Pharmaceutics and Industrial Pharmacy, Cairo University, Egypt
*Corresponding author: Ghada El Hilaly Mohamed Eid, Faculty of Dentistry, Department of Endodontics, Cairo University, Egypt
Abstract
Objective: The purpose of this randomized double-blind clinical trial was to compare the effect of a single pretreatment dose of Curcumin and placebo on post-operative pain for patients diagnosed with symptomatic irreversible pulpitis in mandibular molars treated in single visit.
Methods: Forty-four patients with severe to moderate pain randomly received either Curcumin (400mg +20 mg pepper) or placebo (420 mg Starch) one hour before starting root canal treatment (n = 22 per group). Participants rated their pain using visual analogue pain scale (VAS): preoperatively and at 5 time points: immediately post-operative, 8, 12, 24 and 48 hours postoperative. Patients also stated emergency analgesic intake. The need for supplemental anesthesia during treatment was recorded. Mann-Whitney U-test compared the two groups at each time point, while Repeated-Measure ANOVA and Wilcoxon Signed Rank test compared time points within each group. A p-value <0.05 was considered statistically significant.
Results: Baseline characteristics of both groups showed non-significant differences (P > 05). Curcumin group at 8, 12 and 24 hours revealed statistically significantly less VAS values (44.2, 26.7, 19.1) than the placebo (58.5, 43.3, 30.3), respectively, (P > 05). All patients in Curcumin group did not need emergency analgesics. Curcumin group revealed statistically significantly lower percentages for the need of supplemental anesthesia (27.3%) compared to placebo (68.2%), (P < 05).
Conclusion: Single preoperative oral dose of Curcumin proved to be an effective premedication that reduced post-operative pain as well as the need of supplemental anesthesia for patients diagnosed with symptomatic irreversible pulpitis of mandibular molars.
Keywords: Symptomatic irreversible pulpitis, mandibular molars, post-operative pain, Curcumin, randomized controlled trial.
Abbreviations: VAS: visual analogue pain scale, NSAIDs: non-steroidal anti-inflammatory drugs, IANB: Inferior Alveolar Nerve Block
Introduction
Post endodontic pain is one of the primary problems in single visit treatment in cases of irreversible pulpitis of mandibular molars. A systematic review reported post endodontic pain ranging from 25% to 40% in single visit treatment of diseased vital pulp cases [1]. The severity of pain is highest at 6 to 8 hours after endodontic treatment [2]. Post-operative pain is attributed to periapical inflammation resulting from pulp extirpation; whereby pain fibers get directly stimulated or sensitized by the released inflammatory mediators. In addition, the vascular dilation, increases permeability and interstitial tissue response [3, 4]. Common effective pharmacological premeditations targeting inhibition of prostaglandins are corticosteroids [5-7] and non-steroidal anti-inflammatory drugs (NSAIDs) [8-11]. NSAIDs suppress the inflammation and pain by inhibition of cyclooxygenase enzymes (COX-1 and COX-2) which are responsible for production of the inflammatory mediator prostaglandin. However, there exist some side effects such as inhibition of the protective role of COX-1 to stomach lining increasing the possibility of gastric ulcer occurrence [12].
Thus, the search for natural herbs having anti-inflammatory and analgesic potentials is encouraged hoping to provide the required pain control without the side effects of NSAIDs [13]. Curcumin (diferuloylmethane), the main yellow bioactive component of turmeric herb has been shown to have a wide spectrum of useful biological actions such as powerful antioxidant [13], anti-inflammatory [14], anti-bacterial, anti-viral and fungal effect [15], anti-platelets aggregation [16], as well as being effective in treatment of gastric ulcer [17]. In medical clinical trials, Curcumin analgesic effect is recommended for pain relief after laparoscopic cholecystectomy [18], in patients with osteoarthritis [19] and rheumatoid arthritis [20]. The use of Curcumin as intracanal medication in an vitro study; reveals potent antibacterial activity against pathogenic bacteria including Enterococcus Feacales [21], while its use in an in-vivo, shows high analgesic and anti-inflammatory effect [22].
Thus, despite the useful use of Curcumin in the medical field for pain control, however, there is little available evidence supporting its use in controlling post endodontic pain. Thus, the aim of this study was to determine the effect of preoperative oral administration of Curcumin on the post-operative pain in single visit endodontic treatment of symptomatic irreversible pulpitis in mandibular molars teeth. The null hypothesis was that there is no effect of preoperative administration of Curcumin on post-operative pain as compared to placebo.
Material and Methods
Study design and setting: This 1:1 allocation ratio parallel randomized controlled trial design was approved by evidence-base and ethical committee, Faculty of Dentistry. Study reporting followed the Consolidated Standards of Reporting Trials guidelines. The study protocol was registered on www. clinicaltrials.gov (Clinical Trials.govidentifier: NCT04012424). The trial took place in the outpatient clinic of the Department of Endodontics. Participants signed printed informed consent; after the investigator explained the aim of the study, treatment procedures and possible side effects.
Sample Size calculation: Considering data from a previous study [23], a type I error at 5% and statistical power of 80%, the minimum sample required to detect differences between 2 groups was calculated to be 19 subjects/group. The sample size was increased to 22 participants per group considering a 15% dropout rate.
Participants' eligibility criteria: Inclusion Criteria were males and females, with age range 20- 55y, suffering from symptomatic irreversible pulpitis in mature mandibular first or second molar teeth. Exclusion criteria were cases with non-vital pulp, acute apical periodontitis or patients with known allergy to Curcumin or medications administered or those who took analgesic medication within 12-hour time. Non- restorable or periodontally affected teeth or teeth in malocclusion or with anatomic abnormalities as well as medically compromised patients were excluded.
Diagnosis: Diagnosis was based on patient’s chief complaint, and clinical and radiographic examination. Preoperatively patients experienced moderate to severe pain (45-100 mm readings on the visual analogue scale VAS) [24,25]. Pain was spontaneous or stimulated by thermal changes. A lingering pain which continued after the removal of the stimulus was also indicative of irreversible pulpitis. The teeth gave positive early response to ethyl chloride cold test as well as to electric pulp testing (Denjoy DY310 Dental Pulp Tester, Denjoy Dental Co, Hunan, China). There was no pain on palpation or percussion. Periapical radiographs revealed absence of periapical involvement.
Randomization, allocation concealment and blinding: The random allocation sequence was generated via (http://www.random.org/); with 22 participants/ group. Allocation concealment until intervention was done by placing the loaded capsules in sequentially numbered sealed opaque envelop according to the generated sequence. Both Curcumin and placebo capsules had the same color and shape. Thus after assignment to the groups both operator and patients were blinded to the capsule content, the data assessor was also blinded. The code details were not revealed until the end of the study.
Intervention: Eligible participant was given the envelope and was asked to take the contained capsule; either Curcumin capsules (400mg Curcumin" Curcumin, Shanghai, China" + 20 mg pepper) or a placebo capsule (starch 420 mg). One hour after medication, the tooth was anesthetized by Inferior Alveolar Nerve Block (IANB) using 1.8 ml of 4% Articaine HCl with 1:100,000 epinephrine (Artinibsa (4% carpule. inibsa, spain). Post-injection lip numbness was a subjective sign of IANB success. After isolation with rubber dam, access cavity preparation was performed and canal patency was confirmed with K-file size #10 (Mani, Mani Inc. Utsunomiya, Tochigi, Japan). Working length was determined using apex locator ( iPex II, NSK, Japan), and confirmed radiographically to be 1 mm short of the radiographic apex. Root canals were prepared using M-Pro nickel titanium rotary instruments (M- Pro smart kit, Hunan, China) at a speed 450 rpm and torque 1.5Ncm (Endo motor, NSK, Japan). Rotary files were introduced inside the canal lubricated with EDTA Cream for easier negotiation (dMD-Chelcream, META BIOMED CO, Korea). Preparation was done in crown down sequence as follows: orifice opener, # 20 4%, # 25 6%, and finally # 35 4%. The canals were irrigated using 2.5% NaOCl, at a rate 1ml/30 second, by side vent 27-gauge needles reaching a maximum depth of 1mm short of working length. Supplemental anesthesia was given in case the patient experienced pain during access cavity or extirpation according to the following sequence: buccal infiltration (1/2 Articane cartridge), intraligmentary and finally intra pulpal anesthesia if needed. Canals were dried using proper sized paper points and obturated using lateral gutta-percha compaction technique and ADSEAL sealer (ADSEAL, META BIOMDED CO., LTD, Korea). Access cavity was temporized using Coltosol; Coltene Brasil, Rio de Janeiro, RJ, Brazil), and reduced from occlusion. Post-obturation periapical radiograph (Kodak, USA, speed D, size 2) was taken.
Assessment of Post-operative pain: Patients were given visual analog pain scale VAS which consists of a 10-cm line anchored by 2 extremes, ‘‘no pain’’ and ‘‘pain as bad as it could be.’’ Patients were asked to put a mark on the line to describe their pain level on the VAS sheets at five intervals: immediately after treatment and at 8, 12, 24, 48 hours post-operatively. Patients delivered their sheets after 48 hours and were referred for permanent restoration. Readings were transformed into categories; no pain (range of 0-4mm), mild pain (range of 5-44mm), moderate pain (range of 45-74mm) and severe pain (range of 75-100mm) [25]. In case of severe pain, a rescue analgesic (ibuprofen 600mg tab/8hr) was prescribed and recorded. Primary outcome was postoperative pain. Secondary outcomes were the need for supplemental anesthesia and rescue medication.
Statistical analysis: Data were tested for normality with Kolmogorov–Smirnov test. Mann-Whitney U-test compared the two groups at each time point, while Repeated-Measure ANOVA and Wilcoxon Signed Rank test compared time points within each group A p-value <0.05 was considered statistically significant.
Results
Sixty participants were accessed for eligibility. Sixteen patients were excluded for not meeting inclusion criteria or refusal to participate in the trial. Forty-four patients were enrolled, and randomly allocated in the two groups. All participants were analyzed. None of thepatients reported any side effects for up to 48 hours after the procedures.
Baseline data: There was no significant difference between the groups regarding the following baseline characteristics: age, gender and pre-operative pain VAS scores and incidence of pain categories (P < 05), Table (1).
Table 1: Comparison of demographic characteristics: age, gender and pre operative pain of studied groups.
| Curcumin Group A (n = 22) | Placebo Group B (n = 22) | P-value | |||
|---|---|---|---|---|---|
| Age (years) | Mean ± SD (Range) | 31.6 ± 9.8 (18 – 50) | 38.7 ± 9.6 (20 – 52) | 0.949 | |
| Gender | Male n (%) | 10 (45.5%) | 11 (50%) | 0.763 | |
| Female n (%) | 12 (54.5%) | 11 (50%) | |||
| Pre-operative pain | VAS score | mean± SD | 83.9 ± 7.3 | 83.8 ± 7.5 | 0.814 |
| (range) | (65 – 94) | (66 – 93) | |||
| Pain incidence | Moderate: n (%) | 3 (13.6%) | 5 (%22.7) | 0.698 | |
| Severe: n (%) | 19 (86.4%) | 17(77.3%) | |||
Comparison of the pain scores between studied groups at each time point, Table (2): Curcumin group had lower VAS scores values than placebo group at each time point. At three time points namely, 8 hours, 12 hours, and 24 hours statistically significant reduction occurred in Curcumin group compared with placebo, (p> 05).
Comparison of pain scores at different time points within each group, Table (2): Within each group a significant decrease in VAS scores was observed between the baseline and all time intervals, (P < 0.001). Pairwise analysis showed in placebo group there was significant difference between each successive time points, (p> 05). While in Curcumin group there was significant difference between successive time points, except between immediate post-operative and 8 hours post-operative, P = 0.054 as well as between 12- and 24-hours post-operative, P = 0.203. Both groups showed the same pattern of decrease of pain up to immediate post-operative followed by a sharp increase at the 8-hour time point followed by a decreasing tend up to 48- hour time point.
Table 2: Stastitical analysis of the VAS pain scores between studied groups at each time point (horizontal) and comparison of all time points within each group (vertical)
| Curcumin Group A (n = 22) | Placebo Group B (n = 22) | ||||
|---|---|---|---|---|---|
| Mean ± SD | 95% CI | Mean ± SD | 95% CI | P-value | |
| Preoperative | 83.9 ± 7.3 | 80.6, 87.1 | 83.8 ± 7.5 | 80.5, 87.2 | 0.814 |
| Immediately post operative | 26.6 ± 17.7 | 18.8, 34.5 | 27.5 ± 17.9 | 19.5, 35.4 | 0.510 |
| 8-hours | 44.2 ± 15.8 | 37.2, 51.2 | 58.5 ± 13.5 | 52.5, 64.4 | 0.001 |
| 12-hours | 26.7 ± 13.4 | 20.8, 32.7 | 43.3 ± 17.5 | 35.5, 51.0 | 0.001 |
| 24-hours | 19.1 ± 8.4 | 15.4, 22.9 | 30.3 ± 14.3 | 23.9, 36.6 | 0.002 |
| 48-hours | 9.0 ± 8.5 | 5.3, 12.8 | 15.2 ± 10.1 | 10.7, 19.7 | 0.054 |
| P-value | 0.001* | 0.001* | |||
Comparison of incidence of pain categories between the two groups at each time point; there was significant difference between percentages of different pain categories at 8 hours post-operative (P < 0.001) and at 12 hours post-operative (P = 0.002), Figure (1).
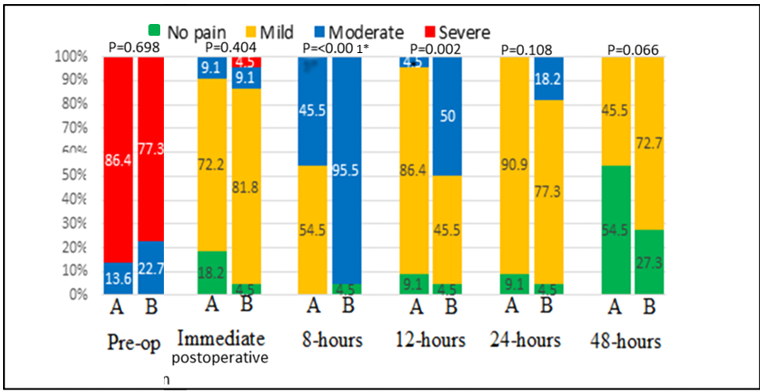
Figure 1: Stacked bar chart showing comparison of incidence of pain categories between the two groups at each time point; Group A: Curcumin, and Group B: Placebo. Statistically significant (p-value < 0.05)
Comparison between groups for the need of supplemental anesthesia: Significantly lower percentages of patients needed supplemental anesthesia in Curcumin group (n = 6, 27.3%) compared to placebo (n = 15, 68.2%); (p value = 0.004).
Comparison between groups for the need of emergency analgesic medication: All patients in Curcumin group did not need analgesics, while two patients in placebo group took analgesics (p value = 0.488).
Discussion
Ultimate control of pain during and after root canal treatment still presents a clinical demand. Patients with severe preoperative pain present challenge for intraoperative pain and postoperative pain control especially in cases of mandibular molars [1, 26]. A decreased susceptibility to pulpal anesthesia of mandibular molars compared to maxillary molars might be due to various factors such as the different bony landmark, anatomical variation, needle deflection, accessory innervations [27].
Premedication proved to be effective in both reduction of post-operative pain [28] and pain during root canal treatment [26]. No randomized controlled trial studied the effect of the natural herb Curcumin on post endodontic pain, though it has proven its efficacy in medical clinical trials [18-20]. It has a reported role in reducing postsurgical pain [18]. The efficacy and safety of Curcumin are reported in a randomized controlled trial that studied Curcumin versus diclofenac in patients with active rheumatoid arthritis [20], as well as another trial that studied curcuma domestica extracts versus ibuprofen in patients with knee osteoarthritis [19]. Both studies concluded that most of adverse effects occurred more frequently with sodium diclofenac or ibuprofen. The analgesic and inflammatory effects of Curcumin were explained by; first Curcumin capacity to inhibit prostaglandin2 production via the inhibition of COX-2 gene expression and inhibition of arachidonic acid metabolism via lipoxygenase and scavenging of free radicals generated in this pathway. Thus cyclooxygenase path would be blocked and pain sensation would be prevented before it even begins, second to stimulate cortisol production by adrenal gland, third to deplete nerve ending of the neurotransmitter substance [30] , fourth Curcumin provides down regulation of inflammatory cytokines namely: interleukins-1, 2, 5, 6, 8, 12 and TNF-a [14, 18], fifth it down regulates enzymes, such as protein kinase C that mediate inflammation [14]. Since the liver is the major organ responsible for metabolism of Curcumin [29] it is assumed that Curcumin can be a suitable option in patients with kidney disease. Moreover, being effective in treatment of gastric ulcer [17] it can be a good analgesic choice for those patients.
The present study used 400mg Curcumin in accordance with Drobnic et al. [31] who reported that 400mg Curcumin provided better analgesic effect and gastric tolerability compared with 500mg acetaminophen. Furthermore, 20 mg pepper was added for increasing Curcumin bioavailability [32]. Nanocurcumin can enhance its bioavailability [33]; emphasizing its possible use in further studies instead of incorporating pepper.
The control group was chosen to be placebo to avoid bias and assures that if improvement occurs only in the intervention group, this surely would be from the investigated treatment. A standard rescue medication (ibuprofen600 tab/8hr) and emergency appointment were offered for patients in case of severe pain.
During shaping and cleaning; irrigation was done using 2.6% freshly prepared sodium hypochlorite [34]. Several precautions aided to decrease the possibility of extrusion of irrigants to periapical area with its possible confounding effect on postoperative pain: first, a side-vent needle 27-gauge was inserted to maximum depth of 1mm shorter of the working length. Second, irrigation was delivered at a slow rate 1ml/30 second.
Curcumin was tolerated by the patient. No patient reported any gastric side effects from this single preoperative dose of Curcumin pepper capsule. This may be attributed to the fact that Curcumin blocks COX-2 only while NSAIDs block both COX-1 and COX-2, which can cause gastrointestinal effects [12].
Base line characteristics; age, gender, and the preoperative pain, were statistically non-significant in both groups This eliminates their possible confounding effects and assures homogeneity between the two groups [35].
The present study revealed that the null hypothesis was rejected at 8 and 12 hours, in terms of pain intensity and percentage of pain categories. At these time points, there was statistically significant decrease of both VAS scores and incidence of pain categories in Curcumin group compared to placebo.
The pattern of intragroup VAS scores along different time points was similar in both groups. The decrease in immediate-postoperative-VAS scores in both groups to 26.6 in Curcumin group and to 27.5 in placebo group is expected because of the effect of local anesthesia where pulpal anesthesia usually lasts for 60 to 90 minutes [36]. The spike in VAS scores at 8 hours post-operative in both groups was similarly observed when using pharmacological analgesics or placebo [8, 9, 11]. It was explained that post treatment severity levels may be caused by ongoing inflammatory processes; apical instrumentation; injection of local anesthetic; pressure from a rubber dam clamp; or discomfort because of prolonged mouth opening [2]. The good news is that in Curcumin group the mean VAS score at 8 hours was statistically significantly lower (44.2) than in placebo (58.5). Additionally, the incidence of pain categories was of clinical relevance where in Curcumin group nearly half patients had mild pain (54.5%) and the remaining had moderate pain (45.5%), while in placebo group almost all patients (95.5%) had moderate pain.
At 12 hours postoperative further reduction of pain occurred in both groups, a similar trend was observed in other studies with other pharmacological drugs [37, 38] or placebo [8, 37, 38]. Further clinical significance exists at this time point where the mean VAS pain score reduction was statistically significantly lower in Curcumin group (26.7) compared to placebo (43.4). Moreover, in Curcumin group no pain or mild pain occurred in nearly all patients (95.5%) while in placebo group only half patients (50%) had no pain or mild pain and the other 50% had moderate pain. This reduction can be attributed to pharmacodynamics of Curcumin where it is reported that peak analgesia and anti-inflammatory effect is experienced at 1 to 2 hours and has long half-life lasting for 12 hours [39]. At 24 hours postoperative further reduction in pain values occurred in both groups, which was more in Curcumin group (19.1) versus placebo (30.3). Both values were in the mild range tolerated by the patients. Similar trend of reduction of postoperative pain at this point was observed in other studies that used pharmacological drugs [7-9, 11, 40] or placebo [8, 37, 38]. At 48 hours post-operative pain scores decreased to 9 in Curcumin and 15.2 in placebo. All patients in both groups had mild or no pain. Moderate and Severe pain were absent in both groups. Similar trend of pain reduction trend was revealed in other studies [8, 40]. This pain reduction follows the decline of inflammatory reaction in the tissues by time.
Regarding the need of the supplemental anesthesia, results showed that lower proportion of patients (27.8%) needed supplemental anesthesia compared to placebo (68.2%). It was observed that all patients who took supplemental anesthesia in both groups suffered from preoperative severe pain. However, well organized observational studies might be useful to decide risk factors. Worthy to state that in Curcumin group, the percentage of patients who did not need supplemental anesthesia was almost similar to a study that used diclofenac potassium (75%) [41]. Also in the placebo group of the current study, the percentage for those who did not need supplemental anesthesia was similarly reported previously [42].
Ibuprofen was prescribed as rescue medication for post-operative pain relief after root canal treatment [43]; where only two patients (9%) in placebo group took the rescue medication. The low percentage of analgesic intake in the present study might be related to preoperative confinement of inflammation to pulpal tissue and precautions taken during technical steps of treatment. Furthermore, one cannot underestimate the effect of psychological reassurance which eases patients' anxiety.
It appeared that preoperative Curcumin administration aided intraoperative pain control, reduced post-operative pain intensity to a tolerable level and limited its duration. Thus, by using Curcumin premedication, VAS scores along postoperative time points mostly lied in a tolerable mild range where no patient took rescue medication. Interestingly, lower proportion of patients (27.8%) needed supplemental anesthesia compared to placebo (68.2%).
Conclusion
Within the limitations of this study, it could be concluded that premedication with single oral dose Curcumin provides an effective, safe, inexpensive reduction in intraoperative and post endodontic pain in single visit endodontic treatment of mandibular molars with symptomatic irreversible pulpitis. However, further randomized controlled trials are recommended to examine the effect of Curcumin premedication on the success of inferior alveolar nerve block during different stages of endodontic treatment and in different pulp and periapical diseases. Moreover, further randomized clinical trials are recommended to establish the direct comparison of Curcumin versus other NSAIDs.
References
- De Geus JL, et al. (2018) Effects of ibuprofen compared to other premedication drugs on the risk and intensity of postendodontic pain: a systematic review. Eur Endod J. 3(3): 123-133. [PubMed.]
- Pak JG, White SN. (2011) Pain prevalence and severity before, during, and after root canal treatment: a systematic review. J Endod. 37(4): 429-438. [PubMed.]
- Clem WH. (1970) Posttreatment endodontic pain. J Am Dent Assoc. 81(5): 1166-1170. [PubMed.]
- Torabinejad MR, Walton R. (2008) Pulp and periapical pathosis. Endodontics: Principles and Practice. 4: 49. [Ref.]
- Suresh N, et al. (2021) Effect of preoperative oral administration of steroids in comparison to an anti‐inflammatory drug on postoperative pain following single‐visit root canal treatment–a double‐blind, randomized clinical trial. Int Endod J. 54(2): 198-209. [PubMed.]
- Elkhadem A, et al. (2018) The effect of preoperative oral administration of prednisolone on postoperative pain in patients with symptomatic irreversible pulpitis: a single‐centre randomized controlled trial. Int Endod J. 51: e189-e196. [PubMed.]
- Pochapski MT, et al. (2009) Effect of pretreatment dexamethasone on postendodontic pain. Oral Surg Oral Med Oral Pathol Oral Radiol and Endod. 108(5): 790-795. [PubMed.]
- Mokhtari F, et al. (2016) Effect of premedication with indomethacin and ibuprofen on postoperative endodontic pain: a clinical trial. Iran Endod J. 11(1): 57-62. [PubMed.]
- Menke ER, et al. (2000) The effectiveness of prophylactic etodolac on postendodontic pain. J endod. 26(12): 712-715. [PubMed.]
- Metri M, Hegde S, Bhandi S. (2016) Effect of pretreatment diclofenac sodium on postendodontic pain: A randomised controlled trial. J Conserv Dent. 19(1): 7-10. [PubMed.]
- Ramazani M, et al. (2013) The prophylactic effects of zintoma and ibuprofen on post-endodontic pain of molars with irreversible pulpitis: a randomized clinical trial. Iran Endod J. 8(3): 129-134. [PubMed.]
- Bhala N, et al. (2013) Vascular and upper gastrointestinal effects of non-steroidal anti-inflammatory drugs: meta-analyses of individual participant data from randomised trials. Elsevier. 382(9894):769-79. [PubMed.]
- Jakubczyk K, et al. (2020) Antioxidant Potential of Curcumin-A Meta-Analysis of Randomized Clinical Trials. Antioxidants. 9(11): 1092. [PubMed.]
- Shimizu K, et al. (2019) Anti-inflammatory action of curcumin and its use in the treatment of lifestyle-related diseases. Eur CardioL Rev. 14(2): 117-122. [Ref.]
- Moghadamtousi SZ, et al. (2014) A review on antibacterial, antiviral, and antifungal activity of curcumin. BioMed Res Int. [Ref.]
- Srivastava R, et al. (1986) Effect of curcumin on platelet aggregation and vascular prostacyclin synthesis. Arzneimittel-forschung. 36(4): 715-717. [PubMed.]
- Sadeghi N, et al. (2020) The effect of curcumin supplementation on clinical outcomes and inflammatory markers in patients with ulcerative colitis. Phytother Res. 34(5): 1123-1133. [PubMed.]
- Agarwal KA, et al. (2011) Efficacy of turmeric (curcumin) in pain and postoperative fatigue after laparoscopic cholecystectomy: a double-blind, randomized placebo-controlled study. Surg Endosc. 25(12): 3805-3810. [PubMed.]
- Kuptniratsaikul V, et al. (2014) Efficacy and safety of Curcuma domestica extracts compared with ibuprofen in patients with knee osteoarthritis: a multicenter study. Clin Interv Aging. 9: 451-459. [PubMed.]
- Chandran B, Goel A. (2012) A randomized, pilot study to assess the efficacy and safety of curcumin in patients with active rheumatoid arthritis. Phytother Res. 26(11): 1719-1725. [PubMed.]
- Prabhakar A, et al. (2013) Comparison of antibacterial efficacy of calcium hydroxide paste, 2% chlorhexidine gel and turmeric extract as an intracanal medicament and their effect on microhardness of root dentin: an in vitro study. Int J Clin Pediatr Dent. 6(3): 171-177. [PubMed.]
- Khetarpal S, Bansal A, Kukreja N. (2014) Comparison of Anti-Bacterial and Anti-Inflammatory Properties of Neem, Curcumin and Aloe Vera in Conjunction with Chlorhexidine as an Intracanal Medicament-an In-Vivo Study. Dent J Adv Stud. 2(3): 130-137. [Ref.]
- Jorge-Araújo ACA, et al. (2018) Effect of Premedication with Anti-inflammatory Drugs on Post-Endodontic Pain: A Randomized Clinical Trial. Braz Dent J. 29(3): 254-260. [PubMed.]
- Langley G, Sheppeard H. (1985)The visual analogue scale: its use in pain measurement. Rheumatol int. . 5(4): 145-148. [PubMed.]
- Jensen MP, Chen C, Brugger AM. (2003) Interpretation of visual analog scale ratings and change scores: a reanalysis of two clinical trials of postoperative pain. J Pain. 4(7): 407-414. [PubMed.]
- Karapinar-Kazandag M, Tanalp J, Ersev H. (2019) Effect of Premedication on the Success of Inferior Alveolar Nerve Block in Patients with Irreversible Pulpitis: A Systematic Review of the Literature. BioMed Res. Int. [PubMed.]
- Allegretti CE, et al. (2016) Anesthetic efficacy in irreversible pulpitis: a randomized clinical trial. Braz. Dent J. 27: 381-386. [PubMed.]
- De Geus JL, et al. (2018) Effects of Ibuprofen Compared to Other Premedication Drugs on the Risk and Intensity of Postendodontic Pain: A Systematic Review. Eur Endod J. 3(3): 123-133. [PubMed.]
- Wahlström B, Blennow G. (1978) A study on the fate of curcumin in the rat. Acta pharmacologica et toxicologica. 43(2): 86-92. [PubMed.]
- Zanjani TM, et al. (2014) The attenuation of pain behavior and serum COX-2 concentration by Curcumin in a rat model of neuropathic pain. Korean J Pain. 27(3): 246-252. [PubMed.]
- Drobnic F, et al. (2014) Reduction of delayed onset muscle soreness by a novel curcumin delivery system (Meriva®): a randomised, placebo-controlled trial. J Int Soc Sports Nutr. 11(1): 1-10. [PubMed.]
- Anand P, et al. (2007) Bioavailability of curcumin: problems and promises. Molecular pharmaceutics. 4(6): 807-818. [PubMed.]
- Bisht S, et al. (2007) Polymeric nanoparticle-encapsulated curcumin (" nanocurcumin"): a novel strategy for human cancer therapy. J nanobiotechnol. 5(1): 3. [Ref.]
- Mohammadi Z. (2008) Sodium hypochlorite in endodontics: an update review. Int Dent J. 58(6): 329-341. [Ref.]
- Sadaf D, Ahmad MZ. (2014) Factors associated with postoperative pain in endodontic therapy. Int J Biomed Sci. 10(4): 243-247. [PubMed.]
- Malamed SF. (2004) Handbook of local anesthesia: Elsevier Health Sciences. [Ref.]
- Elkhadem A, et al. (2018) The effect of preoperative oral administration of prednisolone on postoperative pain in patients with symptomatic irreversible pulpitis: a single-centre randomized controlled trial. Int Endod J. 51 Suppl 3: e189-e196. [PubMed.]
- Jenarthanan S, Subbarao C. (2018) Comparative evaluation of the efficacy of diclofenac sodium administered using different delivery routes in the management of endodontic pain: A randomized controlled clinical trial. J Conserv Dent. 21(3): 297-301. [PubMed.]
- Sharma RA, Steward WP, Gescher AJ. (2007) Pharmacokinetics and pharmacodynamics of curcumin, in The molecular targets and therapeutic uses of curcumin in health and disease. Springer. 453-470. [Ref.]
- Praveen R, Thakur S, Kirthiga M. (2017) Comparative evaluation of premedication with ketorolac and prednisolone on postendodontic pain: a double-blind randomized controlled trial. J Endod. 43(5): 667-673. [PubMed.]
- Wali A, et al. (2012) Effectiveness of premedication with analgesics vs placebo for success of inferior alveolar nerve block in irreversible pulpitis. Pain. 26(31): 32. [Ref.]
- Modaresi J, Dianat O, Mozayeni MA. (2006) The efficacy comparison of ibuprofen, acetaminophen-codeine, and placebo premedication therapy on the depth of anesthesia during treatment of inflamed teeth. Oral Surg Oral Med Oral Pathol Oral Radiol and Endod. 102(3): 399-403. [PubMed.]
- Smith EA, et al. (2017) Nonsteroidal anti-inflammatory drugs for managing postoperative endodontic pain in patients who present with preoperative pain: a systematic review and meta-analysis. J Endod. 43(1): 7-15. [PubMed.]