>Corresponding Author : Thomas M Johnson
>Article Type : Research Article
>Volume : 3 | Issue : 1
>Received Date : 20 Oct, 2023
>Accepted Date : 3 Nov, 2023
>Published Date : 10 Nov, 2023
>DOI : https://doi.org/10.54289/JDOE2300102
>Citation : Bumpers AP, Wilson JP, Retrum JK, Pfaff AS, Ryser AS, et al. (2023) Preservation of Alveolar Dimensions at Molar Immediate Implant Sites Using Laser-Assisted Clot Stabilization: A Report of Four Consecutive Cases with One to Three Years of Follow-Up. J Dent Oral Epidemiol 3(1): doi https://doi.org/10.54289/JDOE2300102
>Copyright : © 2023 Bumpers AP, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Research Article | Open Access
1Department of Periodontics, United States Army Dental Health Activity, Fort Jackson, SC, USA
2Private Practice, McKenzie Periodontics and Implant Dentistry, Columbia, SC, USA
3Department of Periodontics, United States Army Dental Health Activity, Fort Riley, KS, USA
4Department of Periodontics, United States Army Dental Health Activity, Fort Wainwright, AK, USA
5Department of Prosthodontics, Army Postgraduate Dental School, Postgraduate Dental College, Uniformed Services University, Fort Eisenhower, GA, USA
6Department of Periodontics, Army Postgraduate Dental School, Postgraduate Dental College, Uniformed Services University, Fort Eisenhower, GA, USA
*Corresponding author: Thomas M Johnson, Department of Periodontics, Army Postgraduate Dental School, Postgraduate Dental College, Uniformed Services University, Fort Eisenhower, GA, USA
Abstract
Objective: Immediate implant placement into a molar extraction socket may hasten return to masticatory function and reduce overall treatment time. Placement of a graft or biomaterial in the peri-implant gap defect (PGD) has been associated with superior treatment outcomes. The purpose of this report is to present four cases demonstrating use of laser-generated blood clots to stabilize freeze-dried bone allografts (FDBAs) at molar immediate implant sites.
Methods: Four patients with non-restorable mandibular first molars presented to the Department of Periodontics, Army Postgraduate Dental School, Uniformed Services University, Fort Eisenhower, GA, USA. The hopeless teeth were extracted without flap reflection, and dental implants were installed in each socket. FDBAs were applied in the PGDs. In one case, a cover screw was utilized, and the implant was submerged under a laser-generated clot. In the remaining cases, transmucosal healing abutments were installed.
Results: Favorable healing was observed in all cases, each patient reporting minimal discomfort limited to the first two postoperative days. At the submerged implant site, > 2 mm buccal bone thickness was noted at re-entry. In the remaining cases, keratinized peri-implant mucosa was in contact with the healing abutment at the one-week follow-up appointment. All implants exhibited interproximal radiographic bone levels coronal to the first implant thread at every follow-up assessment.
Conclusions: Whether infrared lasers enhance healing at immediate implant sites remains an open question in implantology. However, the presented cases demonstrate that a neodymium-doped yttrium aluminum garnet laser can reliably stabilize particulate bone allografts in PGDs at immediate implant sites exhibiting large horizontal defect dimensions.
Keywords: Tooth Loss; Dental Implants; Allografts; Lasers; Clinical Protocols; Treatment Outcome
Abbreviations: PGD: Peri-Implant Gap Defect, FDBA: Stabilize Freeze-Dried Bone Allografts, IIP: Immediate Implant Placement, Nd: YAG: Neodymium-Doped Yttrium Aluminum Garnet, FDBA: Freeze-Dried Bone Allograft
Background
Clinicians widely acknowledge that immediate implant placement (IIP) in the esthetic zone is a predictable therapy with the potential to enhance—or even optimize—clinical and patient-oriented outcomes, assuming appropriate case selection and careful technique [1-4]. However, advantages such as early return to masticatory function, reduced number of procedures, and high patient acceptance have also been attributed to IIP at molar sites [4-6]. A recent systematic review by Ragucci and colleagues reported 1-year molar immediate implant survival and success rates reaching 97% and 93%, respectively, although evidence supporting molar IIP remains mostly limited to case series [4-6]. Superior treatment outcomes have been associated with flapless surgery, graft placement in the peri-implant gap defect (PGD), one-stage implant placement, and allowance for a healing period without loading [4,6]. The purpose of this report is to present a technique for stabilizing graft material in PGDs at molar immediate implant sites using a neodymium-doped yttrium aluminum garnet (Nd:YAG) laser.
Materials and Methods
Patients in this report presented to the Department of Periodontics, Army Postgraduate Dental School, Postgraduate Dental College, Fort Eisenhower, GA, USA, and completed an informed consent process involving verbal and written components. Each patient elected IIP at a mandibular first molar site.
Case 1
A healthy female aged 51 years presented in December of 2021 with a non-restorable, fractured tooth #30. The tooth was removed without flap reflection, and a ø5 x 11.5 mm implant (Nobel Replace Conical Connection, Nobel Biocare, Zurich, Switzerland) was placed with insertion torque of 45 Ncm. A ø5 x 5 mm healing abutment was applied, and a freeze-dried bone allograft (FDBA) (Oragraft, LifeNet, Virginia Beach, VA, USA) was placed in the PGD. An Nd:YAG laser (3.6W, 550 μs, 20 Hz, 30 J applied) was used to establish a stable clot to contain the FDBA particles. Additionally, the operator applied 380 J (3.0W, 100 μs, 20 Hz) to the facial, occlusal, and palatal/lingual aspects of the site, with the fiber located ≈ 2-3 cm above the tissue (Table 1). Ibuprofen (400 mg) and acetaminophen (325 mg) were prescribed for analgesia, as needed, and chlorhexidine mouth rinse was used for plaque control until normal oral hygiene practices could be reinstated. Early healing was uneventful, and minimal changes in buccal alveolar ridge and mucosal contours were observed from baseline through definitive restoration (Figs. 1 and 2). After 22 months of follow-up, interproximal radiographic levels were at or beyond the polished collar of the implant.
Case 2
A healthy female aged 31 years presented in February of 2019 with a fractured fixed dental prosthesis (#30-#32) and minimal clinical crown height at tooth #30, which also exhibited failed root canal therapy (Fig. 4). Following extraction of tooth #30, an intact buccal cortex was noted. A ø5 x 13 mm implant (Nobel Replace Conical Connection, Nobel Biocare) was installed with a 35-Ncm torque, and a ø5 x 5 mm healing abutment was applied. The PGD received particulate FDBA (Oragraft, LifeNet), and a laser-generated clot was established using parameters described in Table 1 with a total of 374 J delivered (Fig. 3). Postoperative analgesics and oral hygiene instructions were also as described in Case 1. However, the patient additionally received amoxicillin (500 mg) three times daily for one week.
Early healing was uneventful. The definitive implant-supported restoration was delivered at postoperative week 16 (Fig. 4). After 3 years of follow-up, radiographic peri-implant bone levels appeared favorable (Fig. 5).

Table 1: Proposed technique for stabilizing freeze-dried bone allograft in peri-implant gap defects at molar i0mmediate implant sites
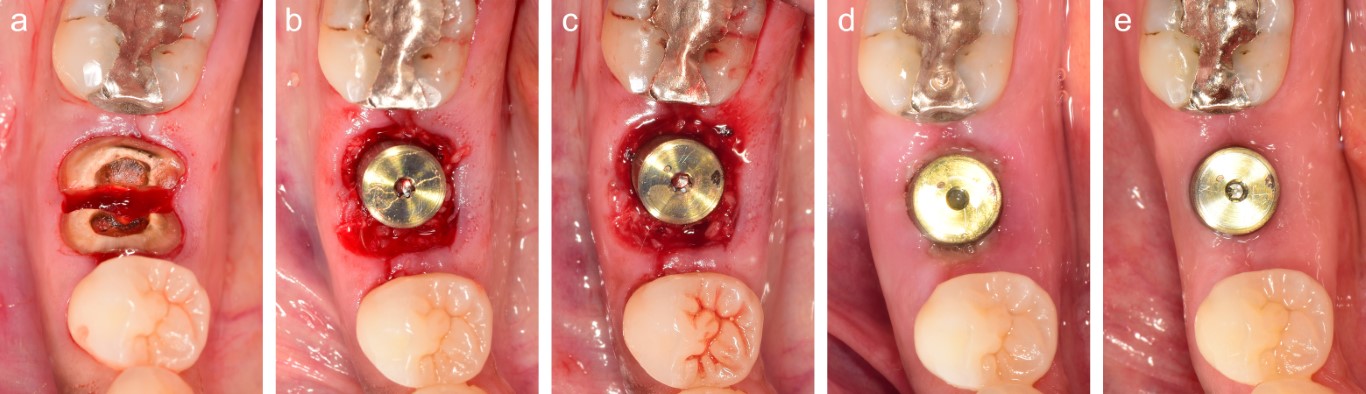
Figure 1: Case 1. 1a Tooth #30 sectioned. 1b Implant and healing abutment installed with particulate freeze-dried bone allograft (FDBA) in the peri-implant gap defect. 1c FDBA stabilized using a laser-generated clot. 1d Postoperative week one. 1e Postoperative week 12.
Case 3
A healthy male aged 25 years presented in April of 2022 with a fractured restoration and recurrent caries on tooth #19 (Fig. 6). After minimally traumatic extraction of tooth #19, a ø5 x 13 mm implant (Nobel Replace Conical Connection, Nobel Biocare) was placed with > 35 Ncm torque, and a ø5 x 5 mm healing abutment was applied. A particulate FDBA (Oragraft, LifeNet) was implanted in the PGD, and a laser-generated clot was established using the parameters described in Table 1, a total of 382 J delivered (Fig. 7). Analgesics and oral hygiene instructions were as described in Case 1. The patient received amoxicillin (500 mg) three times daily for one week, and healing progressed uneventfully. At postoperative month three, a provisional restoration was delivered. After 16 months of follow-up (Fig. 8), interproximal radiographic bone levels were at or coronal to the polished collar of the implant.
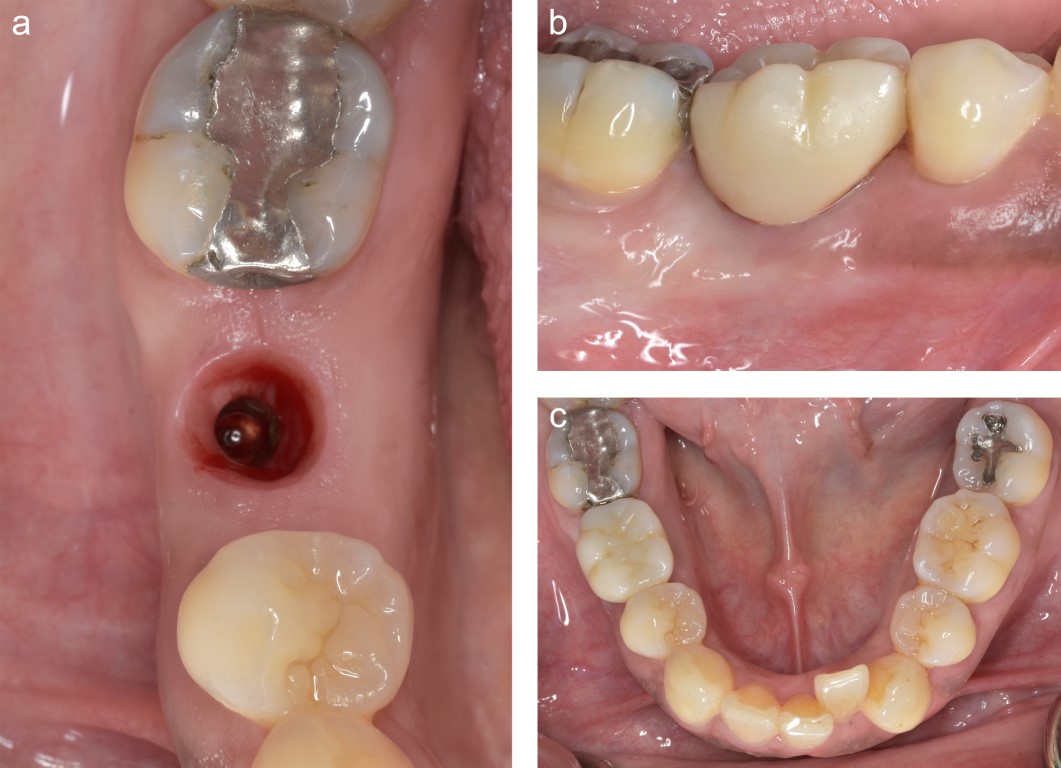
Figure 2: Case 1. 2a Appearance of the peri-implant mucosa at the time of implant restoration (postoperative week 36). 2b Definitive implant-supported crown. 2c Appearance of the mandible with implant supported crown in place. 2d Periapical radiograph at implant placement. 2e Periapical radiograph after 22 months of follow-up.
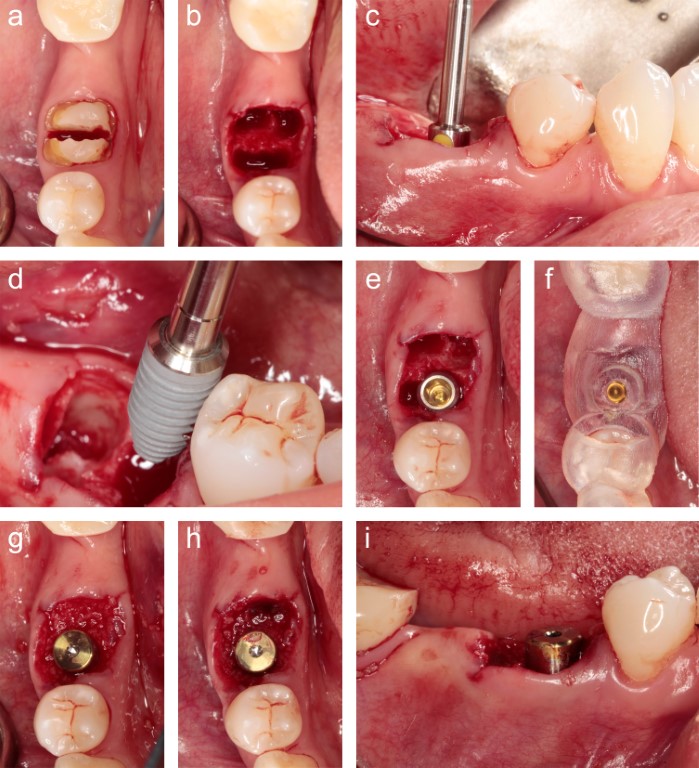
Figure 3: Case 2. 3a Tooth #30 sectioned. 3b Extraction socket. 3c Implant shaping drill corresponding to a platform depth of ≈ 3.5 mm apical to the buccal gingival margin. 3d Implant installation. 3e Implant stabilized in extraction socket. 3f Implant position confirmed with surgical template. 3g Particulate freeze-dried bone allograft (FDBA) placed in the peri-implant gap defect. 3h, 3i FDBA stabilized with laser-generated clot.

Figure 4: Case 2. Healing and definitive restoration. 4a Postoperative week one. 4b Postoperative week two. 4c through 4e Definitive restoration at postoperative week 16.
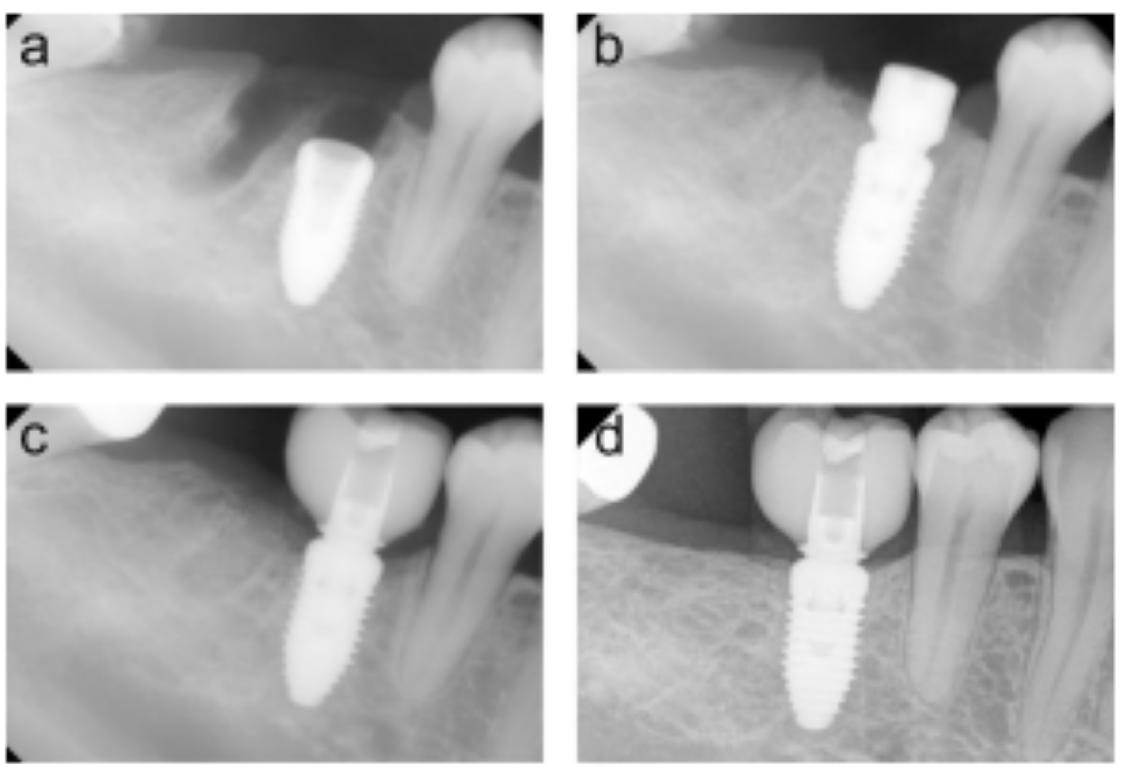
Figure 5: Case 2. Periapical radiographs. 5a Immediately after implant placement. 5b Immediately after freeze-dried bone allograft and healing abutment placement. 5c Definitive implant-supported crown at postoperative week 16. 5d Radiographic appearance after 3 years of follow-up.
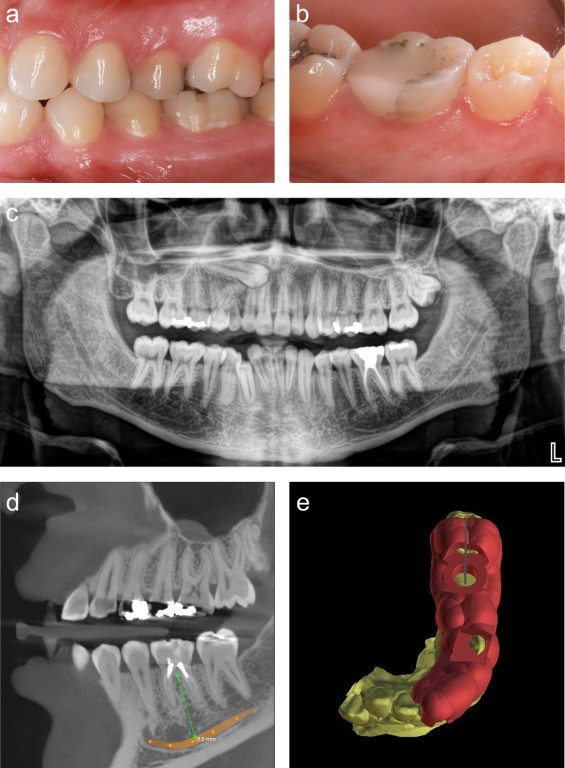
Figure 6: Case 3. 6a, 6b Baseline clinical appearance of tooth #19. 6c Panoramic radiograph. Tooth #6 was fully impacted, and tooth #C was over-retained. Tooth #16 was malpositioned and partially impacted. 6d Cone-beam computed tomography slice through the left posterior mandible. 6e Nonrestrictive surgical template used to confirm shaping drill and implant position. In addition to this nonrestrictive guide, a restrictive surgical template was used for the initial 2-mm osteotomy.
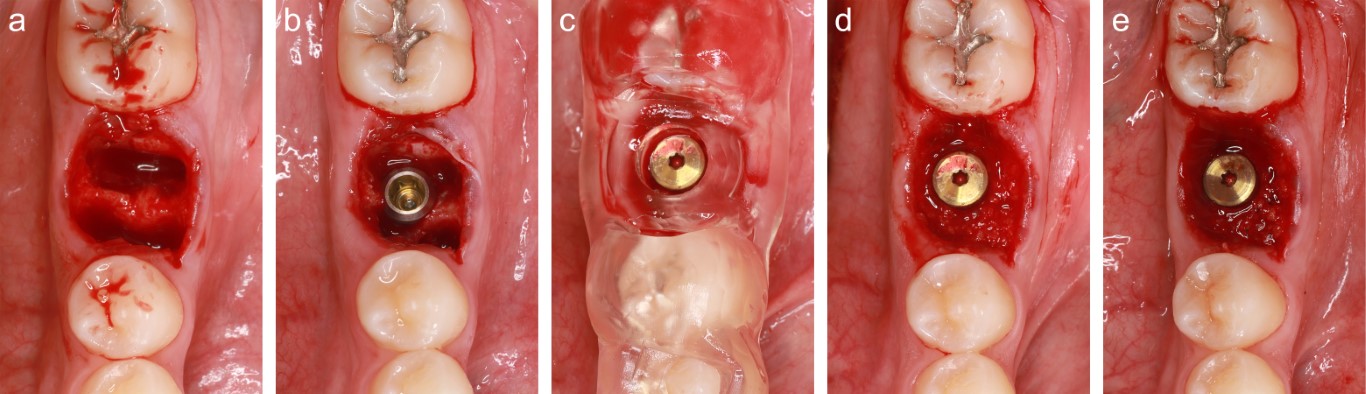
Figure 7: Case 3 surgery. 7a Extraction socket. 7b Implant stabilized. 7c Position confirmed with nonrestrictive surgical template. 7d Freeze-dried bone allograft (FDBA) placed in the peri-implant gap defect. 7e FDBA stabilized using a laser-generated clot.
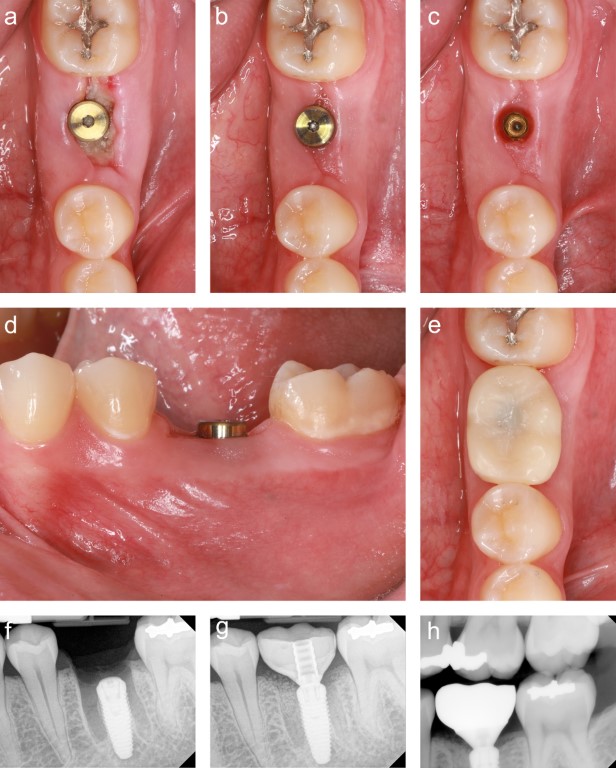
Figure 8: Case 3 healing. 8a Postoperative week one. 8b Postoperative week 12. 8c Appearance of peri-implant mucosa with healing abutment removed (postoperative week 12). 8d Postoperative week 12, buccal view. 8e Provisional implant supported crown in place. 8f Extraction socket with implant stabilized. 8g Provisional restoration at postoperative week 12. 8h Peri-implant bone level at postoperative month 16.
Case 4
A healthy male aged 44 years presented in May of 2022 with caries at tooth #18 (mesial) and recurrent caries at tooth #19 with evidence of failed root canal therapy. After extraction of tooth #19, a ø6.0 x 13 mm implant (Nanotite Tapered Certain, ZimVie, Warsaw, IN, USA) was installed (25 Ncm torque). The PGD received a particulate FDBA (Oragraft, LifeNet), and a laser-generated clot was established using the parameters described in Table 1, a total of 582 J administered (Fig. 9). Healing progressed uneventfully, and three months following implant placement, a ø6 x 5 mm healing abutment was inserted (Fig. 10). After 12 months of follow-up, radiographic peri-implant bone levels remained coronal to the first implant thread.
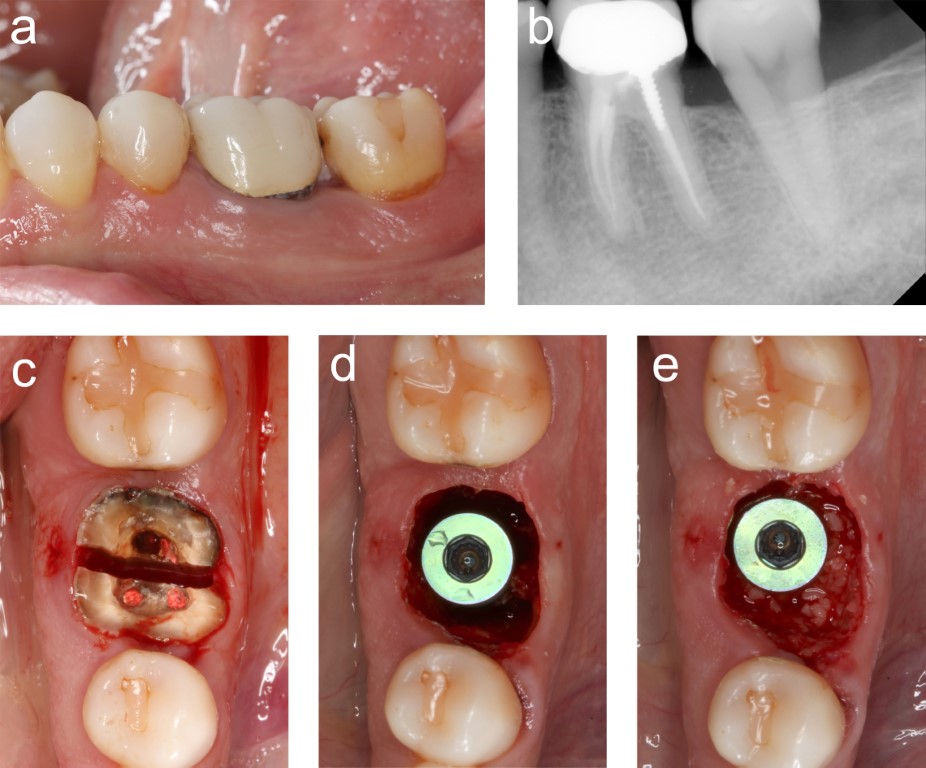
Figure 9: Case 4. 9a Baseline clinical appearance. 9b Baseline periapical radiograph demonstrating caries on the mesial of tooth #18 and recurrent caries on the distal of tooth #19. 9c Tooth #19 sectioned. 9d Implant stabilized in the extraction socket. Insertion torque was 25 Ncm. 9e Particulate freeze-dried bone allograft placed in the peri-implant gap defect.
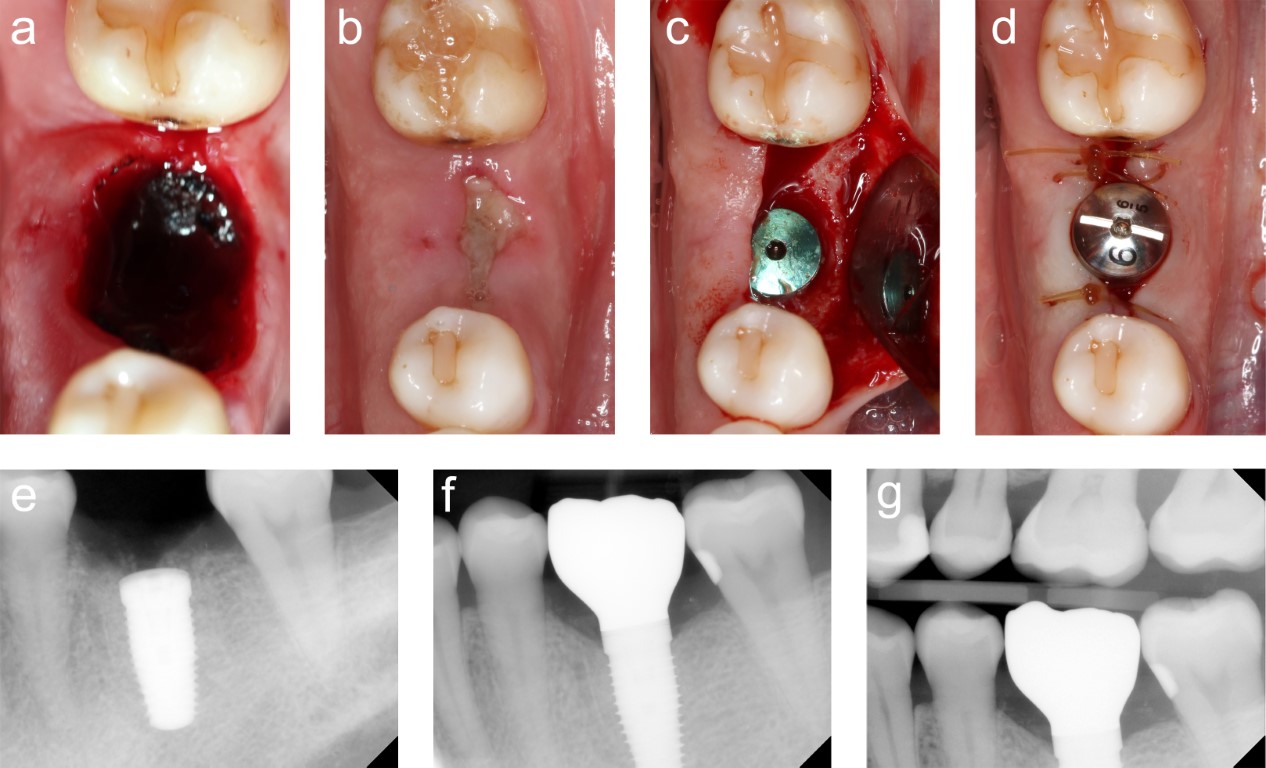
Figure 10: Case 4. 10a Laser-generated clot established over the cover screw and freeze-dried bone allograft particles. 10b Postoperative week one. Keratinized mucosa partially covered the extraction socket. The central portion of the socket was covered with a provisional matrix presumed to consist predominantly of fibrin. 10c, 10d Placement of the transmucosal healing abutment occurred at postoperative week 12. Upon re-entry, buccal bone thickness was > 2 mm. 10e Periapical radiograph at implant placement. 10f Periapical radiograph at placement of definitive implant-supported crown, postoperative week 16. 10g Bitewing radiograph after 12 months of follow-up. Interproximal peri-implant bone levels were coronal to the first thread, at the border between the polished collar of the implant and the roughened surface.
Results and Discussion
The objective of this report was to demonstrate use of laser-generated blood clots to stabilize FDBAs in PGDs at molar immediate implant sites. In all cases, early healing was favorable, and radiographic bone levels remained at or coronal to the first implant thread after 1 to 3 years of follow- up. Large PGD size is a feature distinguishing molar from non-molar immediate implant sites. Various approaches to PGD management at molar sites have been reported—no graft placement [7] or use of a dense polytetrafluoroethylene membrane [8], an absorbable membrane [9], a connective tissue graft [10], platelet rich fibrin [11], or granulation tissue obtained from the socket [12] to stabilize the graft/biomaterial. In each presented case, laser use to generate a blood clot required only 2 to 3 minutes, and each clot reliably contained the FDBA. Subjectively, healing of the peri-implant mucosa appeared advanced at the one-week assessment in each case.
Limited evidence from in vitro and animal studies has led to hypotheses that infrared laser energy stimulates osteoprogenitor cells [13], enhances bone regeneration [14], and improves osseointegration of dental implants [15]. Enhanced healing at immediate implant sites receiving infrared laser application has not been demonstrated in controlled clinical studies. However, the described clinical protocol is convenient and well accepted by patients. Previously, laser-generated clots were found to effectively contain bone biomaterials in PGDs at anterior and premolar immediate implant sites [16]. Despite the large horizontal defect dimensions encountered at molar immediate implant sites, Nd:YAG lasers appear to reliably establish clots that stabilize FDBA in the PGDs, based on observations from the presented cases.
This consecutive case series represents the first report demonstrating containment of a particulate bone biomaterial in PGDs at molar immediate implant sites using laser clot stabilization. Previous authors have suggested that infrared laser radiation may stimulate cells involved in hard and soft tissue healing. Whether Nd:YAG laser use at immediate implant sites enhances the clinical outcome remains unknown. However, the cases presented herein demonstrate that laser-generated blood clots reliably produce immediate graft containment and graft stability through the early postoperative period. Use of the laser to dry the pooled blood (3.0 W, 100 µs, 20 Hz, noncontact) appears essential for increasing clot stability. Controlled clinical research validating the presented technique is needed.
Acknowledgements
The authors gratefully recognize the prosthodontists who provided restorative treatment in the presented cases: Dr. Kellie S. O’Keefe (Case 2), U.S. Army Dental Health Activity, Fort Wainwright, Alaska, USA, and Dr. Kevin M. Lassiter (Case 4), U.S. Army Dental Health Activity, Fort Stewart, Georgia, USA.
Disclaimer: The views expressed in this manuscript are those of the authors and do not necessarily reflect the official policy of the United States Government, the Department of Defense, the Defense Health Agency, the Department of the Army, the United States Army Medical Department, or Uniformed Services University of the Health Sciences.
Author contribution statement: All authors have contributed substantially to conceptualization of the article, writing the original draft, critical review, and editing. All authors have approved the final version of the manuscript.
Disclosure statement: The views expressed in this manuscript are those of the authors and do not necessarily reflect the official policy of the United States Government, the Department of Defense, the Defense Health Agency, the Department of the Army, the United States Army Medical Department, or Uniformed Services University.
Conflict of interest statement: The authors report no financial, economic, or professional interests that may have influenced the design, execution, or presentation of this work.
Funding: The authors report no extramural funding for this work.
References
- Chu SJ, Salama MA, Salama H, Garber DA, Saito H, et al. (2012) The dual-zone therapeutic concept of managing immediate implant placement and provisional restoration in anterior extraction sockets. Compend Contin Educ Dent. 33(7): 524-532. [PubMed.]
- Cheng AW, Berridge JP, McGary RT, Erley KJ, Johnson TM. (2019) The extraction socket management continuum: A hierarchical approach to dental implant site development. Clin Adv Periodontics. 9(2): 91-104. [PubMed.]
- Chen ST, Buser D. (2014) Esthetic outcomes following immediate and early implant placement in the anterior maxilla -a systematic review. Int J Oral Maxillofac Implants. 29(Suppl): 186-215. [Ref.]
- Ragucci GM, Elnayef B, Criado-Cámara E, Del Amo FS, Hernández-Alfaro F. (2020) Immediate implant placement in molar extraction sockets: a systematic review and meta-analysis. Int J Implant Dent. 6(1): 40. [PubMed.]
- Urban T, Kostopoulos L, Wenzel A. (2012) Immediate implant placement in molar regions: risk factors for early failure. Clin Oral Implants Res. 23(2): 220-227. [PubMed.]
- Ketabi M, Deporter D, Atenafu EG. (2016) A systematic review of outcomes following immediate molar implant placement based on recently published studies. Clin Implant Dent Relat Res. 18(6): 1084-1094. [PubMed.]
- Atieh MA, Alsabeeha NH, Duncan WJ, de Silva RK, Cullinan MP, et al. (2013) Immediate single implant restorations in mandibular molar extraction sockets: a controlled clinical trial. Clin Oral Implants Res. 24(5): 484-496. [PubMed.]
- Johnson TM, Berridge JP, Baron D. (2017) Protocol for maintaining alveolar ridge volume in molar immediate implant sites. Clin Adv Periodontics. 7(4): 207-214. [PubMed.]
- Matarasso S, Salvi GE, Iorio Siciliano V, Cafiero C, Blasi A, et al. (2009) Dimensional ridge alterations following immediate implant placement in molar extraction sites: a six‐month prospective cohort study with surgical re‐entry. Clin Oral Implants Res. 20(10): 1092-1098. [PubMed.]
- Wilson Jr TG, Carnio J, Schenk R, Cochran D. (2003) Immediate implants covered with connective tissue membranes: human biopsies. J Periodontol. 74(3): 402-409. [PubMed.]
- Sun XL, Mudalal M, Qi ML, Sun Y, Du LY, et al. (2019) Flapless immediate implant placement into fresh molar extraction socket using platelet-rich fibrin: A case report. World J Clin Cases. 7(19): 3153. [Ref.]
- Liu Y, Chen Y, Chu C, Qu Y, Xiang L, et al. (2020) A prospective cohort study of immediate implant placement into posterior compromised sockets with or without primary wound closure of reactive soft tissue. Clin Implant Dent Relat Res. 22(1): 13-20. [PubMed.]
- Chellini F, Sassoli C, Nosi D, Deledda C, Tonelli P, et al. (2010) Low pulse energy Nd: YAG laser irradiation exerts a biostimulative effect on different cells of the oral microenvironment: An in vitro study. Lasers Surg Med. 42(6): 527-539. [PubMed.]
- Kim K, Kim IS, Cho TH, Seo YK, Hwang SJ. (2015) High-intensity Nd: YAG laser accelerates bone regeneration in calvarial defect models. J Tissue Eng Regen Med. 9(8): 943-951. [PubMed.]
- Karoussis IK, Kyriakidou K, Psarros C, Lang NP, Vrotsos IA. (2017) Nd: YAG laser radiation (1.064 nm) accelerates differentiation of osteoblasts to osteocytes on smooth and rough titanium surfaces in vitro. Clin Oral Implants Res. 28(7): 785-790. [PubMed.]
- Choi AY, Reddy CM, McGary RT, Hill RB, Swenson DT, et al. (2019) Adjunctive Nd: YAG laser irradiation for ridge preservation and immediate implant procedures: a consecutive case series. Clin Adv Periodontics. 9(3): 125-134. [PubMed.]