>Corresponding Author : Subash Chandra Raj
>Article Type : Case Report
>Volume : 4 | Issue : 1
>Received Date : 20 Feb, 2024
>Accepted Date : 05 March, 2024
>Published Date : 09 March, 2024
>DOI : https://doi.org/10.54289/JDOE2400105
>Citation : Raj SC, Tabassum S, Mishra AK and Pandia V. (2024) Prosthetic Rehabilitation of Post Covid Mucormycosis of Maxilla with Definitive Obturator Prosthesis- A 24 Month Follow Up Case Report. J Dent Oral Epidemiol 4(1): doi https://doi.org/JDOE2400105
>Copyright : © 2024 Raj SC, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Case Report | Open Access
Department of Periodontics, SCB Dental College and Hospital, Cuttack, Odisha, India
*Corresponding author: Subash Chandra Raj, Department of Periodontics, SCB Dental College and Hospital, Cuttack, Odisha, India
Abstract
The second wave of COVID-19 in April 2021 witnessed a new mutated variant of SARS-CoV2 known as B.1.617 resulting in Mucormycosis. Inhalation, ingestion, or contamination of ulcerated mucosa by fungal spores results in infection and cause Mucormycosis.
Objective: To highlight how a complex case of oral mucormycosis can be misdiagnosed due to its similar clinical presentations with other periodontal diseases and benefits of prosthetic rehabilitation of surgical defects with definitive obturator which improves the quality of life by restoring oral function and aesthetics.
Case report: A 35-year-old female reported with chief complaint of pain, pus and mobility in upper front teeth region of 2 months and swelling of mid-face. Darkening of skin, swelling with tenderness over bilateral malar- infraorbital regions with epiphora and blurred vision in right eye and discharge from right nostril. She had multiple abscess in attached gingiva in incisor and premolar region of maxilla having probing depths ≤ 4mm with mobility.
Conclusion: A precise diagnosis is prerequisite to specific treatment of any disease. Treatment often requires an extensive surgical resection causing facial deformation, masticatory, swallowing and speech problems. It is important to rehabilitate these patients by correcting the defects with the help of obturators and improve their lifestyle.
Keywords: COVID 19; Mucormycosis; Prosthesis; Obturator
Abbreviations: COVID: Coronavirus Disease, SARS-Cov: Severe Acute Respiratory Syndrome–Related Coronavirus, CBCT: Cone-Beam Computed Tomography, CT: Computed Tomography
Introduction
The second wave of Coronavirus disease 2019 (COVID-19) due to a new mutated variant of Severe acute respiratory syndrome–related coronavirus (SARS-CoV2) known as B.1.617 resulted in Mucormycosis known as “black fungus” in India [1]. It causes immunosuppression which leads to the development of new onset of diabetes which again is risk factor for oral mucormycosis [2].
In 1885, Paultauf first gave description about mucormycosis [3]. Inhalation, ingestion, or contamination of ulcerated mucosa or skin by fungal spores may result in infection and cause mucormycosis due to mucorales [4]. The fungal spores gain entry through the nasal cavity and infiltrate the orbit, paranasal sinuses and brain. Granulomatous lesions, painful ulcers, presence of abscess in gingiva or palate, mobility of teeth are some other oral clinical manifestations [5].
In this case report, the authors highlight how a complex case of oral mucormycosis can be misdiagnosed due to its similar clinical presentations with other periodontal diseases and benefits of prosthetic rehabilitation of surgical defects due to mucormycosis with definitive obturator which improves the quality of life by restoring oral function and aesthetics.
Case Report
A 35-year-old female reported with chief complaint of pain, pus discharge and mobility in upper front teeth region for 2 months and was associated with swelling of mid-face, darkening of skin, swelling with tenderness over bilateral malar and infraorbital regions with epiphora and blurring of vision in right eye and occasional discharge from right nostril. She had multiple abscess in attached gingiva in relation to incisor and premolar region of maxilla with probing depths ≤ 4mm with mobility (figure 1a-c).

Figure 1: Patient 1st visit (a) swelling of mid-face with darkening over bilateral malar and infraorbital region (b) & (c) multiple abscess, pus discharge and mobility in maxillary arch.
6 months back she was diagnosed with COVID-19, with type 2 diabetes mellitus (Haemoglobin A1c: HbA1c = 9.6). Concomitant treatment included oral hypoglycaemics (Metformin, Glimepiride) and systemic steroids (Prednisolone) for 8 weeks. After recovery from COVID 19, the patient still had uncontrolled blood glucose levels (HbA1c = 6.5), a raised Erythrocyte sedimentation rate ESR (112 mm in 1st hr) and CRP level (8.1 mg/dL), but normal D-dimer level (0.34 μg/mL).
Intraoral periapical radiograph (IOPA) and Cone-beam computed tomography (CBCT) analysis showed extensive destruction of alveolar bone from right second premolar to left first premolar with falling maxilla appearance. There was evident destruction of bone around bilateral infraorbital foramen and inferior nasal turbinate. Opacification with mucosal thickening seen in bilateral maxillary sinus and traces of erosion of infraorbital rim of right orbit (Figure 2d). In the non-contrast Computed tomography (CT) scan of paranasal sinus, mucosal thickening of bilateral maxillary sinus with bone erosion and infraorbital extension into right ethmoid air cells seen. In non-contrast CT scan of brain, the bilateral cerebral parenchyma appeared normal. Usually, the symptoms associated with post COVID oral mucormycosis are jaw pain, loosening of teeth mostly maxillary teeth, facial numbness and pain, blackish discoloration around nose and eyes, haziness of vision, black or blood discharge from nose. From the clinical findings along with radiographic correlation, the provisional diagnosis of post covid Mucormycosis of maxilla with differential diagnosis of osteomyelitis of maxilla following odontogenic infections was made.
Exuding pus from gingival abscess were sent for fungal analysis under Potassium hydroxide (KOH) mount which was inconclusive of Mucorales. A tissue specimen was incised from attached gingiva of left lateral incisor where exudation was present and sent for light microscopic analysis. It also came inconclusive of fungal elements and was only suggestive of granulation tissues. Inconclusive microbial investigations but with positive clinical and radiological findings increased the diagnostic dilemma for the case. To decrease the patient morbidity, surgical debridement of necrotic bones followed by antifungal medication was the treatment option selected and the patient was thus referred to mucormycosis ward for evaluation and surgical intervention was planned. A bilateral maxillectomy and inferior turbinectomy followed by aggressive debridement of necrotic bones was performed by a maxillofacial surgeon. To gain access to the necrotic infraorbital rim and zygomatic bone, lateral eyebrow approach was performed. Following debridement temporalis myocutaneous flap as a sinus obliterating material and for achieving primary closure was used (Figure 3e-f).

Figure 2: (d) CBCT showing extensive destruction of alveolar bone w.r.t 15-24 with falling maxilla appearance.
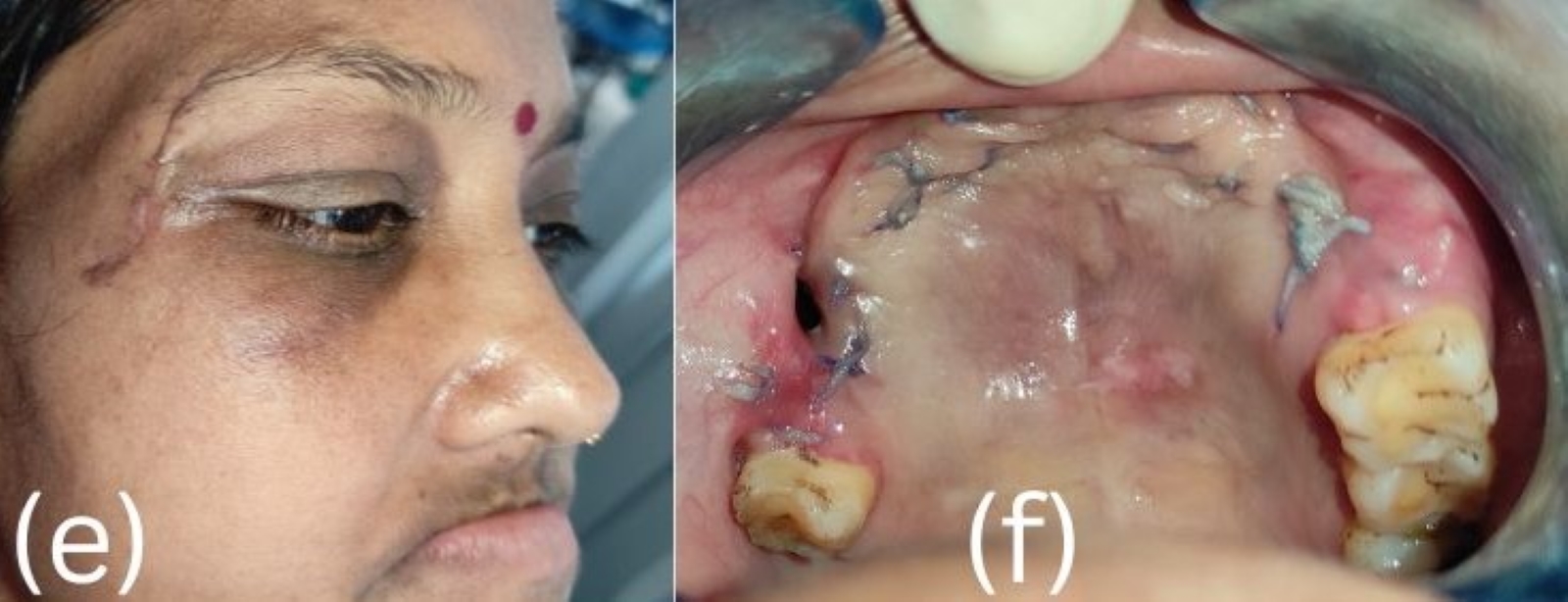
Figure 3: Post surgery (e) Lateral eyebrow approach to gain access to the necrotic infraorbital rim and zygomatic bone (f) Bilateral maxillectomy and inferior turbinectomy done.
The patient was prescribed paracetamol 500 mg, twice daily for a week for pain management. Medical management comprised of antifungal medication with liposomal Amphotericin-B, 5 mg/kg body weight in slow infusion for 10-12 hours for 14 days. Then oral Posaconazole, 300 mg twice daily for first day, followed by once daily for 28 days was initiated.
The histopathological examination of the deeper excised tissues revealed a collection of broad, ribbon like pauci-septate hyphae with branching at right angles and round fungal spores surrounded by necrotic tissues and a dark inflammatory infiltrate that was suggestive of invasive Mucormycosis of maxilla and paranasal sinuses.
Prosthetic rehabilitation: Following healing after 4 weeks, complete upper lip support was lost. In intraoral examination, Class IV Aramany defect with a small remnant oro-antral communication was noted in the right palatal aspect [6]. There was total loss of anterior maxilla concerning the missing teeth 11 to 16 on right side and 21 to 25 on left side. Prosthetic treatment options for acquired maxillary defect was discussed with patient: a) Implant supported prosthesis b) Interim acrylic obturator. There was severe bony defect in maxillary anterior region which requires extensive surgical procedure with bone graft and membrane placement before proceeding for implant surgery. Patient was not interested for another extensive surgical procedure and cost of the implants an issue for her also, so patient preferred an acrylic obturator for replacing her missing teeth. For rehabilitation of missing teeth, the devised prosthetic plan consisted of precautionary preliminary impressions of both arches. A custom tray was fabricated for the maxillary arch and secondary impression was made with light body addition silicone impression material. Jaw relation was recorded and teeth setting were done and the waxed-up obturator was tried in the patient for occlusal support, phonetics and aesthetics. C-clasps were constructed on tooth 17 and 26 for enhanced retention. The waxed-up obturator was processed using heat cured acrylic resin and further finished and polished for insertion. In final definitive obturator, post-insertion adjustments were made after 48 hours of denture insertion (Figure 4g-k). Following 2-year use of the obturator the patient was satisfied with the aesthetics and functional result of the prosthesis (Figure 5l-n). Destruction of maxillary bone is also stabilised and confirmed with post operative 2 years CBCT (Figure 6). Informed consent was obtained from the patient for publication purpose.

Figure 4: Prosthesis fabrication (g) Primary impression (h) Primary casts (i) Occlusal rim (j) Teeth Setting (k) Final obturator with clasp.

Figure 5: Follow up after 2 years (l) Extra oral view showing fullness of face (m) & (n) Intra oral view with obturator showing restoration of aesthetics & function.

Figure 6: 2-yr post operative CBCT.
Discussion
During COVID-19, the unsupervised use of corticosteroids and antibiotics caused drug-induced hyperglycemia [7-9]. At initial hospital visits, the dental symptoms were not addressed and priority was given to nasal or sinus symptoms. The absence of the pathognomonic eschar feature in our case along with mere presence of generalised grade 3 mobile teeth and swelling leads to an erroneous diagnosis of advanced periodontitis. Advanced destruction of alveolar bone associated with single arch in short period of time but with probing depth ≤ 4 mm made us think about other possible disease spectrum.
As bilateral partial maxillectomy and inferior turbinectomy followed by aggressive debridement of necrotic bones with intraoral approach was done for the patient, it was not feasible to place implant or any other means of replacement of missing teeth. We followed up the case after review and suture removal and obturator was fabricated for restoring the oral function and aesthetics of patient. A simultaneous prosthetic rehabilitation of missing teeth and closure of Oro-antral communication was achieved in this patient with an acrylic definitive obturator prosthesis.
Partial or complete maxillectomy which would break the antral floor should be done to manage a case of maxillary mucormycosis as maxillary antrum is considered a vital reservoir of the pathogen [10]. Partial maxillectomy and removal of portion of the hard palate in this patient resulted in hyper nasal speech, masticatory difficulties with chance of fluid leakage through the nose post-surgery. The prosthetic treatment in this patient differs from regular maxillofacial patients as there was collapse of face around lip area which was imposing psychological and social disability. The aim was to eliminate the oro antral communication by obturator, providing adequate functions of chewing, swallowing, and speech and aesthetic appearance. An accurate impression of the basal tissues and adjacent teeth is made to make a denture which will provide good retention, stability, and support [11]. Even after addition of excessive acrylic material to the labial flange, the anterior bone defect could not be compensated. Replacing the anterior missing teeth with larger artificial teeth would not be aesthetically acceptable. So, we planned open bite in anterior region which was quite acceptable by her. Following 2-year use of obturator, the patient is satisfied leading a comfortable life with normal speech and with proper mastication. The obturator fabricated was comfortable to use which helped in improvement in speech with good retention post obturator placement [12,13]. There is fullness of face around upper lips and change in the facial profile of the patient which relieved of psychological distress. Thus, it improved her lifestyle with proper aesthetic and function.
Conclusion
A precise diagnosis is a prerequisite to specific treatment of any disease. These cases with rare presentation which mimics advanced periodontitis without any hallmark features clinically shows importance of further investigations that should be done to look into differential diagnosis. The treatment of invasive mucormycosis often requires an extensive surgical resection causing facial deformation, masticatory problems, swallowing, speech, etc. This deteriorates the quality of general and oral health causing psychological distress. It is thus important to rehabilitate these patients by improvement of these defects with the help of obturators and improve their lifestyle.
Acknowledgement: None
Conflicts Of Interest: The authors declare no conflict of interest.
References
- Samarasekera U. (2021) India grapples with second wave of COVID-19. Lancet Microbe. 2: e238. [Ref.]
- Duffy J, Harris J, Gade L, Sehulster L, Newhouse E, et al. (2014) Mucormycosis outbreak associated with hospital linens. The Pediatric infectious disease journal. 33(5): 472-476. [PubMed.]
- Paltauf A. (1885) Mycosis mucorina) ein Beitrag zur Kenntnis der menschlichen Fadinpilzerkrankungen. Virch Arch Path Anat Physiol. 102(3): 543-564. [Ref.]
- Rai S, Misra D, Misra A, Jain A, Jain P, et al. (2018) Palatal mucormycosis masquerading as bacterial and fungal osteomyelitis: A rare case report. Contemp Clin Dent. 9(2): 309-313. [Ref.]
- Reddy SG, Kumar KK, Sekhar CP, Reddy RB. (2014) Oral mucormycosis: Need for early diagnosis!! J NTR Univ Health Sci. 3(2): 145-147. [Ref.]
- Bhasin AS, Singh V, Mantri SS. (2011) Rehabilitation of patient with acquired maxillary defect, using a closed hollow bulb obturator. Indian J Palliat Care. 17(1): 70-73. [Ref.]
- Coutinho AE, Chapman KE. (2011) The anti-inflammatory and immunosuppressive effects of glucocorticoids, recent developments and mechanistic insights. Mol Cell Endocrinol. 335(1): 2-13. [Ref.]
- Garg D, Muthu V, Sehgal IS, Ramachandran R, Kaur H, et al. (2021) Coronavirus disease (Covid-19) Associated Mucormycosis (CAM): case report and systematic review of literature. Mycopathologia. 186(2): 289-298. [PubMed.]
- Ahmadikia K, Hashemi S, Khodavaisy S, Getso M, Alijani N, et al. (2021) The double-edged sword of systemic corticosteroid therapy in viral pneumonia: a case report and comparative review of influenza-associated mucormycosis versus COVID-19 associated mucormycosis. Mycoses. 64(8): 798-808. [PubMed.]
- Arafat Y, Kumar YN, Bharani K, Balaji K, Varadarajan S, et al. (2021) COVID19-related Mucormycotic Osteomyelitis of the Maxilla: A Case Report of Findings, Surgical Management and Post-surgical Rehabilitation. World J Dent. 12(5): 423-426. [Ref.]
- Ravi MB, Srinivas S, Silina E, Sengupta S, Tekwani T, et al. (2022) Prosthetic Rehabilitation of Rhino Orbital Mucormycosis Associated with COVID-19: A Case Series. Clin Cosmet Investig Dent. 14: 1-10. [Ref.]
- Nilanonth S, Shakya P, Chotprasert N, Srithavaj T. (2017) Combination prosthetic design providing a superior retention for mid-facial defect rehabilitation: a case report. J Clin Exp Dent. 9(2): e590-e594. [Ref.]
- Vero N, Mishra N, Singh BP, Singh K, Jurel SK, Kumar V, et al. (2015) Assessment of swallowing and masticatory performance in obturator wearers: a clinical study. J Adv Prosthodont. 7(1): 8-14. [Ref.]