>Corresponding Author : Lim Chee Min
>Article Type : Research Article
>Volume : 2 | Issue : 1
>Received Date : 14 March, 2022
>Accepted Date : 28 March, 2022
>Published Date : 31 March, 2022
>DOI : https://doi.org/10.54289/JORVC2200104
>Citation : Min LC, Ariffin N, Hong HS. (2022) Case Series of Parinaud’s Oculoglandular Syndrome Caused by Fungal Infection. J Ophthalmic Res Vis Care 2(1): doi https://doi.org/10.54289/JORVC2200104
>Copyright : © 2022 Min LC, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Research Article | Open Access
Department of Ophthalmology, Hospital Sultanah Aminah Johor Bahru
*Corresponding author: Lim Chee Min, Department of Ophthalmology, Hospital Sultanah Aminah Johor Bahru
Abstract
We report 5 cases of fungal-related Parinaud’s oculoglandular syndrome (POS), presenting to Hospital Sultanah Aminah from June 2017 to June 2019. This is a retrospective case series. Four patients presented with unilateral POS while another patient presented with unilateral granulomatous conjunctivitis which did not respond to a two-week course of oral doxycycline (4 patients) or a three-day course of oral azithromycin (1 patient). While all patients had contact with cats, only one had a history of being scratched by a cat. Three patient’s pet cats were receiving treatment for ‘Sporo’ skin infection by their veterinarians while another two patients had no history suggestive of their cats having active infection. The first patient who presented with POS following her cat scratching her leg, had a skin biopsy done and received a course of antifungal antibiotics from a dermatologist when it was discovered that the cat had a fungal skin infection. Both her leg skin lesion and POS completely resolved. Conjunctival biopsies were performed in other 4 patients at 2 weeks to 1 month after their first presentation in view of poor response to antibiotics.
Two patients’ conjunctival fungal culture and sensitivity showed a growth of Sporothrix schenkii. Both symptoms and conjunctival lesions resolved completely after taking a course of oral Itraconazole for 6 weeks (1 patient), 3 months (3 patients) and 4 months (1 patient). POS is most commonly caused by Bartonella hensalae infection related to a cat’s scratch. Detailed history taking is important in diagnosing infection by other microorganisms such as fungi especially when the lesion does not respond to conventional antibiotic therapy. Besides clinical monitoring, conjunctival culture and sensitivity support the diagnosis.
Keywords: fungal infection, Parinaud’s oculoglandular syndrome, sporotrichosis
Introduction
Parinaud’s oculoglandular syndrome (POS) is a rare medical condition characterized by unilateral granulomatous conjunctivitis associated with ipsilateral cervical and either pre or retro auricular lymph adenopathy [1]. It has been associated with different etiologic agents, including bacteria, viruses and fungi [2]. In fungal infections, the causative agents include sporotrichosis (Sporothrix schenckii), blastomycosis
(Blastomyces dermatitidis), and coccidioidomycosis (Coccidioides immitis) [1].
Materials and methods
We conducted a retrospective review of the clinical records of 5 patients with clinical and microbiological evidence of fungal related POS presenting to Hospital Sultanah Aminah from June 2017 to June 2019.
Results:
A total of 5 patients were diagnosed of fungal related POS within this study period.
The demographic features and other clinical information of these 5 fungal related POS patients are summarized in Table 1. The mean age of presentation is 45 (range 13-62 years). 4 out of 5 patients were in the middle-aged and elderly populations (47-62 years). 3 out of 5 cases were female. 2 out of 5 patients had underlying diabetes mellitus and hypertension while the rest had no systemic illness.
Table 1
| Case | Age | Gender | Medical illness | History of presenting illness | Cat exposure | Physical examination |
|---|---|---|---|---|---|---|
| 1 | 62 | Male | Nil | Painless left eye redness with eye discharge for 2 weeks | Kept a pet cat undergoing treatment for a skin lesion called 'sporo" | • Left conjunctival granuloma over tarsal and bulbar conjunctiva • No lymphadenopathy |
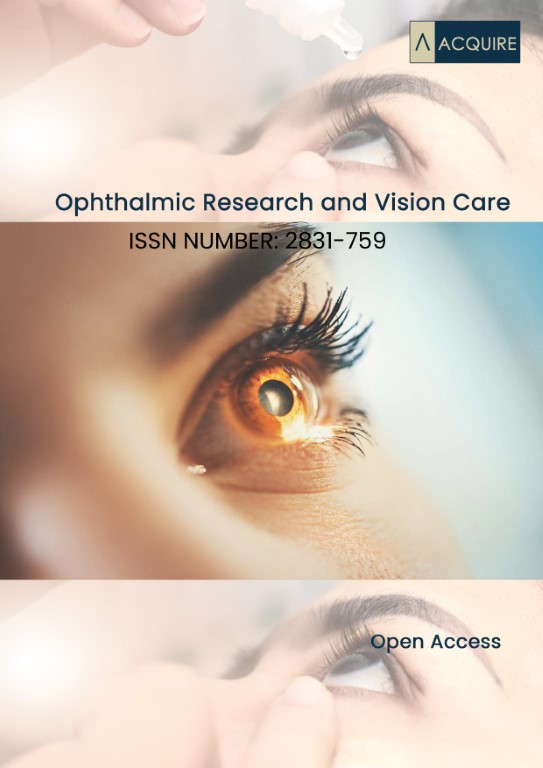
| 2 | 54 | Female | DM, HPT | Painful left eye redness, with eyelid swelling for 3 weeks | Kept a pet cat receiving treatment for ‘Sporo’ skin infection by veterinarian | • Left conjunctival granuloma over tarsal and bulbar conjunctiva (Figure 1 and 2) • Enlarged left preauricular lymph node |
| 3 | 13 | Female | Nil | Painful right eye redness with eye discharge for 3 days | • Had exposure to many cats at home
• No cat scatch or bite | • Right conjunctival granuloma over tarsal and bulbar conjunctival
• Enlarged right postauricular lymph node |
| 4 | 47 | Female | Nil | Left eye redness, swelling with itchiness for 1 week | • History of cat scratch over left leg 2 weeks prior to eye symptoms
• The cat was receiving treatment for ‘Sporo’ skin infection | • Left conjunctival granuloma over tarsal and bulbar conjunctiva
• Enlarged left preauricular lymph node |
| 5 | 50 | Male | DM, HPT | Painful right eye redness and swelling for 2 weeks | • Had pet cats at home
• No history of cat scratch or bite | • Right conjunctival granuloma over tarsal and bulbar conjunctiva (Figure 3 and 4)
• Enlarged right cervical lymph node |
4 patients presented with acute unilateral POS while another patient presented with acute unilateral granulomatous conjunctivitis without lymphadenopathy. While all patients had contact with cats, only 1 had a history of being scratched by a cat. 3 patient’s pet cats received treatment for ‘Sporo’ skin infection by their veterinarians while another 2 patients had no history suggestive of their cats having active infection. The first patient who presented with POS following her cat scratching her leg, had a skin biopsy done by a dermatologist which showed no growth from the culture. In other 4 patients conjunctival biopsies were performed at 2 weeks to 1 month after their first presentation in view of poor response to antibiotics. 2 patients’ conjunctival fungal culture showed a growth of Sporothrix schenkii while the other 2 patients’ conjunctival fungal culture yielded no growth. Bartonella serology was negative in all 5 patients.
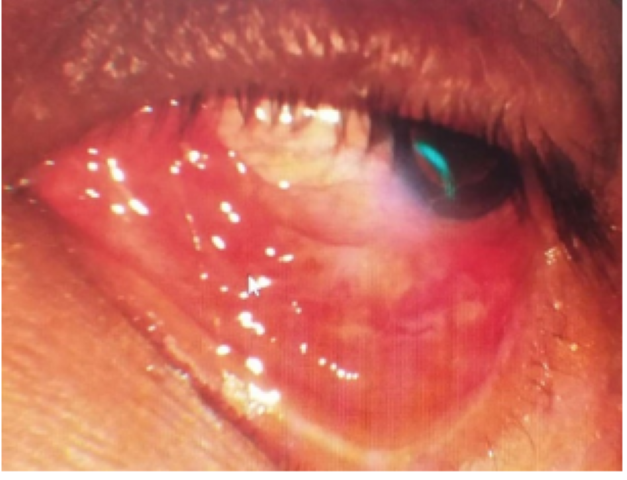
Figure 1:Granuloma over left lower tarsal and bulbar conjuntiva
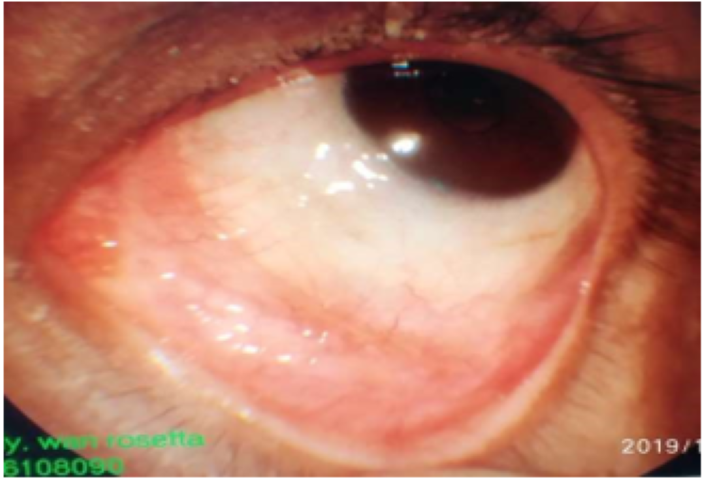
Figure 2:Complete resolution of left conjunctival granuloma
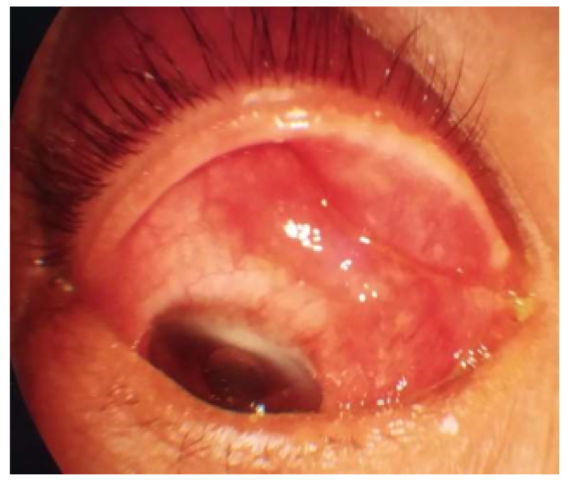
Figure 3:Granuloma over right upper tarsal and bulbar conjuntiva
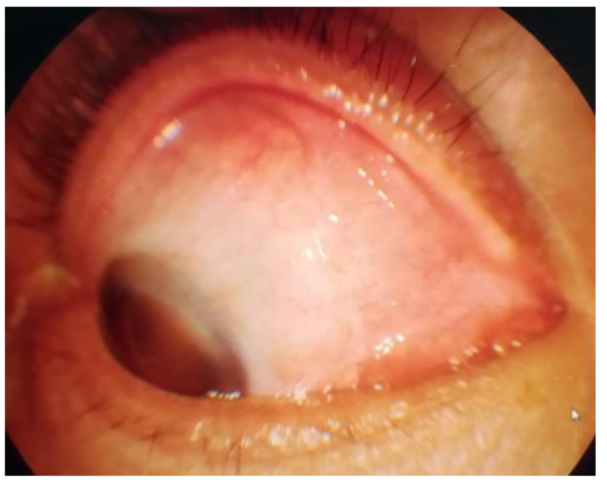
Figure 4:Complete resolution of right conjunctival granuloma
Both symptoms and conjunctival lesions resolved completely after taking a course of oral Itraconazole for 6 weeks (1 patient), 3 months (3 patients) and 4 months (1 patient).
Discussion
The most common cause of Parinaud’s oculoglandular syndrome (POS) has been cat scratch disease caused by Bartonella henselae infection. [1]. In this case series, 2 out of 5 cases were diagnosed of ocular sporotrichosis while 3 patients were clinically treated as fungal infection.
Sporotrichosis is an infection caused by fungi of the Sporothrix complex. It is a common plant saprophyte found in tropical and subtropical regions [3]. Sporotrichosis usually occurs by traumatic inoculation of soil, plants and organic matter contaminated with fungus [2]. Close interaction with cats plays a key role in transmission [2]. Cats constitute a reservoir of this agent as they have very close contact with contaminated soil and organic matter [2].
All 5 cases in this case series had exposure to cats. 1 patient received treatment for cutaneous sporotrichosis by dermatologist while 2 patients’ pet cats were treated as cutaneous sporotrichosis by their veterinarians. The diagnosis of fungal infection in POS is usually confirmed by isolation of fungus in culture, as in 2 cases in this case series. Another 3 patients were treated as fungal infection despite of negative finding in culture due to poor response to antibiotic. Treatment of fungal infection in POS is oral Itraconazole 100mg OD. Duration of antifungal varies depending on clinical condition, as in this case series, duration of antifungal ranges from 6 weeks to 20 weeks.
In conclusion. detailed history taking is important in diagnosing infection by other microorganisms such as fungi especially when the lesion does not respond to antibiotic therapy. Besides clinical monitoring, conjunctival culture supports the diagnosis.
Acknowledgements: Informed consent on the use of clinical details and photos in this case series were obtained from patients.
References
- Paulo S, Beatriz V, Raimunda V, et al. (2002) Parinaud’s Oculoglandular syndrome associated with Paracoccidioidomycosis. Rev. Inst. Med.trop.S. Paulo.44(1): 49-52. [PubMed.]
- Cassio P, Jose A, Ana C, et al. (2014) Parinaud’s oculoglandular syndrome associated with Sporothrix schenckii. IDCases 1: 38–39. [PubMed.]
- Thiago A, Celso T, Julia M, et al. (2018) Primary conjunctival sporotrichosis: Anatypical presentation of the disease. JAAD Case Reports. 4: 497-9. [PubMed.]