>Corresponding Author : Takesha Cooper
>Article Type : Research Article
>Volume : 2 | Issue : 1
>Received Date : 06 May, 2023
>Accepted Date : 22 May, 2023
>Published Date : 13 June, 2023
>DOI : https://doi.org/10.54289/JPPC2300101
>Citation : Cooper T, Ge S, Ijeaku I, Lee R, Moss HB, et al. (2023) Specific Adverse Childhood Experiences and Homelessness are Associated with Increased Risk for Attention Deficit Hyperactivity Disorder in a Nationally Representative Sample. J Pediatr Prim Care 2(1): doi https://doi.org/10.54289/JPPC2300101
>Copyright : © 2023 Cooper T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Research Article | Open Access
1Department of Psychiatry and Neuroscience; University of California, Riverside School of Medicine; 900 University Avenue, Riverside, CA 92521
2Division of Research Development; University of California, Riverside School of Medicine; 900 University Avenue, Riverside, CA 92521
*Corresponding author: Takesha Cooper, Department of Psychiatry and Neuroscience; University of California, Riverside School of Medicine; 900 University Avenue, Riverside, CA 92521
Abstract
This study examines associations of homelessness and specific Adverse Childhood Experiences (ACEs) on Attention Deficit Hyperactivity Disorder (ADHD). Unlike prior research focusing on the number of ACEs, our study hypothesized that there are specific types of high-risk ACEs associated with ADHD, and that homelessness further increased such risk association. Data samples obtained from the National Longitudinal Study of Adolescent to Adult Health, and measures of ACEs derived from measures used in the CDC-Kaiser ACE study were used to test the associations. Survey based logistic regression analysis identified which specific high-risk ACES were associated with ADHD. The specific high-risk ACEs were summed, then used with homelessness and demographics as covariates to adjust a survey based logistic regression model for the assessment of relative risk, namely the odds ratios of ACE scores and homelessness associated with ADHD. Three ACEs (sexual abuse, emotional abuse, and mental illness in the household) were associated with increased risk of ADHD by 67%, 76% and 89%, respectively. The addition of homelessness and any one of the identified high-risk ACEs was strongly associated with almost a 5.0-fold risk of lifetime ADHD diagnosis. The assessment of these ACEs and homelessness should be included when screening patients for ADHD.
Keywords: Attention Deficit Hyperactivity Disorder; Homelessness; Adverse Childhood Experiences; Childhood; Young Adulthood
Abbreviations: ADHD: Attention Deficit Hyperactivity Disorder, ACE: Adverse Childhood Experiences, AFDC: Aid to Families with Dependent Children, OR: Odds Ratio, CI: Confidence Interval, PTSD: Post-Traumatic Stress Disorder
Introduction
Attention Deficit Hyperactivity Disorder (ADHD) is a childhood-onset neurodevelopmental disorder that can lead to poor outcomes in education, occupation, social and financial arenas [1,2]. The core features of ADHD include inattention, impulsivity, and hyperactivity with impairment in at least two settings (i.e., school/work and home) and symptom onset before age twelve. The etiology of ADHD is thought to be multifactorial [3]. Children with ADHD face key challenges during seminal formative years and if not addressed, harmful long-term consequences may result. Although symptom onset of ADHD typically presents during childhood, approximately 50% of cases demonstrate continued impairment into adulthood [4]. ADHD prevalence rates range from 2.2% to 7.9% with worldwide community prevalence rate of 5% [5,6].
The 1998, CDC-Kaiser Permanente Adverse Childhood Experience (ACE) Study retrospectively and prospectively assessed the long-term impact of childhood abuse and/or household dysfunction by examining 10 different ACEs: maternal exposure to domestic violence, physical abuse, sexual abuse, emotional abuse, exposure to mental illness in the household, parental divorce/separation, substance abuse in the household, incarcerated family member, emotional neglect, or physical neglect. A dose-response relationship was reported between the number of indicators of these adverse exposures during childhood and several forms of morbidity and mortality in adults [7].
There is converging evidence that there is an association between ACEs and parent-reported ADHD [8,9]. A study using a nationally representative sample of children aged 4-17 years found that those with ADHD have higher ACE exposures compared to children without ADHD. ADHD was associated with 6 of 9 types of ACEs, two of which were further associated with ADHD severity. Like the majority of studies investigating the impact of ACEs on mental health, the report summed the scores of all nine ACEs, and used the total score to assess the risks of ACEs on ADHD. This approach presumed all ACEs make an equal contribution to ADHD, despite noting that ADHD was only associated with certain types of ACEs [8,9]. While the aforementioned study assessed the impact of ACEs on children, to our knowledge there are no extant studies which investigated this association using a representative sample that permits the exploration of the relationship between ACEs and ADHD in young adults at a national level using prospective data. Such data can provide insights to enhance both screening and the development of preventive and interventional strategies to more effectively address the high risk of ADHD among young adults.
Prior ACEs research has focused on either young cohorts with stable housing conditions or did not take into account the possibility that homelessness could confound the prevalence and risk estimates of ACEs and their associated outcomes [10]. Unfortunately, compared to those who were housed, the homeless cohort has extremely high ACE scores and more serious mental illness [11]. A recent study revealed that 55% of young homeless adults had more than 4 ACEs, the highest average noted was 4.41 ACEs for adults of 25-44 years. The researchers noted that these high ACE scores were strongly associated with the severe mental illness [12]. Given the potential association of homelessness with ACEs, our study compares the history of housing conditions (being housed vs. homeless) to quantitatively examine the impact of homelessness on the association between ACEs and ADHD.
In this study, we used a national representative longitudinal sample to test the following hypotheses: 1) We hypothesized that specific types of ACEs are associated with ADHD, the greater the number of these specific ACEs experienced, the greater the risk for ADHD among young adults; 2) We hypothesized that adjusting our models for history of homelessness versus having been housed, in addition to demographics, would reveal that the association between ACEs on ADHD would differ by housing conditions such that homelessness would contribute to this relationship. To our knowledge, this is the first study which utilized a nationally representative prospective sample to explore whether there is an association between specific ACEs and ADHD, and whether this association is affected by homelessness.
Materials and Methods
Study Sample and Design
We conducted a secondary analysis of data from the National Longitudinal Study of Adolescent to Adult Health (Add Health), a nationally representative prospective U.S. survey. Briefly, this survey first conducted in 1994-1995 (i.e., Wave I) with students in grades 7-12 who were followed prospectively now through five waves of data collection into adulthood [13]. Systematic multistage samplings were involved with clustering, stratification, and oversampling for represented national population with respect to region of the country, urbanicity, school size and type, and ethnicity.
Informed Consent
Prior to participation, all Add Health participants provided written informed consent in accordance with the University of North Carolina School of Public Health Institutional Review Board guidelines that are based on the Code of Federal Regulations on the Protection of Human Subjects 45CFR46: http://www.hhs.gov/ohrp/humansubjects/guidance45cfr46.html. These secondary data analyses from the Add Health restricted use dataset were approved by the University of California, Riverside Institutional Review Board.
Inclusion and Exclusion Criteria and the Analytic Sample
There was a total of 9421 young adults available for this analysis in Add Health across Waves I to IV consistent with the official Add Health documentation [14]. Certain groups of adolescents were over sampled, such as the parents of African American adolescents who completed college. Of these, 220 (2.3%) subjects were excluded from analyses if they responded “did not know” or “refused” when asked about homelessness during childhood or ADHD. In addition, 1598 (17.0%) subjects responded that they answered the questions in Waves I and II as “Not honestly at all” or “Somewhat honestly.” These were also excluded from the analyses over concerns about invalid responses in subsequent waves of data collection. A sensitivity analysis was conducted to examine the impact of these self-reported dishonest subjects. This analysis demonstrated that inclusion of these self-reported dishonest responders resulted in an underestimation of risks for ADHD and homelessness. (See supplementary data 1).
Measures
Adverse Childhood Experiences (ACEs)
The CDC-Kaiser ACE study identified 10 ACEs in various aspects of abuse, neglect, and household dysfunction [7]. In the Add Health Study, specific items in the Waves III and IV interview inquired about various types and amounts of adverse childhood experiences, as seen in Supplementary Table 1. These items were then used to map to the CDC-Kaiser ACE categories. Unfortunately, one item (“domestic violence towards a mother by a male partner”) could not be reconstructed from the Add Health items and therefore was excluded from our analysis. As a result, there were 9 ACEs found in Add Health data rather than the original 10 from the CDC-Kaiser study.
Presence of ADHD
The retrospective presence of ADHD was determined from the following question asked at Wave IV: “Has a doctor, nurse or other health care provider ever told you that you have or had: attention problems or ADD or ADHD?” Wave IV participants were 24 to 32 years old and having transitioned into young adulthood.
History of Homelessness
A retrospective history of homelessness was assessed in Wave III by asking participants, “Have you ever been homeless for a week or longer – that is, you slept in a place where people weren’t meant to sleep, or slept in a homeless shelter, or didn’t have a regular residence in which to sleep.” Participants who answered ‘yes’ were deemed having experienced homelessness (herein referred to as ‘homeless’) those who responded ‘no’ were deemed having been normally housed (herein referred to as ‘housed’). At Wave III, subjects were between 18 and 26 years old and reflected recall of homelessness sometime at or prior to this age.
Demographic variables
Ethnicity was self-reported and defined at Wave 1 as “White”, “Black”, “Hispanic” and “Others” (combined for races of Asian, Pacific Islander, and American Indian or Native American, due to the relatively small sample sizes).
Educational attainment was assessed at Wave III when subjects were age 18-26 years and was comprised of two levels: those who reported not going beyond a high school education and those attending at least some college or vocational training beyond high school.
Economic stress was reflected by the number of times their families received social welfare and/or public supports across the first three Waves of data, and included supports such as food stamps, Aid to Families with Dependent Children (AFDC), housing assistance, welfare payments, and unemployment insurance. Consequently, this variable was coded as 0, 1, and 2+ for families never, only once, and two or more times having received the public economic support, respectively.
Statistical Analysis
National sample weighted estimation of ADHD across sociodemographic factors, housing history, and individual ACEs:
The nationally representative sample weighted estimation was conducted using the survey-based frequency function in SAS 9.4, in which the region (i.e., the Northeast, the Middle West, the South, and the West in the U.S) was the stratification factor, and subject ID was the cluster factor. Contingency tables were constructed according to the binary outcomes for ADHD with either sociodemographic factors or each of the nine ACEs. Association was assessed with a Chi-square test. As a result, the nationally weighted estimation was reported as the sample weighted frequency and prevalence rate (%).
To identify which ACEs were specifically associated with ADHD, survey-based logistic regression was utilized in SAS 9.4, using the binary outcomes of ADHD as the dependent variable, and each of the single ACEs as the independent variable. The model was further adjusted by demographic and history of housing condition, thus estimating an adjusted association. As a result, any statistically significant ACE was identified as a specific ACE related to ADHD only if the ACE was strongly associated with ADHD in the adjusted model with a p-value < 0.05 for a 2-sided test.
After each specific ACE was identified as related to ADHD, that ACE was then scored as 1 for those who endorsed that specific ACE. For those not endorsing that specific ACE, the variable was coded as 0. Subsequently, these ACE scores were summed together as summary scores for specific ACEs, that is, the number of ACEs that were specifically associated with ADHD.
To assess how the risk for ADHD was associated with the sum scores of the identified specific high-risk ACEs and homelessness, the survey-based logistic regression models were built in 3 steps to estimate relative risk as odds ratio (OR):
1) We used ADHD as a binary outcome and the sum scores of high-risk ACEs as an independent variable (with a score of 0 as the control level) to see how ADHD unadjusted was associated with the summed scores of high-risk ACEs.
2) The binary outcomes for ADHD were employed as a dependent variable, both the sum scores of high-risk ACEs and homelessness were utilized as the independent covariates to see how ADHD was associated with the levels of summed high-risk ACEs and housing condition history. Whenever multiple comparisons were conducted, results were adjusted by the Dunnett method. These model-based assessments of the risks for ADHD were reported as odds ratio (OR), its 95% confidence interval (CI), and p-values.
Results
1. Sample Summary and National Trends of ADHD Characterized by Demographics
• It is noteworthy, that we utilized cluster-based samples with an unequal probability, therefore their estimations at population levels were sample weighted. Thus, simple percentages could not be used. Among the 7603 young adults in the study samples, 322 (4.2%) were self-reported as having ADHD. The sex distribution of this sample was 4332 females (57.0%) and 3271 males (43.0%). In terms of educational attainment in the samples, more young adults completed high school and subsequent professional training (4505; 59.3%) than completed only high school or below (3098, 40.7%). The ethnic distribution of subjects in the samples was 4296 Whites (56.5%), 1409 African Americans (18.5%), 1160 Hispanic/Latino (15.3%), and 738 “Others” (9.7%). Among these samples of young adults, the cohort size of those who experienced homelessness was 245 (3%).
• The sample-weighted overall rate of ADHD in the study population was 5.4% at the national level. Importantly, rates of ADHD were strikingly different between those who had experienced homeless (15.7%) and those who were housed (5.0%). The rates of ADHD also differed significantly across gender, race/ethnicity, and education level. As can be seen in Table 1, males had a higher rate of ADHD than females (7.9% vs 3.0%, p <0.0001), Whites had higher ADHD rates than African Americans or Hispanics respectively (6.5% vs 2.8% and 2.4%, p = 0.0004), and fewer subjects with ADHD attained an education beyond high school (4.1% vs 6.9%, p = 0.0004).
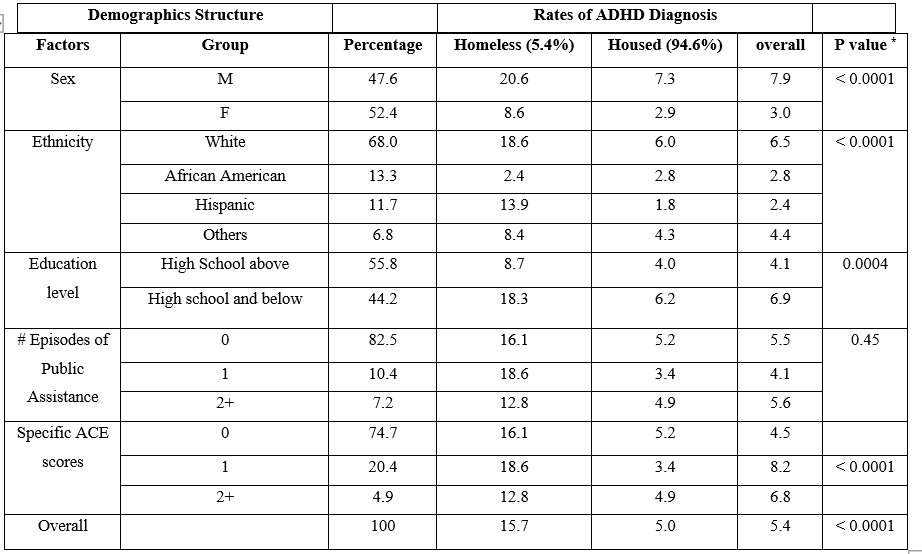
Table 1: Sample Weighted Prevalence Rates of ADHD during the Lifetime of Young Adults (24-32 years old) across Demographics Stratified by Housing History
Note: * p value was for association test if national weighted prevalence of ADHD diagnoses during lifetime of young adults of 24-32 years were different cross demographic groups.
2. Associations of Individual ACEs, Homelessness and ADHD
• As shown in Table 2, the ACE identified as emotional abuse was significantly associated with ADHD risk, with endorsement of emotional abuse increasing the odds by 76% (OR = 1.76; p = 0.006). Similarly, endorsement of sexual abuse was significantly associated with ADHD risk, with the odds increasing by 67% (OR = 1.67, p = 0.03). The endorsed ACE of the presence of mental illness in the household was also significantly associated with ADHD, with the odds increasing by 89% (OR = 1.89, p = 0.01). The other specific ACEs were not significantly associated with ADHD in this study.
• These high-risk ACEs (i.e., “emotional abuse”, “sexual abuse” or “mental illness in the household”) were summed and presented as 3 levels, i.e., 0, 1, and 2+, indicating none, only one, and at least two of these three specific ACEs that the young adults experienced through their first 18 years in life. Given the low number of young adults endorsing 3 or more ACEs (N = 35) this group was combined into the 2 or more ACEs group.
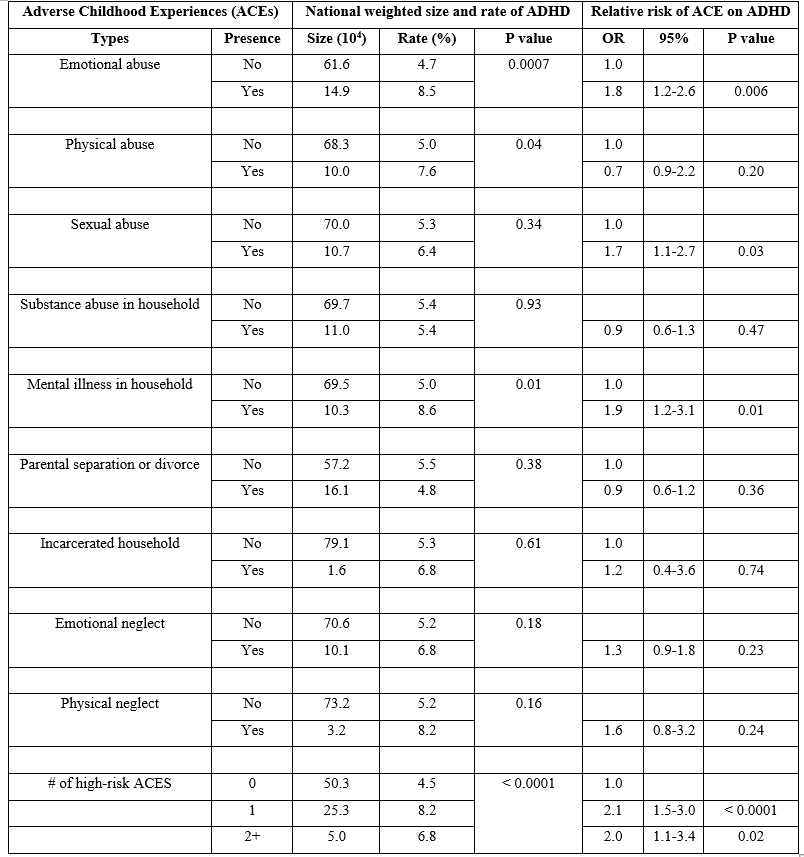
Table 2: Nationally Weighted Rates of ADHD and the Risk of ADHD Associated with Specific Types of ACEs
• Table 3 demonstrates that the cohort experiencing homelessness had higher ACE scores and higher ADHD prevalence rates than their housed peers. In other words, homelessness was associated with higher ACE scores and a higher risk of ADHD. It is noteworthy that 47.6% of the young adults who experienced homelessness had at least one specific ACE, compared to only 24.5% of those housed. Subjects who endorsed homelessness more frequently endorsed one high-risk ACE (34.1% homeless vs 20.0% housed, p <.0001) and two or more high-risk ACEs (13.5% homeless vs 4.6% versus housed, p < 0.0001), Additionally, subjects experiencing homelessness also endorsed higher rates of ADHD than those who were housed (15.7% vs. 5.0% respectively; p < 0.0001). Thus, the data suggests that those who endorsed homelessness had both higher ACE scores and higher rates of ADHD in comparison to the housed peers. Therefore, we took homelessness into account when further examining the association between ACE scores and ADHD.
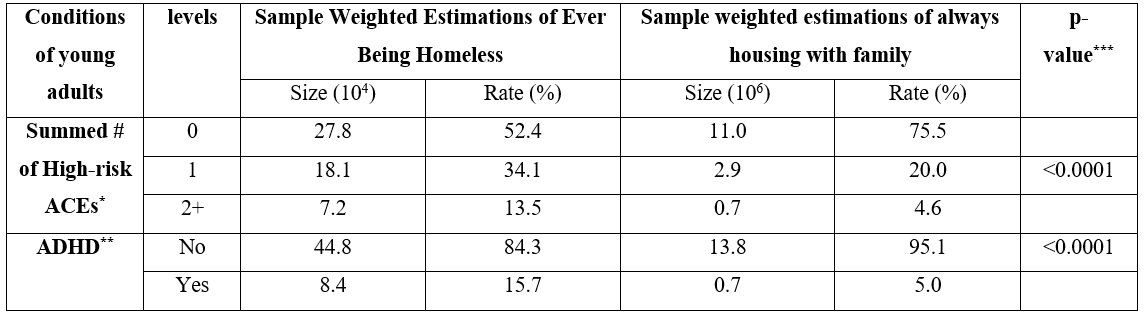
Table 3: Associations between Sample Weighted Estimations of Homelessness, the High-Risk ACE Summary Scores and the Presence of ADHD
* The rate was estimated to provide the sample representative sizes and percentages of those who scored ACEs as 0, 1, and 2+ among for the two cohorts, i.e., homelessness and housed, respectively.
** the rate was estimated to provide the representative sample sizes and percentages of those who were ever diagnosed as ADHD for the two cohorts as above, respectively.
*** p value reflects the sample weighted Chi-square test examining the association of housing condition history with ACEs scores and ADHD , respectively.
3. Risk assessment of ADHD associated with summed scores of specific high-risk ACEs and homelessness in the young adults.
• Table 4 depicts the results of a survey-based logistic regression model that examined concurrently ADHD risk associated with the sum of the high-risk ACE scores, and homelessness while controlling for demographics. It was found that having one or two of the high-risk ACES respectively were associated with a doubling for the risk of ADHD (OR = 2.1 and OR = 2.0), compared to the absence of these ACEs.
• The young adults who experienced homelessness were more than twice as likely (OR = 2.4) to also have ADHD, compared to their housed peers despite these young adults having the same demographic conditions and the high-risk ACE sum scores. Taken together, subjects who experienced both homelessness and at least one of the high-risk ACEs have approximately a five-fold risk of ADHD (estimated OR is approximately 2.1 x 2.4 = 5.0 for endorsing 1 high risk ACE and 2.0 x 2.4 = 4.8 for 2 or more high risk ACEs), compared to those who never experienced homelessness yet were exposed to the three high-risk ACEs.
Discussion
The results supported our hypothesis that among the ACEs studied, a subset of specific high-risk ACEs were significantly associated with ADHD. The specific high-risk ACEs associated with ADHD were sexual abuse, emotional abuse, and mental illness in the household. These specific ACEs increased the odds of ADHD by 67% (sexual abuse), 76% (emotional abuse) and 89% (mental illness in the household), respectively. It is unclear why these specific ACEs showed risk association with ADHD in our study. It may be that these specific ACEs are somehow more traumatic to normal development. Prior research has demonstrated sensitive developmental periods and that the specificity of these more traumatic ACE subtypes can lead to functional and volumetric changes in brain structures [15]. Longitudinal studies are needed to elucidate how and when exposure to the ACE subtypes of emotional abuse, sexual abuse and mental illness in the household might impact development and functioning of the cortical structures which underlie ADHD.
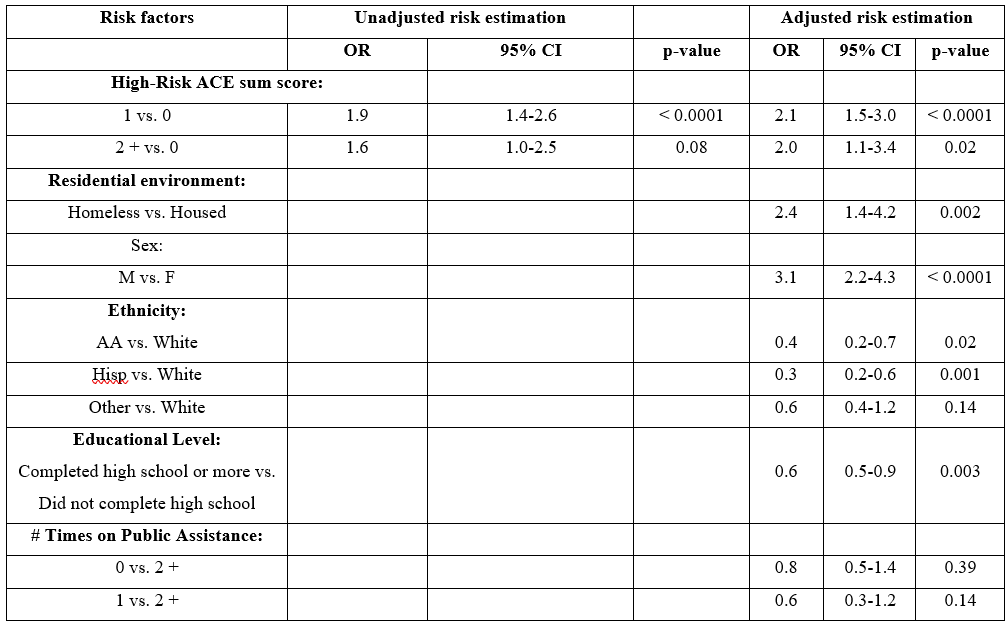
Table 4: Logistic Regression Estimates of ADHD Risk
Furthermore, our data suggests that if children experienced both homelessness and one of the specific high-risk ACEs, the odds for ADHD is increased by nearly 5.0-fold. Those who endorsed an experience of homelessness, had much higher ACE scores and a higher prevalence of ADHD. ACEs and homelessness may be the strongest predictors for ADHD and has important screening and clinical implications. To our knowledge, this is the first study to demonstrate an association between ADHD in young adulthood and ACEs and reveal that the experience of homelessness further elevated the associated risk for ADHD by 2.4 times, on average. Thus, homelessness amplified the association between ADHD and the high-risk ACEs. Based upon these findings, we believe that homelessness behaves as a potent adverse childhood experience that should be classified as an ACE and included minimally as a covariate in subsequent research on the impact of ACEs on child and adult development, as well as an additional item in clinical screening for ADHD.
Previously, the effects of ACEs on physical and mental health were commonly assessed by the summary score of all ACEs with little attention to the specific nature of the ACEs. The default assumption has been that all ACEs equally impact health outcomes and therefore could be linearly summarized to assess the magnitude of effects. However, in this study, we found that the impact of ACEs on ADHD was unequal, with three of the nine ACEs examined revealing robust association with ADHD. We found that having one, two or more endorsed specific ACEs resulted in an OR of about 2 for the risk of ADHD. Thus, we did not see the dose-response relationship noted in the CDC-Kaiser study, although our methodology was different in that we identified and examined specific high-risk ACEs [7]. Though speculative, it is possible that having at minimum one ACE could be sufficient to engage adaptive mechanisms such that additional insults were tolerated better and enhanced resilience against greater harm. Having more than one ACE might overwhelm adaptive mechanisms leading to pathology.
Several aspects of our findings offer confidence in the results. ADHD population prevalence rates vary from 2.2% to 7.9% with worldwide community prevalence rate of 5% [5,6]. Our sample had a similar ADHD prevalence rate of 5.35% consistent with that of the worldwide community. Compatible with the extant literature, our results show a higher prevalence of ADHD in males compared to females (7.92% versus 3.02%). Racial differences in our study were also consonant with findings in other studies which found that ADHD is more prevalent among Whites compared to other racial groups. In addition, ADHD as a neurodevelopmental disorder can present with symptoms that can lead to poor educational achievement and difficulty progressing educationally [1]. Consistent with these observations, individuals with ADHD in our study had significantly lower rates of education beyond high school than those without ADHD (4.12% vs 6.90%) suggesting that the presence of ADHD may have hindered the capacity of individuals to attain educational goals and academic achievement. Lastly, our findings converge with other reports associating ACEs with the risk for ADHD [8,9].
An additional consideration is that children who experience ACEs show symptoms that are similar to those of ADHD (difficulty focusing, behavioral disinhibition, restlessness etc.) [16]. Importantly, some symptoms of both the Inattentive and Hyperactive clusters of ADHD overlap with those of Post-Traumatic Stress Disorder (PTSD), therefore it is possible that highly traumatized subjects were mis-diagnosed [17]. Therefore, it is possible that some children with ACEs are unnecessarily treated for ADHD, when in fact they are experiencing behavioral and neurocognitive reactions to their life experiences. For some of these children, symptoms may disappear once the adversity is addressed. We believe it is paramount for pediatricians, child and adolescent psychiatrists and other health providers to carefully assess children’s exposure to ACEs (particularly emotional abuse, sexual abuse and mental illness in the household) and homelessness during assessment and follow-up to ensure an adequate and accurate diagnosis and subsequent treatment plan for the child and family.
Limitations:
There are several limitations to the interpretation of these secondary analyses of existing data. First, due to the lack of clearly delineated temporal ordering of the events of ADHD, homelessness, and ACEs in the Add Health data sets, we could not conduct an analysis to make causal inferences. Therefore, we could only rely on an associational analysis for this study. While conducting this association analysis, these three key variables were exchangeable, regardless of cause and outcome, thus allowing us to avoid collider effects [18,19]. By definition, a collider (e.g., ADHD) is the common outcome of the other two causal variables (e.g., ACEs and homelessness), when causal effects are estimated only from cause(s) to outcome(s). As opposed to causal inference, association analysis ignores the direction to estimate how the variables can happen consistently with positive or negative correlations. In particular, Add Health subject selection was not conditioned on these three factors; thus, the sample selection was not biased by these potential colliders. A collider effect is also often a source of concern when paradoxical findings appear in the data. We found no paradoxical associations between ACEs, ADHD, and homelessness.
An additional limitation of this research is that the presence of ADHD was derived from self-report and was not further validated by physicians or other mental health professionals. Thus, no formal psychiatric diagnosis of ADHD was performed nor were diagnoses confirmed by a clinician.
Since this study was conducted as a secondary analysis of existing data, the questionnaires in this survey were not specifically constructed for this study. The variables employed in this study are those chosen by others to address different goals, and the timing of ascertainment was determined by the researchers who developed the survey. In our case, we constructed variables to mirror the types of ACEs measured in the CDC-Kaiser study. However, we cannot address the developmental timing of these traumatic events nor can we address the frequency or severity of these ACEs. Certain variables were employed as proxies for certain sociodemographic measures as a formal assessment of socioeconomic status. In the future, greater precision in defining these sociodemographic measures might result in more accurate assessments of their contribution to ADHD risk.
We also used a single item as an indicator of homelessness that did not permit us to address issues of quality (living with a family member vs living in a shelter or car, vs sleeping on the street), the length of time the individual was homeless, or the developmental timing of homelessness. The number of times children experienced homelessness was also not evaluated despite our understanding that the life of a child who was homeless ten times throughout their childhood would likely present with differential pathology compared to children who were homeless once. These factors may be critically important in understanding the impact of homelessness on subsequent young adult ADHD.
Future Directions
Future research should address both resilience and risk in order to facilitate prevention efforts such that future interventions could be developed to facilitate prevention efforts against the adverse impact of ACEs and homelessness. To achieve this goal, acquiring additional contextual details concerning the nature, frequency, the severity of both the ACEs and homelessness, as well as the emotional responses to these adverse experiences would be valuable. Information about family structure and potential buffers would also aid our understanding of the pathogenic nature of these adversities and factors related to resilience. Future research designs directly addressing the causation of ADHD by ACEs and homelessness will have to consider the aforementioned collider effects. A prospective cohort study may avoid such biases by accrual and ascertainment of samples based upon two arms defined by housing condition. Well-powered samples accrued at specific developmental stages would inform more about the timing of ACEs, homelessness, and their impact. Furthermore, such research would benefit from structured diagnostic psychiatric assessments in order to not only fully characterize ADHD symptoms, but also assess comorbid psychopathology in order to validate the mental health outcomes.
Conclusion
This associational study found that some, but not all ACEs were associated with the risk of ADHD. However, three specific ACEs (sexual abuse, emotional abuse, and mental illness in the household) markedly increased risk of ADHD. The addition of homelessness and at least one of the high-risk ACEs yielded a 5.0-fold increase in ADHD risk. Given recent data suggesting that 2.5 million children or one in every 30 children are now homeless each year in the US [20], it is imperative that public health policies address this risk to the mental health and development of children. Furthermore, socioeconomic and health crises from the recent coronavirus pandemic have the potential to increase exposure to ACEs and homelessness nationwide [21]. Given such, the ascertainment of ACEs and homelessness need to be considered as part of the screening and diagnostic evaluation of patients presenting for treatment of ADHD.
Supplementary Materials
Supplementary Table 1: Derivation of Adverse Childhood Experiences Items Employed Based on CDC-Kaiser Permanente Study Using Add Health Measures
| CDC-Kaiser Permanente Study ACE Item | CDC-Kaiser Permanente Study ACE Item | |
|---|---|---|
| ACE 1: Emotional Abuse | “[Before your 18th birthday] A parent, stepparent, or adult living in your home swore at you, insulted you, put you down, or acted in a way that made you afraid that you might be physically hurt.” | “Before your 18th birthday, how often did a parent or other adult caregiver say things that really hurt your feelings or made you feel like you were not wanted or loved?” |
| ACE 2: Physical Abuse | “[Before your 18th birthday] A parent, stepparent, or adult living in your home pushed, grabbed, slapped, threw something at you, or hit you so hard that you had marks or were injured.” | “[Before your 18th birthday] A parent, stepparent, or adult living in your home pushed, grabbed, slapped, threw something at you, or hit you so hard that you had marks or were injured.” |
| ACE 3: Sexual Abuse | “[Before your 18th birthday] An adult, relative, family friend, or stranger who was at least 5 years older than you ever touched or fondled your body in a sexual way, made you touch his/her body in a sexual way, attempted to have any type of sexual intercourse with you.” | Any endorsed: “How old were you the first or only time this happened? [been forced, in a non-physical way, to have any type of sexual activity against your will]”-"How old were you the first or only time this happened? [been forced, in a physical way, to have any type of sexual activity against your will. "How old were you the first time one of your parents or other adult caregivers touched you in a sexual way, forced you to touch him or her in a sexual way, or forced you to have sexual relations?” |
| *ACE 4: Viewing Domestic Violence (*Not Employed in these analyses) | “[Before your 18th birthday] Your mother or stepmother was pushed, grabbed, slapped, had something thrown at her, kicked, bitten, hit with a fist, hit with something hard, repeatedly hit for over at least a few minutes, or ever threatened or hurt by a knife or gun by your father (or stepfather) or mother’s boyfriend.” | No Equivalent Item found in Add Health |
| ACE 5: Household Substance Abuse | “[Before your 18th birthday] A household member was a problem drinker or alcoholic or a household member used street drugs.” | Any endorsed: “Does biological mother currently have the following health problem: Alcoholism” “Does biological father currently have the following health problem: Alcoholism” |
| ACE 6: Mental illness or suicide in household | “[Before your 18th birthday] A household member was depressed or mentally ill or a household member attempted suicide” | Any endorsed: “Have any of your family members tried to kill themselves during the past 12 months?” “Have any of your family members tried to kill themselves during the past 12 months?” |
| ACE 7: Parental separation, divorce or death. | “[Before your 18th birthday] Your parents were ever separated or divorced.” | This was broadened in our analysis to also include the death of a parent. “Mother interview: What is your current marital status?” “How did it end?” “How old were you when she (biological mother) died?” “How old were you when he [biological father] died?” |
| ACE 8: Criminality and Incarceration in household | “[Before your 18th birthday] A household member went to prison?” | Any endorsed: How old were you when your [mother figure] went to jail or prison (the first time)? How old were you when your [father figure] went to jail or prison (the first time)? |
| ACE 9: Emotional Neglect | “[Before your 18th birthday] Someone in your family helped you feel important or special, you felt loved, people in your family looked out for each other and felt close to each other, and your family was a source of strength and support.” | “How much do you feel that your family pays attention to you?” |
| ACE 10: Physical Neglect | “[Before your 18th birthday] There was someone to take care of you, protect you, and take you to the doctor if you needed it, you didn’t have enough to eat, your parents were too drunk or too high to take care of you, and you had to wear dirty clothes.” | “[Before your 18th birthday] How often had your parents or other adult caregivers not taken care of your basic needs, such as keeping you clean or providing food or clothing?” |
Supplementary Data 1: Sensitivity Analysis for Sample Exclusion due to Self-reported “Dishonest” Responding: In this study, 1598 subjects were excluded because they reported to have responded dishonestly to the survey during Waves I and II. We conducted a sensitivity analysis of the impact of this exclusion. In comparing the self-reported “honest” and “dishonest” responders, we found that prevalence rates for ADHD and homelessness were lower among the “dishonest” responders, compared to their “honest” adolescent peers, i.e., 4.6% vs. 5.5% and 2.1% vs. 3.5%, respectively. This trend implied that the “dishonest” responders very likely misreported ADHD and homelessness. Similarly, those who self-reported “dishonest” responses, also had different ACE scores and educational level responses. This is noteworthy because these variables played critical roles in our analysis that estimated ADHD risk. When we added this “dishonest” responding sample back into full analytic sample and used a surrogate index variable to indicate whether their responses were “dishonest”, the relative risks of summed specific ACE scores being either 1 or 2 had ORs=1.7 and 1.8, thereby decreasing about 21% and 11% respectively compared to those estimated from the “honest” sample. In terms of the homelessness variable, the relative risk of homelessness was 2.1, and also decreased about 12%. Thus, those subjects who self-reported “dishonest” responses appeared to bias their responses downward, suggesting that their exclusion from the full analytic sample was justified.
Author Contributions: “Conceptualization, T.C., H.M., R.L., S.G., I.J., and D.D; methodology, S.G. and H.M.; software, S.G.; validation, S.G., and H.M..; formal analysis, S.G. and H.M..; investigation, T.C., H.M., R.L., S.G., I.J. and D.D..; writing - T.C., H.M., S.G., and D.D; .; writing-review and editing, T.C., H.M., R.L., S.G., I.J., and D.D; supervision, D.D..; All authors have read and agreed to the published version of the manuscript.
Funding: This research received no external funding.
Institutional Review Board Statement: Not applicable
Informed Consent Statement: Not applicable
Data Availability Statement: Information on how to obtain the Add Health data files is available on the Add Health website (https://addhealth.cpc.unc.edu/). No direct support was received from grant P01-HD31921 for this analysis.
Acknowledgments: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. This research uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill and funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations.
Conflicts of Interest: The authors declare no conflict of interest.
References
- Fredriksen M, Dahl AA, Martinsen EW, Klungsoyr O, Faraone SV, et al. (2014) Childhood and persistent ADHD symptoms associated with educational failure and long-term occupational disability in adult ADHD. Atten Defic Hyperact Disord. 6(2): 87-99. [PubMed.]
- Biederman J, Petty CR, Fried R, Kaiser R, Dolan CR, et al. (2008) Educational and occupational under attainment in adults with attention-deficit/hyperactivity disorder: a controlled study. J Clin Psychiatry. 69: 1217-1222. [PubMed.]
- Cabral MDI, Liu S, Soares N. (2020) Attention-deficit/hyperactivity disorder: diagnostic criteria, epidemiology, risk factors and evaluation in youth. Transl Pediatr. 9(Suppl 1): S104-S113. [PubMed.]
- Thomas R, Sanders S, Doust J, Beller E, Glasziou P. (2015) Prevalence of attention deficit/ hyperactivity disorder: A systematic review and meta-analysis. Pediatrics. 135(4): e994-e1001. [PubMed.]
- Sayal K, Prasad V, Daley D, Ford T, Coghill D. (2018) ADHD in children and young people: prevalence, care pathways, and service provision. The lancet. Psychiatry. 5(2): 175-186. [PubMed.]
- Polanczyk GV, Willcutt EG, Salum GA, Kieling C, Rohde LA. (2014) ADHD prevalence estimates across three decades: an updated systematic review and meta-regression analysis. International journal of epidemiology. 43(2): 434-442. [PubMed.]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, et al. (1998) Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. American journal of preventive medicine. 14(4): 245-258. [PubMed.]
- Brown NM, Brown SN, Briggs RD, Germán M, Belamarich PF, et al. (2017) Associations Between Adverse Childhood Experiences and ADHD Diagnosis and Severity. Acad Pediatr. 17(4): 349-355. [PubMed.]
- Jimenez ME, Wade R, Schwartz-Soicher O, Lin Y, Reichman NE. (2017) Adverse Childhood Experiences and ADHD Diagnosis at Age 9 Years in a National Urban Sample. Acad Pediatr. 17(4): 356-361. [PubMed.]
- Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, et al. (2017) The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health. 2(8): e356-e366. [PubMed.]
- Radcliff E, Crouch E, Strompolis M, Srivastav A. (2019) Homelessness in Childhood and Adverse Childhood Experiences (ACEs). Maternal and child health journal. 23(6): 811-820. [PubMed.]
- Liu M, Mejia-Lancheros C, Lachaud J, et al. (2020) Resilience and adverse childhood experiences: associations with poor mental health among homeless adults. AJPM. 58(6): 807-816. [PubMed.]
- Klein JD. (1997) The National Longitudinal Study of Adolescent Health: Preliminary Results: Great Expectations. JAMA. 864-865. [PubMed.]
- Chen P, Chantala K. (2014) Guidelines for analyzing Add Health data. Carolina Population Center, University of North Carolina at Chapel Hill. 710. [Ref.]
- Herzog JI, Schmahl C. (2018) Adverse Childhood Experiences and the Consequences on Neurobiological, Psychosocial, and Somatic Conditions Across the Lifespan. Front Psychiatry. 9: 420. [Ref.]
- Linares LO, Li M, Shrout PE, et al. (2010) The course of inattention and hyperactivity/impulsivity symptoms after foster placement. Paediatrics. 125: e489-e498. [PubMed.]
- Ford JD, Rascusin CGE, Daviss JR, Fleisher A, Thomas J. (2000) Child maltreatment, other trauma exposure, and posttraumatic symptomatology among children with oppositional defiant and attention deficit hyperactivity disorders. Child Maltreatment. 5: 205-217. [PubMed.]
- Holland PW. (1986) Statistics and causal inference. JASA. 81(396): 945-960. [Ref.]
- Luque-Fernandez MA, et al. (2019) Educational note: paradoxical collider effect in the analysis of non-communicable disease epidemiological data: a reproducible illustration and web application. Int J. Epidemiol. 48: 640-653. [PubMed.]
- SAMHSA. (2022) Child Homelessness: A Growing Crisis. Left side footer content. SAMHSA. [Ref.]
- Bryant DJ, Oo M, Damian AJ. (2020) The rise of adverse childhood experiences during the COVID 19 pandemic. Psychol Trauma. 12(S1): S193-S194. [PubMed.]