>Corresponding Author : Matanda Kapend Serge
>Article Type : Research Article
>Volume : 3 | Issue : 1
>Received Date : 18 Aug, 2023
>Accepted Date : 04 Sep, 2023
>Published Date : 14 Sep, 2023
>DOI : https://doi.org/10.54289/JVVD2300102
>Citation : Serge MK, Michel KN, Eric K, Josephine MK, Christian KN, et al. (2023) HIV, HBV Infections and HIV-HBV Coinfection in Lubumbashi: 6 Years Follow-Up of Prevalence (2016 To 2021). J Virol Viral Dis 3(1): doi https://doi.org/10.54289/JVVD2300102
>Copyright : © 2023 Serge MK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Research Article | Open Access
1Medical teaching hospital of Lubumbashi, internal medicine department, university of Lubumbashi
2Public health department, University of Kamina
3HIV/AIDS unit, molecular biology, school of medicine, university of Kinshasa
4Medical teaching hospital of Lubumbashi, pediatrics department, university of Lubumbashi
5Medical teaching hospital of Lubumbashi, immunology laboratory university of Lubumbashi
6Blood transfusion program of Lubumbashi
7Sendwe Hospital, immunology laboratory
8Medical teaching hospital of Kinshasa, infectious diseases and tropical medicine department, university of Kinshasa
*Corresponding author: Matanda Kapend Serge, Medical teaching hospital of Lubumbashi, internal medicine department, university of Lubumbashi
Abbreviations: WHO: World Health Organization, HIV: Human Immunodeficiency Virus, HBV: Hepatitis B Virus, DRC: Democratic Republic of Congo
Introduction
For World Health Organization (WHO), hepatitis B elimination as a public health threat by 2030 is one of his most priorities. In 2015, 257 million of people worldwide were infected by this virus (representing 3% of world population) [1].
More recently discovered the human immunodeficiency virus (HIV) infection is also a public health threat. In 2019, 37,9 million of people were affected worldwide. The WHO has also planned its elimination as threat by 2030.
Those two infections are particularly frequent in Africa region. Most infected persons by hepatitis B are in Africa and west pacific region where there is 68% of all infected persons.
Almost the same portion of infected persons (67,8%) live in the south part of Africa [2].
The WHO reported that 2,7 millions of persons were coinfected by both HIV and hepatitis B virus (HBV) viruses in 2015 [1]. For those persons there is an increased of morbidity due to interaction of viruses.
The HIV-HBV coinfection has some particularities: reactivation of HBV infection in severe immunodepression for persons with HBs (antibodies+/ HBc+ antibodies) [3] and for those with HBs negative Antigen, more rapid evolution to cirrhosis, less efficacity for vaccination related to the drop in T CD4 lymphocytes.
Thus, the WHO has involved countries in a common battle against those pandemic diseases during international assemblies.
Some countries implemented programs of elimination of those 2 infections particularly hepatitis B and are reaching their goals years after years. In Democratic Republic of Congo (DRC) nothing has been done yet in the scale of the country for elimination of hepatitis B infection. Thus, nothing of good can be expected in this battle to hope better control of this specific infection. It appears urgent that something must be done urgently in the whole country.
Unless need of controlling the prevalence, the spread of this infection by survey is important to focus on specific situation from collected data.
The aim of this study is to evaluate prevalence evolution of HIV, HBV infections and HIV-HBV coinfection in Lubumbashi for 6 years.
Specifically, to search for correlation between those infections and age, sex, site of blood collection in Lubumbashi.
Method
Design of the study and period
The study is annual retrospective review of cases of HIV, HBV, and HIV-HBV coinfections from 2016 to 2021.
Sites of study
Three sites were chosen considering the quality of data conservation and completion. There were those of transfusion programs.
Two of them are hospital sites, one was mobile during caravan of collection of blood by donors.
Study population
Persons were included from those living in Lubumbashi town or those who has reached the mobile caravan of blood donation in this town by the time of collection.
Sample size and selection of cases
The selected people were blood donors aged from 16 years and above. They have donated or tried to during the period of study. Those from which important data such as name or specific serologic results were not included.
Study variables
Social and demographic
• Age (by year and categorized by decades and by 50 years). Expressed by its median and limits.
• Gender: expressed in two categories: female and male
• Origin: into two categories (persons living in Lubumbashi and those from out of Lubumbashi)
Type of donors: paid and unpaid donors
Site of blood collection: hospital or mobile
Prevalence calculated by amount of cases/population of donors) *100 (expressed in percentage)
Biological variables: HBs surface antigen of hepatitis B virus detected by Wondfo® rapid test (Sensitivity of 97.3% and specificity of 99.2%) on whole blood collected and tested immediately.
HIV antibodies detected by combination of Determine® and Unigold® tests. (Sensitivity of 99.76% and specificity of 99.85%) on whole blood collected a few minutes before examination.
These 2 detections led to define HBV infected persons, HIV infected persons and coinfected HIV-HBV
Data analysis
Descriptive analysis: Qualitative variables (sex, origin, site of collection, nature of infection) were “dichotomized” and presented by proportions.
Age as variable was classified in groups of decades first and in groups of 50 years. Those groups were used as qualitative variables for comparison. The median of age was calculated and presented with the limits of distribution.
Annual prevalence of infections (in percentage) was showed on a curve which allowed to see the trend of the two infections and coinfection for 6 years.
Comparative statistics: Data expressed by categories were compared using chi squared test with confidence interval of 95%. The significant statistic difference considered was inferior to 0,05. When the expected values were less than 5 the Fisher test were used with the same confidence interval of 95%.
The risk of being infected by any virus according to gender was evaluated by odds ratio with confidence interval of 95%.
Ethical considerations
Results are presented anonymously. This study is part of a general study that have been approved by medical ethical committee of Lubumbashi with the reference UNILU/CEM/114/2022.
Conflict of interest
There is no conflict of interest on this study.
Results And Discussion
The study included 12492 donors of hospitals and mobile site.
The table 1 shows their general characteristics.
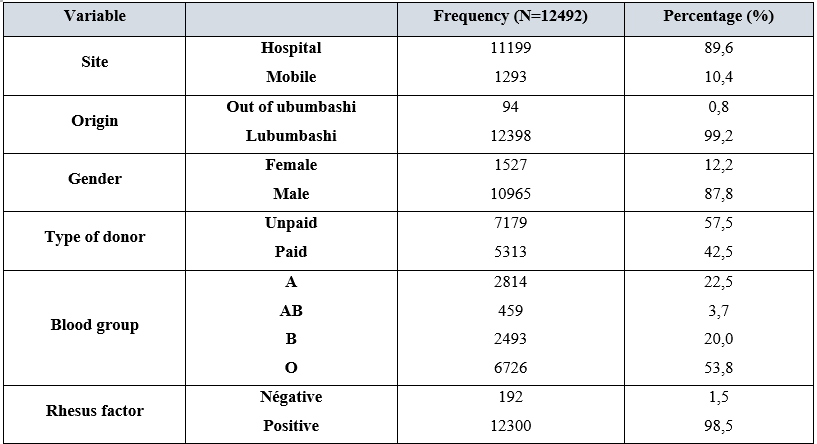
Table 1. General characteristics of blood donors
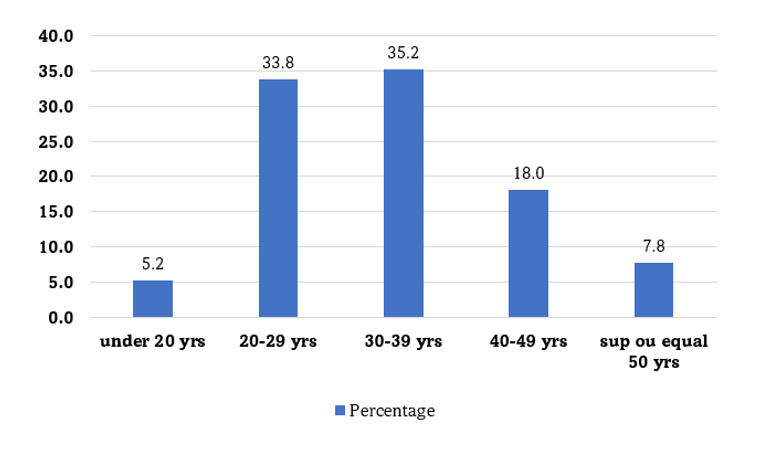
Figure 1: Proportions of donors grouped by decades
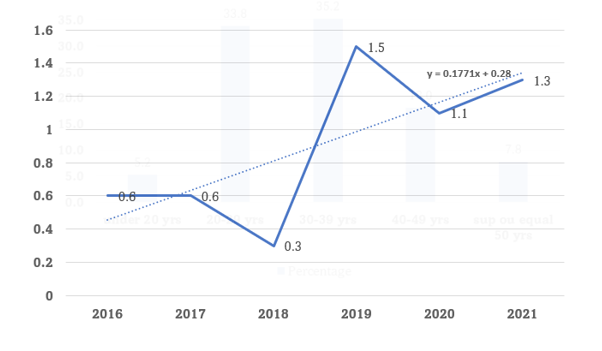
Figure 2: Prevalence of HIV cases
The HIV prevalence varied between 0,6 and 1,5% on the figure above. The HBV prevalence varied between 2,5 and 5% (seen on the figure 3).
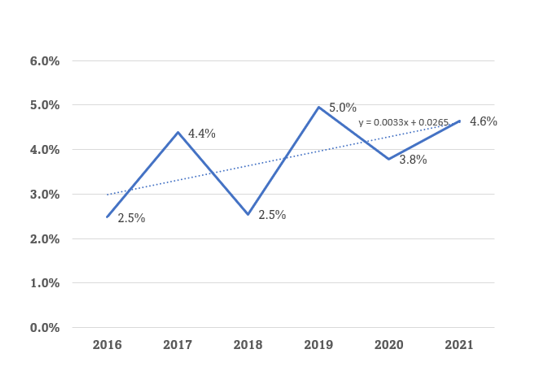
Figure 3: Prevalence of HBV cases during the 6 years of follow up
Population of donors involved in the study were recruited mostly in hospital facilities (table 1). In Lubumbashi, like in Democratic Republic of Congo generally, hospitals are principal place people can be tested and were dealing with blood products can be possible. In facts there is less mobile donor recruitment campaigns partially due to less funds committed for it.
Most people live in Lubumbashi and a few (0,8%) were there transiently and participated in the study (table 1).
Men donates more than women like noticed in previous studies in Lubumbashi [4,5], and in D R Congo generally [6-8]. The reason might be the conception of responsibility in the country to place men before when comes to take medical decisions at hospital and that for mobile blood campaigns to leave women at home while men can move to those caravans. In a neighborhood country (Cameroon) men are also the most donors at an approximate ratio of 4/1 for men [9] and in a northern country of Africa (Tunisia) [10]. In Brazil the trend is different at some places where women are most donor [11].
The study shows that remunerated donors are less represented than voluntary donors who were composed of familiar donors and benevolent donors (table 1). However, the difference is not that great in proportion between the two categories.
The ABO blood group was predominantly O (table 1) like seen in central African country like Cameroon [12] or of neighboring region like in Burkina Fasso [13].
When grouping the donors in two groups of 50 years of age the distribution shows that there were more of them under 50 years, (table 2).
The median age was 32 years. Most of patients (92,27%) had less than 50 years of age, especially between 20 and 39 years, a young population.
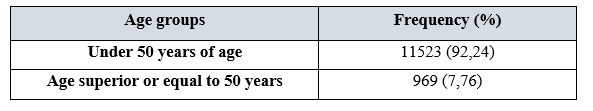
Table 2: Donors grouped on two groups of 50 years of age
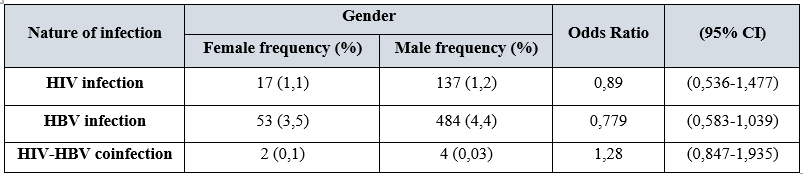
Table 3: Risk of HIV, HBV infections and HIV-HBV coinfections by gender
No gender is more exposed to one of the 3 situations.
Prevalences
Reports about DR Congo estimated the overall prevalence of HIV infection in 2014 around 1,2% where predominantly women were affected. Since there politics has changed worldwide through WHO impulse. In DR Congo too new strategies are used to promote more access to care facilities and treatment to low the morbidity and contaminations. In this study we can see that before 2019 HIV prevalence is lower than 1%. From 2019 with the burden of covid-19 infection we can see a rise of prevalence reaching values of 1,5% in Lubumbashi (figure 1). This event has led local organizations to adapt their strategies of care, keeping patients on treatment and sustain efforts of lowering impact of HIV infection. Those strategies took time to take place while patients were still living in society with all consequences on possible spreading the infection. This may explain the rise of prevalence but must be considered with some caution.
One of the WHO goals by 2030 is to eliminate hepatitis B infection as a health threat worldwide. Thus, all countries has to conjugate efforts to achieve that. Some have seriously improved their results like United State of America: from 2017 there was approximately 22000 new infections per year, they then targeted to reduce by at least 20% per year new hepatitis B infections. Results was better than expected because from a baseline of 22 200 new infections they reach 14 000 new infections in 2020 while were expected 20 100 the same year and 18 000 in 2025 [14]. The USA prevalence of chronic hepatitis B infection was 0,35% in 2016 [15] and should have decreased actually according to state Implication mentioned above.
Previous studies of prevalence in DR Congo in different areas has estimated at 3,7% (in Bukavu), 4,2% (in the east part of the country) and one at 3,3% for a global estimation of all Congolese population [16]. In Lubumbashi there has been different several studies with high estimated prevalence like 17,3% in 2014 [17], 8% in 2015 [18], for the biggest ones. This study, which has an advantage of following for 6 years, reveals a prevalence ranging between 2,5 and 5% and median prevalence of 4,3% (figure 3). This is closely related to a recent global estimation of the country [16].
The current estimation shows the relative constancy of the prevalence which remains one of the highest of the world.
With extrapolation to general population of Lubumbashi according to last estimation of populations of cities worldwide [19] there must be 91 200 persons infected by HBV for a total population of 2 281 000. This is supposed to be number of persons who must be taken into care facilities and followed up. This is unfortunately far from reality because no program yet has been put in place and just isolated initiatives of health workers.
Both infections (HIV and HBV prevalence) when associated leads to greater morbidity on infected people. Among HIV infected people 7,4% are infected by VHB also [1] making the HIV-HBV coinfection having a low prevalence comparing to the 2 infections separately but with a greater potential on morbidity and mortality without antiretroviral treatment. This study shows a prevalence ranging from 0 to 0,066% with a median of 0,05% (figure 4). This looks low reported to total population but considering the HIV infected persons it represents almost 4% of this last group.
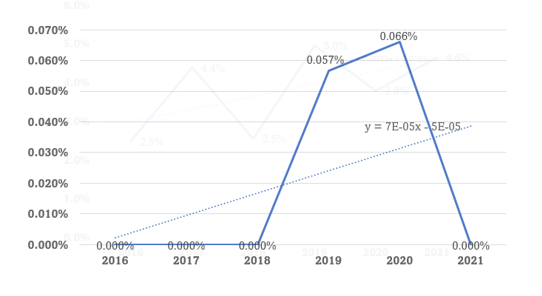
Figure 4: Annual evolution of HIV-HBV coinfection from 2016 to 2021
Evaluation of the mean prevalence of the 3 situations is seen on the figure 5.
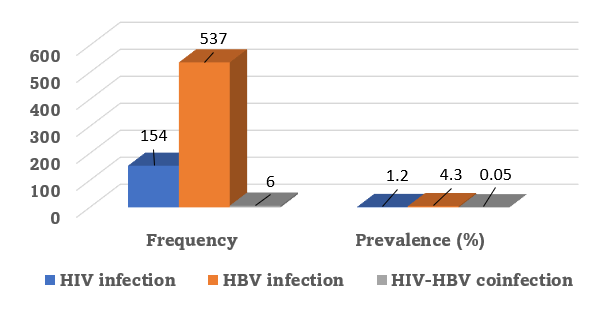
Figure 5: Mean prevalence of HIV, HBV infections and the HIV-HBV coinfection
When we report this number to general population of Lubumbashi, we can expect around 1 140 coinfected persons.
From other place of Africa which is the continent with 70% of coinfected people, higher prevalence are seen in Ghana with 13,6% [20], 9,5% in Zambia [21].
Group comparisons
The study shows a difference between prevalence of HIV and HBV in the sites. More people from hospital facilities than mobile facilities are infected by the 2 viruses. But when comes the coinfection there is no difference (figure 6). What can explain the difference? It’s hard to tell from now.
Between sites of blood collection
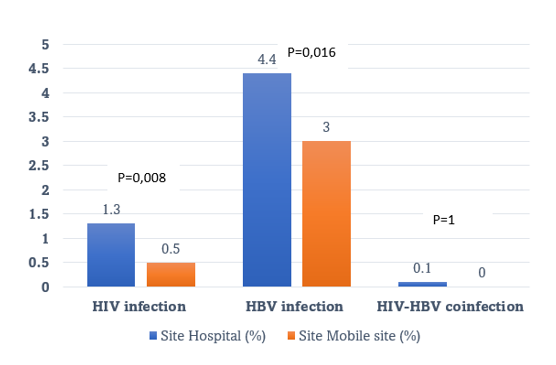
Figure 6: Comparison of prevalence of infections from the different sites
Between age groups
From the results of this study, we can also notice that people over 50 years are more infected by the 2 viruses individually (table 4). Can we have a reason of hope when we know that HBV vaccine has been introduced recently and that young population seems to be less infected? Not sure because we experiment only …years of vaccination at large scale. Can we also have a reason of hope when HBV infections are carried by mother to baby routes and that younger people are less concerned by the infection? Not sure also because of the great population of Lubumbashi. Coinfection is equally represented between the group of age (table 4).
Risk from gender
Gender is not a risk factor of getting infected neither by HIV nor by HBV from this study results. There is no trend too by HIV-HBV coinfection (table 5).
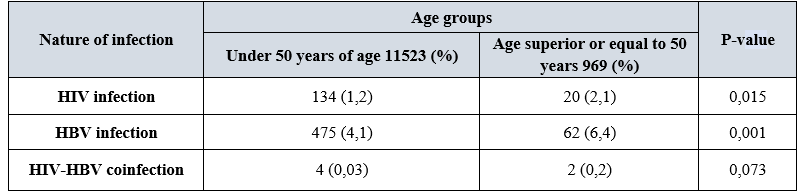
Table 4: Comparison of prevalence of infections between the groups of 50 years of age
Correlation is seen between the two groups of age and infections considered individually.
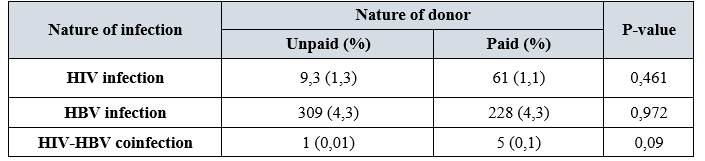
Table 5: Comparison of prevalence of infections with nature of donors
Conclusion
From the 6 years of survey, HIV prevalence of Lubumbashi raised from 0,6 to more than 1% after the burden of covid-19. The prevalence of HBV chronic infection remains one of the highest with 4,3% while HIV-HBV coinfection is less than world mean estimation.
Trends of repartition is predominantly on aged people and those who reached hospital facilities for HIV and HBV infections.
This constant situation of HBV prevalence will not allow the RD Congo to fill the WHO goals because RD Congo still have high prevalence of HBV infection.
References:
- Agyeman AA and Ofori-Asenso R. (2016) ‘Prevalence of HIV and hepatitis B coinfection in Ghana: a systematic review and meta-analysis.’ AIDS research and therapy. 13:23. [PubMed.]
- Batina A, Kabemba S and Malengela R. (2007) Infectious markers among blood donors in Democratic Republic of Congo ( DRC ). 145-149. [PubMed.]
- Clark SJ, et al. (2006) Reactivation of latent hepatitis B virus infection with HIV-related immunosuppression., International journal of STD AIDS. 17(1): 67-69. [PubMed.]
- Kabamba AT, et al. (2021) ‘Epidemiological aspects and molecular characterization of the hepatitis B virus among blood donors in Lubumbashi, Democratic Republic of Congo’. Transfusion Clinique et Biologique. 28(1): 30-37. [PubMed.]
- Kakisingi CN, et al. (2016) ‘Profil épidémiologique et séroprévalence des donneurs de sang aux cliniques universitaires de Lubumbashi, République Démocratique du Congo’, Pan Afr Med J. PAMJ - African Field Epidemiology Network. 23(175). [Ref.]
- Kakisingi CN, et al. (2016) ‘Profil épidémiologique et séroprévalence des donneurs de sang aux cliniques universitaires de Lubumbashi, République Démocratique du Congo’. Pan African Medical Journal. 23(175):1-9. [Ref.]
- Katamba C, Chungu T and Lusale C. (2013) ‘Motivation and sociology of blood donors in Tunisia: Reality and perspectives’. Transfusion Clinique et Biologique. 469-475. [PubMed.]
- Katamba C, Chungu T and Lusale C. (2020) ‘HIV, syphilis and hepatitis B coinfections in Mkushi, Zambia: A cross-sectional study’. F1000Research. 8: 562. [Ref.]
- Michel KN. (2015) ‘HIV and HBV Seroprevalence in Volunteer Blood Donors in Lubumbashi’. SOJ Immunology. 3(5): 1-3. [Ref.]
- Mudji J, Malala J and Horsmans Y. (2021) ‘Seroprevalence of viral hepatitis B and C in two populations: blood donors and patients with suspected hepatic cirrhosis in Kwilu province. Democratic Republic of Congo’. International Journal of Infectious Diseases. 110: 222-225. [Ref.]
- Ndoula ST, et al. (2014) ‘Phenotypic and allelic distribution of the ABO and Rhesus (D) blood groups in the Cameroonian population. International journal of immunogenetics. 41(3): 206-210. [PubMed.]
- Nguyen MH, et al. (2020) ‘Hepatitis B virus: Advances in prevention, diagnosis, and therapy’. Clinical Microbiology Reviews. 33(2): e00046-19. [PubMed.]
- Noubiap JJN, et al. (2013) ‘Sero-epidemiology of human immunodeficiency virus, hepatitis B and C viruses, and syphilis infections among first-time blood donors in Edéa, Cameroon’. International Journal of Infectious Diseases. 17(10): 832-837. [PubMed.]
- Prevention C. (2022) ‘Progress Toward Viral Hepatitis Elimination in the United States, 2022. [Ref.]
- Sawadogo S, et al. (2019) ‘Distribution of ABO and RHD blood group antigens in blood donors in Burkina Faso. International journal of immunogenetics. 46(1): 1-6. [PubMed.]
- Situakibanza N, Sisa B, Mbuyi R, Kiazayawoko Z, et al. (2017) ‘Taux de séroprévalence des marqueurs viraux (VIH/VHB/VHC) chez les donneurs du sang au Centre Provincial de Transfusion Sanguine de Matadi, Province du Kongo-Central, RD Congo Seroprevalence rate of viral markers (HIV / HBV / HCV) in blood donors at the M’. Ann. afr. méd. [Ref.]
- Thompson P, et al. (2019) ‘Seroepidemiology of hepatitis B in the Democratic Republic of the Congo’, American Journal of Tropical Medicine and Hygiene. 101(1): 226-229. [Ref.]
- UNAIDS. (2019) ‘Global HIV and AIDS statistics 2019 Fact sheet’, Global HIV and AIDs ststistics, World AIDS day 2019 Fact Sheet. 1: 1-6. [Ref.]
- United Nations D and of Economic and Social Affairs, PD. (2018) ‘The World’s Cities in 2018’, World Urbanization Prospects: The 2018 Revision. 34. [Ref.]
- World Health Organization. (2017) Global hepatitis report. 2017. [Ref.]
- Zucoloto ML, et al. (2019) ‘Comparison of the demographic and social profile of blood donors and nondonors in Brazil’. Health and Social Care in the Community. 330-336. [PubMed.]